Fill Out Your Sbar Word Form
The SBAR Word form is an essential communication tool that streamlines the process of reporting critical issues within healthcare settings. Originally developed by Kaiser Permanente, the SBAR technique stands for Situation, Background, Assessment, and Recommendation, each component serving a distinct purpose in gathering and presenting vital information. When applying this framework, users begin by outlining the current situation, clearly identifying themselves, their role, and detailing the issue at hand, including its severity and onset. Context is then provided through the background section, where relevant historical data, existing conditions, and applicable national standards or policies are summarized. Following this, a thorough assessment evaluates the situation based on established norms and identifies any areas where compliance is lacking. Finally, users conclude by making specific recommendations that propose actionable steps to address the issues raised. By leveraging the SBAR Word form, healthcare professionals can effectively communicate concerns, ensuring that information is conveyed efficiently and that timely actions are taken to enhance patient care and organizational function.
Sbar Word Example
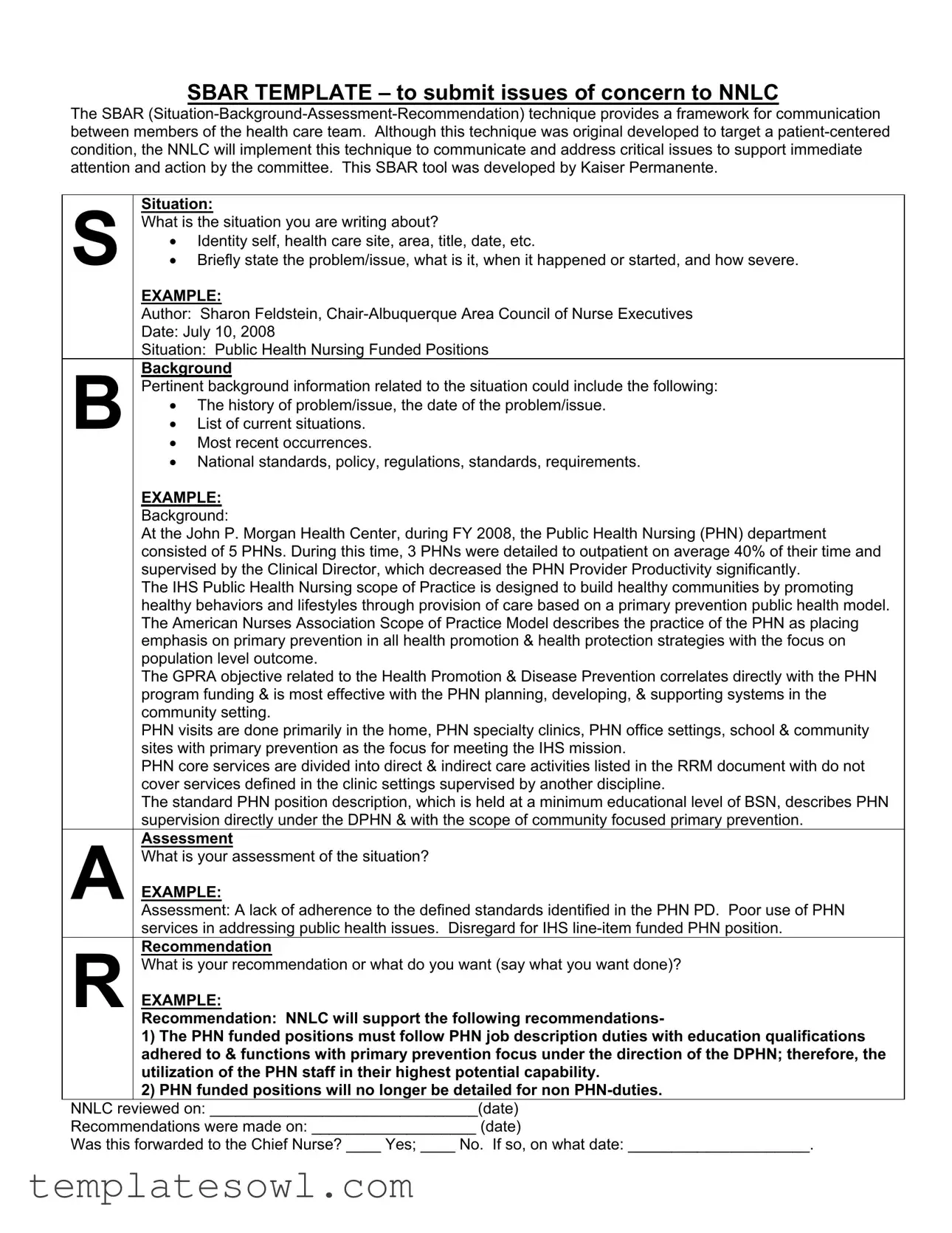
SBAR TEMPLATE – to submit issues of concern to NNLC
The SBAR
Situation:
SWhat is the situation you are writing about?
•Identity self, health care site, area, title, date, etc.
•Briefly state the problem/issue, what is it, when it happened or started, and how severe.
EXAMPLE:
Author: Sharon Feldstein,
Date: July 10, 2008
Situation: Public Health Nursing Funded Positions
Background
BPertinent background information related to the situation could include the following:
•The history of problem/issue, the date of the problem/issue.
•List of current situations.
•Most recent occurrences.
•National standards, policy, regulations, standards, requirements.
EXAMPLE:
Background:
At the John P. Morgan Health Center, during FY 2008, the Public Health Nursing (PHN) department consisted of 5 PHNs. During this time, 3 PHNs were detailed to outpatient on average 40% of their time and supervised by the Clinical Director, which decreased the PHN Provider Productivity significantly.
The IHS Public Health Nursing scope of Practice is designed to build healthy communities by promoting healthy behaviors and lifestyles through provision of care based on a primary prevention public health model. The American Nurses Association Scope of Practice Model describes the practice of the PHN as placing emphasis on primary prevention in all health promotion & health protection strategies with the focus on population level outcome.
The GPRA objective related to the Health Promotion & Disease Prevention correlates directly with the PHN program funding & is most effective with the PHN planning, developing, & supporting systems in the community setting.
PHN visits are done primarily in the home, PHN specialty clinics, PHN office settings, school & community sites with primary prevention as the focus for meeting the IHS mission.
PHN core services are divided into direct & indirect care activities listed in the RRM document with do not cover services defined in the clinic settings supervised by another discipline.
The standard PHN position description, which is held at a minimum educational level of BSN, describes PHN supervision directly under the DPHN & with the scope of community focused primary prevention.
Assessment
AWhat is your assessment of the situation?
EXAMPLE:
Assessment: A lack of adherence to the defined standards identified in the PHN PD. Poor use of PHN services in addressing public health issues. Disregard for IHS
Recommendation
RWhat is your recommendation or what do you want (say what you want done)?
EXAMPLE:
Recommendation: NNLC will support the following recommendations-
1)The PHN funded positions must follow PHN job description duties with education qualifications adhered to & functions with primary prevention focus under the direction of the DPHN; therefore, the utilization of the PHN staff in their highest potential capability.
2)PHN funded positions will no longer be detailed for non
NNLC reviewed on: _______________________________(date)
Recommendations were made on: ___________________ (date)
Was this forwarded to the Chief Nurse? ____ Yes; ____ No. If so, on what date: _____________________.
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose of SBAR | The SBAR technique (Situation-Background-Assessment-Recommendation) serves as an effective communication framework among healthcare team members to address critical issues requiring immediate attention. |
| Origin of SBAR | This tool was originally developed by Kaiser Permanente to enhance patient-centered communication but has been adapted by the NNLC for broader applications in healthcare settings. |
| Components of SBAR | The SBAR format includes four essential sections: Situation (describe the issue), Background (provide relevant history), Assessment (evaluate the current state), and Recommendation (suggest actions to be taken). |
| Implementation | As per NNLC guidelines, SBAR should be utilized by healthcare professionals to ensure that all communications about critical issues follow a clear and structured format to promote effective resolution. |
Guidelines on Utilizing Sbar Word
To complete the SBAR Word form, gather all necessary information about the situation you wish to report. Follow the steps carefully to ensure you provide a comprehensive overview for effective communication. Once the form is filled out, it can be submitted for review and action by the relevant committee.
- Open the SBAR Word form.
- Fill in the situation section:
- State your identity, health care site, title, and date.
- Briefly describe the problem or issue, including when it started and its severity.
- Complete the background section:
- Provide pertinent background information regarding the situation.
- Include the history of the issue and current situations.
- Mention any relevant national standards, policies, or regulations.
- Enter your assessment:
- Clearly outline your evaluation of the situation.
- Make your recommendation:
- State what you want done regarding the situation.
- List any specific actions or changes you recommend.
- Fill in the review and follow-up sections:
- Document the date the SBAR was reviewed.
- Record the date recommendations were made.
- Indicate whether the issue was forwarded to the Chief Nurse, including the date if applicable.
What You Should Know About This Form
What is the SBAR Word form?
The SBAR Word form is a structured communication tool designed to facilitate effective information sharing among healthcare professionals. It breaks down information into four key components: Situation, Background, Assessment, and Recommendation. Each element helps to ensure that all relevant details are captured and communicated clearly, ultimately supporting more efficient decision-making and problem-solving within health-related issues.
How do I use the SBAR Word form?
To use the SBAR Word form, begin by clearly identifying the situation you are addressing. Include essential details such as your identity, the healthcare site, and a brief statement of the issue. Next, provide background information that outlines previous occurrences and relevant standards or policies. Follow this with your assessment, describing your analysis of the situation, and conclude with specific recommendations for action. This structured approach clarifies communication and fosters collaboration among team members.
Who developed the SBAR tool?
The SBAR tool was originally developed by Kaiser Permanente. It was designed to improve communication in healthcare settings, emphasizing a systematic method for conveying critical information. By using this method, healthcare teams can improve their response to situations that require immediate attention, thereby enhancing patient care and operational efficiency.
What types of situations can the SBAR form address?
The SBAR form can be utilized to address a variety of situations within healthcare settings. It is particularly effective for reporting issues such as staff shortages, inadequate resources, safety concerns, and compliance with established regulations. By clearly outlining each component of the SBAR framework, healthcare professionals can ensure that pressing issues receive the necessary attention and intervention.
Is the SBAR form specific to any healthcare team?
While the SBAR format can be adapted for various healthcare teams, the NNLC has specifically implemented this technique to address critical issues that require committee review and action. This tailored use promotes focused communication within the NNLC while maintaining the form’s general applicability across different health organizations and contexts.
Can I modify the SBAR form for my needs?
Absolutely. While the SBAR form follows a structured format, it can be adapted to suit the needs of different healthcare settings or situations. Feel free to modify the template to include relevant details specific to your context. The key is to maintain clarity and ensure that all essential components—situation, background, assessment, and recommendation—are addressed.
How does the SBAR format improve communication?
The SBAR format enhances communication by providing a clear and organized way to present information. It decreases the chances of misunderstandings because it prompts users to provide concise and relevant details. This systematic approach helps healthcare professionals quickly assess the situation and make informed decisions, leading to better outcomes for patients and the healthcare team.
What should I do with the completed SBAR form?
Once you have completed the SBAR form, it’s crucial to share it with the relevant parties, such as team members or decision-makers within your organization. In the case outlined in the form, forwarding it to the Chief Nurse is recommended. Recording the dates when the recommendations were made and when the form was viewed allows for better tracking and accountability in addressing the cited issues.
Is training required to use the SBAR tool effectively?
While formal training can be beneficial in maximizing the effectiveness of the SBAR tool, it is not mandatory. Many healthcare professionals can grasp the basics of the framework quickly. Understanding the purpose and structure of each SBAR component can help users communicate concerns more effectively, which ultimately leads to improved collaboration among healthcare teams.
Common mistakes
When filling out the SBAR Word form, many people make critical mistakes that can lead to confusion or inadequate communication. One common error is failing to clearly identify the subject of the situation. Individuals often neglect to specify who they are and which health care site they represent. This information is crucial for context and should appear at the beginning of the situation statement.
Another frequent mistake is providing an incomplete background. The background section should include relevant history and details about the issue at hand. Simply stating the problem without context leaves the reader in the dark. It is essential to include dates, recent occurrences, and any national standards related to the issue to ensure comprehensive understanding.
In the assessment portion, many users fail to present a coherent evaluation of the situation. It's vital to provide a clear analysis based on the provided context. Vague language or generalizations detract from the effectiveness of the assessment. Specific details highlight the severity of the issue and the impact it has on patient care.
Recommendations often fall short as well. Individuals tend to offer too vague suggestions instead of actionable steps. Effective recommendations should clearly outline what needs to be done, who should do it, and when it should be accomplished. This level of detail allows for accountability and follow-through.
Additionally, users commonly skip the section that confirms whether the issue was forwarded to the Chief Nurse, which may hinder escalation of the problem. This step is crucial for ensuring that the right individuals are aware of the situation and can take appropriate action.
Finally, not maintaining timeliness can lead to missed opportunities for intervention. Filling out the form weeks after the incident loses its urgency. Submitting the SBAR promptly after the situation arises promotes timely communication and action within the health care team.
Documents used along the form
In the process of communicating critical healthcare issues, several documents complement the SBAR Word form. Each serves a unique purpose, aiming to enhance clarity and facilitate effective communication among team members. Below is a list of these documents, along with brief descriptions of their functions.
- Incident Report - This document is used to formally record any unexpected events or accidents that occur within a healthcare setting. It includes details about what happened, factors contributing to the incident, and immediate actions taken. Incident reports are crucial for identifying trends and improving safety protocols.
- Patient Care Report - This report provides a detailed account of a patient’s interaction with healthcare services. It includes information on assessments, interventions, and outcomes, allowing for continuity of care. This document is often shared among healthcare team members to ensure everyone is informed.
- Meeting Minutes - Meeting minutes offer a written record of discussions, decisions, and action items from team meetings. They ensure transparency and accountability by documenting what was agreed upon and who is responsible for follow-up actions.
- Referral Form - Used to formally refer a patient to another healthcare provider or service, this form includes essential patient information, reasons for the referral, and any pertinent medical history. It ensures a smooth transition of care and helps avoid gaps in treatment.
By utilizing these forms alongside the SBAR Word form, healthcare professionals can enhance communication, promote safety, and improve patient outcomes. Each document plays a vital role in ensuring issues are addressed promptly and adequately within the healthcare environment.
Similar forms
- SOAP Note: The SOAP (Subjective, Objective, Assessment, Plan) notes are used in healthcare to document patient information. Just like the SBAR form, it organizes information clearly, helping health professionals communicate about patient care effectively. The structure is similar in that both focus on gathering and presenting critical information systematically.
- PIE Note: The PIE (Problem, Intervention, Evaluation) note shares a common goal with SBAR in providing a clear communication method among medical staff. Both formats help in identifying issues and discussing their management, enabling focused discussions around patient care or operational concerns.
- CHEAT Sheet: A CHEAT (Charting, History, Evaluation, Assessment, Treatment) sheet organizes patient information for quick reference. Similarly, the SBAR framework breaks down important elements of a situation into manageable sections, facilitating effective communication and quicker decision-making within teams.
- Handoff Report: Often used during shift changes, the handoff report supplies relevant patient information to the incoming care team. Like SBAR, it emphasizes clear and concise communication, aiming to ensure continuity of care by outlining necessary details and concerns.
- Incident Report: This document captures details about an event that requires attention, such as an error or an accident. Similar to SBAR’s outline, an incident report organizes significant information to support understanding and future preventive measures, making it easier for teams to address potential improvements.
Dos and Don'ts
When filling out the SBAR Word form, follow these guidelines for a more effective submission:
- Do clearly identify yourself. Include your name, title, health care site, and date.
- Do state the problem succinctly. Describe what the issue is, when it started, and its severity in straightforward terms.
- Do provide relevant background. Include historical context and current situations that pertain to the issue at hand.
- Do assess the situation logically. Explain your evaluation of the circumstances based on the information provided.
- Don't use excessive jargon. Keep language simple and accessible to ensure clarity for all readers.
- Don't omit recommendations. Be clear about what actions you want taken and provide specific suggestions for improvement.
Misconceptions
The SBAR (Situation-Background-Assessment-Recommendation) form is a valuable tool for effective communication within healthcare settings. However, misconceptions can lead to misunderstandings of its purpose and use. Here are nine common misconceptions about the SBAR Word form:
- SBAR is only for urgent situations. Many believe SBAR is meant solely for emergencies. In reality, it can be used for a range of issues, from routine updates to serious concerns.
- Only nurses can use the SBAR form. While it is widely used by nursing professionals, this communication tool is beneficial for all healthcare team members. Anyone involved in patient care can effectively utilize SBAR.
- SBAR is just a checklist. Some think of SBAR as a simple checklist. It serves as a structured framework, promoting clear and efficient communication but requires thoughtful input.
- Filling out the SBAR form is optional. Certain individuals feel that using the SBAR form is not a requirement. In many organizations, however, it is considered essential for standardized communication.
- Once the SBAR is submitted, the job is done. Many assume that submitting the SBAR form ends their responsibility. Instead, it’s crucial to follow up to ensure the issues raised are addressed.
- SBAR is only for written communication. While the form is often written, it can also guide verbal communication. Practicing SBAR in discussions can enhance clarity and focus on key points.
- Only specific issues can be reported using SBAR. Some believe SBAR is limited to certain topics. In truth, it can address various types of concerns, from policy issues to staffing challenges.
- SBAR replaces clinical judgment. There’s a misconception that SBAR diminishes the need for professional judgment. It should complement clinical decision-making, not replace it.
- The effectiveness of SBAR is guaranteed. While SBAR is a powerful tool, its effectiveness is dependent on how well it is utilized. Proper training and consistent practice are key elements.
Understanding these misconceptions is crucial for harnessing the SBAR form's full potential. Clear and effective communication can lead to better patient care and a more efficient healthcare environment.
Key takeaways
The SBAR Word form serves as a vital tool for effective communication in health care settings. Here are key takeaways on filling out and using this form:
- Each section of the form (Situation, Background, Assessment, Recommendation) has a specific purpose that helps frame the information clearly.
- Always start with **identifying yourself** and providing the relevant context, including your title and the date.
- In the Situation section, state the problem concisely. Mention what happened, when it started, and its severity.
- Use the Background section to include necessary history and details related to the situation. Focus on policies, standards, and occurrences.
- In your Assessment, provide a clear evaluation of the situation. This sets the groundwork for the Recommendation.
- Recommendations should be specific and actionable. Outline what you want to see happen in response to the issue.
- Ensure that all team members involved are aware of the SBAR tool and how to utilize it effectively for addressing issues.
- Document dates for NNLC review and any follow-up actions. This ensures accountability and tracking of the recommendations made.
Utilizing the SBAR Word form effectively can enhance communication within the health care team, leading to improved issue resolution.
Browse Other Templates
Qdro Form for Divorce - Completing the form accurately can simplify future benefit distributions.
Usmc Page 11 Template - This form is a straightforward way to confirm legal education has taken place.