Fill Out Your Stable Program Pre Assessment Form
The S.T.A.B.L.E. Program Pre-Assessment form is a vital tool for healthcare professionals working with newborns, aimed at ensuring that they possess the essential knowledge to manage newborn care, particularly in critical situations. This assessment includes a variety of multiple-choice questions that cover key areas such as methods for rewarming hypothermic infants, appropriate responses to respiratory distress, and the implications of maternal health on an infant's well-being, such as hypoglycemia in infants born to diabetic mothers. The form guides practitioners in evaluating their understanding of complex medical scenarios, fostering their ability to identify potential complications like bacterial sepsis or persistent pulmonary hypertension based on specific clinical presentations. Additionally, the assessment emphasizes the importance of accurate measurements, such as pre- and post-ductal saturation monitoring, while also testing knowledge on appropriate interventions, including the correct administration of medications like dopamine in critically ill infants. Overall, this pre-assessment not only serves as a tool for self-evaluation but also reinforces best practices in neonatal care, ensuring that practitioners remain equipped to provide the highest level of support to vulnerable newborns.
Stable Program Pre Assessment Example
S.T.A.B.L.E.
1
S.T.A.B.L.E. Program
Please write your name and answers on the answer sheet. For the following
1.The following are appropriate methods for rewarming a hypothermic infant:
1)Cover with plastic from chin to feet. Fill latex gloves with hot water and place along both sides of infant’s body
2)Place in incubator and increase environmental air temperature
3)Place infant on top of an activated chemical thermal mattress, after the mattress is covered with a thin cloth
4)Place on radiant warmer on
5)Heat a blanket in a microwave for 15 seconds, then place blanket around infant
a)1, 2, 3
b)2, 3, 4
c)3, 4, 5
2.A
a)Bacterial sepsis, Pneumonia, Persistent Pulmonary Hypertension of the Newborn (PPHN)
b)Viral sepsis, Respiratory Distress Syndrome, Cyanotic congenital heart disease
c)Septicemia, Transient Tachypnea of the Newborn (TTNB), Coarctation of the Aorta
3.Hypoglycemia may result in an infant of a diabetic mother because of:
a)The mother’s elevated glucose levels during pregnancy
b)The mother’s use of insulin during pregnancy
c)The mother’s elevated cortisol levels during pregnancy
Edition 7
S.T.A.B.L.E.
2
4.Bacterial sepsis is suspected in a
a)Give a loading dose of dopamine, 5 micrograms per kilogram, followed by a continuous infusion of dopamine 10 micrograms per kilogram per minute IV.
b)Give dopamine 5 micrograms per kilogram per minute via the peripheral IV or umbilical vein.
c)Give dopamine 5 micrograms per kilogram per minute via the umbilical vein or artery.
5.Pre and
a)Left hand
b)Left hand
c)Right hand
6.The function of brown fat is to:
a)Generate heat when it is metabolized
b)Provide a rapidly available source of glucose in the first day of life
c)Provide an insulating layer of fat in the first month of life
7.A term infant develops severe respiratory distress following aspiration of stomach contents. Following endotracheal intubation, the infant is given positive pressure ventilation with 100% oxygen. The oxygen saturation does not rise above 65%. What problems might occur in this infant?
1)Pulmonary vascular resistance may increase and cause
2)Tissue hypoxia may lead to cell and organ damage
3)Increased glucose utilization may result in hypoglycemia
4)Development of metabolic acidosis following conversion to anaerobic metabolism
a)1 and 3 are correct
b)2 and 4 are correct
c)All are correct
Edition 7
S.T.A.B.L.E.
3
8.A mother is concerned because her
five minutes. In the nursery, the vital signs and exam are: Axillary temperature 36.2 C (97.2 F)
Respiratory rate 80 per minute Mild intercostal retractions Oxygen saturation 85% Capillary refill time 5 seconds Brachial and femoral pulses are weak Hypotonic muscle tone, weak cry
Head circumference 36 centimeters (34 centimeters at birth)
Scalp palpation reveals swelling that extends across suture lines from the front of the anterior fontanelle to the ears on both sides and back to the posterior fontanelle
Given this limited information, which of the following should be strongly suspected?
a)Caput succedaneum
b)Cephalohematoma
c)Subgaleal hemorrhage
9.Endotracheal intubation with positive pressure ventilation should be performed without delay if:
1)You are unable to ventilate and/or oxygenate adequately with bag/mask ventilation
2)The infant is gasping
3)The infant is being transported to another facility
4)The infant has a pneumothorax
a)1, 2
b)3, 4
c)All are correct
Edition 7
S.T.A.B.L.E.
4
Matching.
Infants with the following conditions or physical findings are at risk to develop hypoglycemia. Match the reason for becoming hypoglycemic from the “Causes” column on the right side (choose only one answer per question).
CAUSES
10. |
Infant of a diabetic mother |
a |
b |
c |
11. |
Term, small for gestational |
a |
b |
c |
|
age infant |
|
|
|
12. |
Term newborn in cardiogenic |
a |
b |
c |
|
shock |
|
|
|
13. |
Large for gestational age |
a |
b |
c |
14. |
Premature infant |
a |
b |
c |
a)Decreased glycogen stores
b)Hyperinsulinism
c)Increased utilization of glucose and glycogen stores
15.An infant is breathing 80 times per minute. An arterial blood gas reveals a pH of 7.20 and a PCO2 of 25. Which one of the following conditions should be suspected?
a)Congenital heart disease such as coarctation of the aorta or aortic atresia
b)Pneumonia
c)Congenital diaphragmatic hernia
16.An infant is cyanotic at rest but ‘pinks up’ with crying. You suspect the infant may have:
a)Cyanotic congenital heart disease
b)Transient tachypnea of the newborn
c)Choanal atresia
17.A neonate is experiencing severe respiratory distress in the delivery room. When bag/mask ventilation and oxygen are provided, the infant deteriorates further. The abdomen appears sunken. Which action should be strongly considered?
a)Place in hood oxygen and achieve an oxygen saturation greater than 90%
b)Initiate continuous positive airway pressure with 6 to 8 cm H20 pressure
c)Perform endotracheal intubation and assist ventilation
Edition 7
S.T.A.B.L.E.
5
18.Cardiogenic shock may result because of:
a)Subgaleal hemorrhage, placental abruption, arrhythmias
b)Hypoxia, bacterial infection, severe hypoglycemia
c)Intraventricular hemorrhage, tension pneumothorax, viral infection
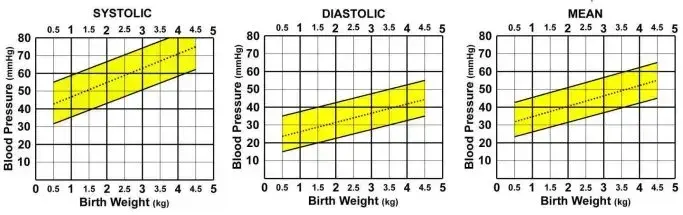
19.
a)Low
b)
c)Normal
(Shaded area between the solid diagonal lines is considered normal)
20.At one hour of life, a term infant weighing 1400 grams (3 pounds, 1.5 ounces) has a serum glucose of 10 mg/dL (0.55 mmol/L). Which of the following orders is the most appropriate therapy in this situation:
a)Begin an intravenous (IV) infusion of D10W at 5 mls per hour (80 mls per kilogram per day). Recheck the blood glucose in one hour.
b)Give 2.8 mls D10W IV slow push, then begin an IV infusion of D10W at 5 mls per hour (80 mls per kilogram per day).
c)Confirm the blood glucose by sending another sample to the lab. If low, give 4 mls/kg D25W IV slow push followed by an IV infusion of D10W at 5 mls per hour (80 mls per kilogram per day).
21.The normal response to cold stress in term infants includes which of the following?
1)Vasodilatation of the coronary arteries
2)Brown fat metabolism
3)Pulmonary vasoconstriction
4)Peripheral vasoconstriction
5)Decreased oxygen consumption
6)Decreased muscle activity and flexion
a)1, 2, 4, 5
b)2, 3, 4
c)All are correct
Edition 7
S.T.A.B.L.E.
6
22.A
Temperature 34 degrees Celsius (93.2 degrees Fahrenheit) Heart rate 100 beats per minute
Respiratory rate 40 (by assisted ventilation) A blood pressure has not been obtained
Which of the following stabilization options should be performed immediately?
1)Establish intravenous access by placing a peripheral intravenous line and administer a 2 ml/kilogram bolus of D25W
2)Move the infant to a radiant warmer, assess patency of the airway, confirm the endotracheal tube is in correct position and well secured
3)Establish intravenous access by placing an umbilical venous catheter and administer a 10 ml/kilogram bolus of normal saline
a)1 and 2
b)2 only
c)2 and 3
The following blood gases are from arterial sites.
23.pH 7.25, PCO2 36, HCO3 (bicarbonate) 15. The correct interpretation of this blood gas is:
a)Uncompensated metabolic acidosis
b)Compensated respiratory acidosis
c)Uncompensated mixed metabolic and respiratory acidosis
24.pH 7.15, PCO2 63, HCO3 (bicarbonate) 21. The correct interpretation of this blood gas is:
a)Uncompensated metabolic acidosis
b)Uncompensated respiratory acidosis
c)Uncompensated mixed metabolic and respiratory acidosis
25.pH 7.0, PCO2 55, HCO3 (bicarbonate) 14. The correct interpretation of this blood gas is:
a)Uncompensated metabolic acidosis
b)Uncompensated respiratory acidosis
c)Uncompensated mixed metabolic and respiratory acidosis
Edition 7
S.T.A.B.L.E.
7
26.pH 7.35, PCO2 23, HCO3 (bicarbonate) 12. The correct interpretation of this blood gas is:
a)Compensated metabolic acidosis
b)Compensated respiratory acidosis
c)Compensated mixed metabolic and respiratory acidosis
27.Which organ is most likely to be adversely affected by severe, persistent hypoglycemia?
a)Liver
b)Kidney
c)Brain
28.A neonate with a pneumothorax may exhibit which of the following symptoms:
1)Increased work of breathing
2)Bradycardia
3)Asymmetric appearing chest
4)Cyanosis
5)Decreased femoral pulses
a)1, 3, 5
b)1, 2, 4
c)All are correct
29.A
a)Too high
b)In good position
c)Too low
30.An infant is born at 42 weeks gestation. Apgars are 3 at one minute, and 5 at five minutes. At 10 minutes of life, the heart rate drops to 60 beats per minute and gasping respirations are noted. The infant is intubated, given assisted ventilation with oxygen, and chest compressions are started. This infant is at risk to develop what complications?
1)Hypoglycemia
2)Acidosis
3)Pneumothorax
4)Seizures
5)Retinal damage from oxygen exposure
a)2 and 3
b)1, 2, 3, 4
c)All are correct
Edition 7
S.T.A.B.L.E.
8
31.An infant is breast feeding when his mother asks you to come and assess him for ‘green’ spit. You notice a lime green colored vomit. The infant’s abdomen is not distended however she appears very irritable and is crying. This history is most consistent with which diagnosis?
a)Malrotation with midgut volvulus
b)Necrotizing enterocolitis
c)Pyloric stenosis
32.An
a)Worrisome - because it indicates decreased inflammatory response
b)Worrisome – because it indicates possible neutrophil depletion
c)Worrisome – because it indicates both viral and bacterial infection are likely
33.The
a)Worrisome – because the numbers indicate an increasing proportion of total mature neutrophils
b)Worrisome – because the numbers indicate an increasing immature and total lymphocyte count
c)Worrisome – because the numbers indicate an increasing proportion of immature neutrophils
34.A
a)Hypertension, atrial arrhythmia, prolonged capillary refill time
b)Irritability, tachycardia, tachypnea
c)Hypotension, bradycardia, slow respirations
35.An infant delivers unexpectedly at home. When the emergency medical personnel arrive, they note the following about the infant’s appearance: very small chin and jaw, obstruction of the airway by the tongue, and extreme respiratory distress. These findings are consistent with:
a)Pierre Robin sequence
b)Tracheoesophageal fistula
c)Choanal atresia
Edition 7
S.T.A.B.L.E.
9
36.A
a)Cyanotic congenital heart disease (cyanotic CHD)
b)Respiratory Distress Syndrome (RDS)
c)Bacterial sepsis
37.Dopamine is a drug prescribed to treat hypotension and may be administered via:
1)Peripheral vein or umbilical venous catheter (UVC)
2)Umbilical artery catheter (UAC)
3)Endotracheal tube
a)1
b)1, 2
c)All are correct
38.A
(101.2 degrees Fahrenheit). A complete blood count (CBC) is ordered with the following results:
WBC ………………………. 9,200
Hemoglobin ……………….. 15
Hematocrit ………………… 46
Platelets …………………… 290,000
Lymphocytes ……………… 51%
Segmented neutrophils ……. 44 %
Band neutrophils ………….. 5 %
You discuss the patient and CBC results with the infant’s healthcare practitioner who responds by saying: “The CBC is normal which reassures me that the baby is fine. I don’t think we need to do anything more than keep a close eye on the baby.”
Your assessment of this response is:
a)You agree with the healthcare practitioner because a normal CBC means this infant is very unlikely to have an infection
b)You disagree with the healthcare practitioner because a normal CBC may be observed when an infant is infected
c)You mostly agree with the healthcare practitioner except you think a CBC should be
Edition 7
S.T.A.B.L.E.
10
39.Which statement(s) about hypothermia are true?
1)Hypothermia stimulates norepinephrine release, which increases metabolic rate and brown fat metabolism
2)Hypothermia causes peripheral vasoconstriction and may lead to tissue hypoxia, dependence on anaerobic metabolism, and impaired brown fat metabolism
3)Hypothermia causes pulmonary vasoconstriction which may result in
a)1 only
b)1 and 2
c)All are correct
40.The parents of a transported infant ask you to explain persistent pulmonary hypertension. The best explanation about this condition is:
a)The lung blood vessels are constricted which makes blood flow under pressure into the lungs. This causes fluid to leak outside of the blood vessels, which floods the lungs and interferes with the normal process of oxygenation.
b)This is a special kind of hypertension that affects the blood vessels in the lungs. It presents at birth in term and near term infants. At approximately two weeks of age, the blood pressure in the lungs will decrease and the problem will resolve. If however, the blood pressure does not decrease, a medication called Nitric Oxide can be given to treat the hypertension.
c)The lung blood vessels are constricted which prevents adequate amounts of blood from entering the lungs. Blood that normally goes to the lungs to become oxygenated is being shunted through a blood vessel called the ductus arteriosus. This causes problems with oxygenation of the blood.
Edition 7
Form Characteristics
| Fact Name | Detail |
|---|---|
| Purpose | The S.T.A.B.L.E. Pre-Assessment form evaluates the knowledge of healthcare providers in caring for newborns. |
| Format | The form consists of multiple-choice questions requiring the best answer selection. |
| Hearing Assessment | The form may include questions related to respiratory and cardiovascular assessments for infants. |
| Content Updates | This form is periodically revised to reflect the latest evidence in neonatal care. |
| Copyrights | The content is protected by copyright laws pertinent to educational materials. |
| State Forms | Variations of the form might exist depending on state regulations. Applicable laws will dictate compliance requirements. |
| Eligibility | Healthcare providers involved in neonatal care should complete the assessment for competency verification. |
| Scoring | Responses are scored to determine the provider's understanding and readiness to apply knowledge in practice. |
| Training Resource | The S.T.A.B.L.E. program serves as a training resource for managing newborns in distress. |
| Procedure | Participants must fill out their names and answers on a dedicated answer sheet provided with the form. |
Guidelines on Utilizing Stable Program Pre Assessment
After filling out the Stable Program Pre Assessment form, the information will be reviewed to determine readiness and knowledge regarding infant care in varying medical situations. This pre-assessment is a crucial step for evaluating the foundational understanding required in the S.T.A.B.L.E. program.
- Write your name at the top of the answer sheet.
- Read each question carefully before selecting an answer.
- For the multiple-choice questions, circle or highlight the answer choice for each question that you believe is correct.
- Make sure to answer all questions, as skipping any may impact the assessment review.
- Double-check your answers to ensure they are marked as intended.
- If there is additional space for comments or notes, fill that out as needed.
- Submit your completed form according to the specified instructions, which may involve turning it in to a designated individual or location.
What You Should Know About This Form
What is the purpose of the S.T.A.B.L.E. Program Pre-Assessment form?
The S.T.A.B.L.E. Program Pre-Assessment form is designed to evaluate the knowledge and understanding of healthcare professionals regarding the care of neonates. It includes multiple-choice questions that assess key concepts essential for the effective management of newborns in clinical settings.
Who needs to complete the S.T.A.B.L.E. Program Pre-Assessment form?
This form is intended for healthcare providers involved in the care of newborns, particularly those participating in the S.T.A.B.L.E. program. This includes nurses, physicians, and other medical professionals working in neonatal care environments.
How should I respond to the questions on the form?
Participants should read each question carefully and select the one best answer for each multiple-choice question. Responses should be written clearly on the answer sheet provided with the form.
Are there any specific guidelines to follow while filling out the form?
Yes, ensure that your name and answers are legibly written on the answer sheet. Review the instructions for any specific requirements before you begin answering the questions.
What happens if I do not complete the form?
If the form is not completed, participants may not meet the prerequisites for the S.T.A.B.L.E. course. It is essential to finish the assessment to proceed with the program effectively.
Is there a time limit for completing the form?
While there is no strict time limit imposed on the assessment, it is recommended that participants complete it in a timely manner to ensure adequate preparation for the course. Prompt completion allows for potential follow-up on any areas needing improvement.
Can I discuss the questions with other participants?
To maintain the integrity of the assessment process, it is advised not to discuss the questions with others. The purpose of the assessment is to individually evaluate knowledge and readiness for the S.T.A.B.L.E. program.
What areas does the pre-assessment cover?
The pre-assessment covers various topics related to neonatal care, including rewarming methods for hypothermic infants, respiratory distress, hypoglycemia, and other critical conditions. Each question is focused on scenarios that healthcare providers may encounter in practice.
Is there feedback available after completing the assessment?
Feedback is typically provided after the completion of the S.T.A.B.L.E. program, alongside recommendations for further study or areas for improvement based on the results of the pre-assessment.
Where can I find additional resources for studying?
Additional resources and study materials for the S.T.A.B.L.E. program may be available on the official program website. Participants are encouraged to review these materials to strengthen their knowledge before the course.
Common mistakes
When individuals fill out the S.T.A.B.L.E. Program Pre-Assessment form, they often make several common mistakes. Knowing what these mistakes are can significantly enhance the accuracy of the responses and ultimately improve the quality of care that infants receive. One of the primary errors is failing to read the questions thoroughly. Some people rush through the form or skim the content, leading them to misunderstand the nuances of the questions. Each question presents specific scenarios or details that are crucial for selecting the correct answer.
Another frequent mistake is overlooking the context provided in the questions. For instance, questions about medical cases often integrate critical details like the infant's age, symptoms, and medical history. Ignoring these factors can result in choosing an answer that may not appropriately reflect the situation presented. A comprehensive understanding of the full context is essential to arrive at the best possible choice.
Many people also experience difficulties with answer selection. They might focus on their initial reaction to a question or guess without weighing all the answer options. It is important to consider each choice carefully, as multiple-choice questions may include answers that are partially correct or misleading. Thoughtful deliberation can prevent misinterpretations and errors in selecting the best answer.
Another common mistake is related to time management. Participants may underestimate how long the assessment will take. Some rush to finish, which can lead to careless mistakes or skipped questions. Allocating adequate time to review not only helps clarify any uncertainties but also allows individuals to cross-check answers for completeness.
In addition, neglecting to ask for clarification is an often-overlooked error. If individuals find a question confusing, it is advisable to seek guidance for clarification rather than leaving it unanswered. Most assessments or educational settings provide avenues for participants to ask questions. Failing to utilize these resources can result in lost opportunities to improve understanding and accuracy.
Lastly, individuals may also make the mistake of not reflecting on their prior knowledge or relying too heavily on memory. It can be beneficial to approach the questions with a mindset open to evidence-based practices and recent learnings rather than relying solely on past experiences. Each assessment serves as an opportunity to reinforce current knowledge and improve skills.
Documents used along the form
The S.T.A.B.L.E. Program Pre-Assessment form is an essential tool for evaluating medical professionals' readiness to care for newborns. Alongside this assessment form, several additional documents often accompany the process, each serving a specific purpose. These documents help to ensure comprehensive assessment, aid in the training of healthcare providers, and improve patient outcomes.
- Infant Assessment Form: This document records detailed clinical observations and physical examinations of the infant, documenting vital signs, reflexes, and overall condition to monitor progress.
- Continuing Education Certificate: Issued upon successful completion of S.T.A.B.L.E. training, this certificate verifies that a healthcare professional has the requisite knowledge to provide specialized care for newborns.
- Clinical Guidelines Booklet: A concise guide outlining standard practices for neonatal care, including emergency protocols and best practice recommendations for common conditions.
- Data Collection Sheet: This sheet is used for gathering information during assessments. It helps track outcomes and ensure data consistency for further evaluation and research.
- Pediatric Advance Directive: A legal document that outlines the medical decisions and preferences of parents regarding the care of their infant in critical situations, ensuring their wishes are respected.
- Discharge Planning Guide: This resource assists healthcare providers in planning follow-up care for the infant after discharge from the intensive care unit or hospital, which is crucial for ongoing monitoring and support.
- Assessment Feedback Form: Completed by participants, this form provides feedback on the S.T.A.B.L.E. assessment experience, helping to identify areas for improvement in training and implementation.
- Clinical Procedure Checklist: A checklist used by healthcare professionals to ensure all necessary procedures, medications, and interventions are performed systematically during the assessment process.
- Referral Form: This document is necessary for referring infants to specialized care providers when specific conditions exceed the immediate capabilities of the assessing facility.
Understanding and utilizing these documents alongside the S.T.A.B.L.E. Program Pre-Assessment form can significantly enhance neonatal care. Each document plays a pivotal role in creating a structured approach to supporting healthcare providers and ensuring that infants receive high-quality care during critical early life stages.
Similar forms
- Clinical Assessment Form: Similar to the Stable Program Pre Assessment, this document gathers vital information about a patient’s condition through structured questions. Both forms focus on identifying medical issues and guiding treatment decisions based on patient responses.
- Patient History Questionnaire: Like the Stable Program, this questionnaire collects background information and relevant clinical history. It is essential for establishing a baseline and understanding potential risk factors.
- Emergency Medical Services (EMS) Report: This report documents pre-hospital care and patient assessments, similar to the Stable Program's focus on immediate clinical evaluations. Both documents aim to provide comprehensive patient details for ongoing treatment.
- Neonatal Risk Assessment Tool: This tool identifies vulnerabilities in infants, paralleling the Stable Program by highlighting critical risk factors and guiding interventions based on specific criteria.
- Medical History and Physical Examination (MHPE) Form: The MHPE form is used for collecting details of an individual’s health history and current status, akin to the Stable Program which assesses immediate clinical needs in infants.
- Standardized Patient Assessment Sheet: This sheet serves as a guideline for evaluating patient conditions. Like the Stable Program, it ensures systematic data collection for effective diagnosis and treatment planning.
- Pediatric Admission Assessment: This document is similar in that it consolidates information about a child’s health for establishing appropriate levels of care, much like how the Stable Program prepares for the specific needs of neonates.
- Nursing Assessment Form: This form captures critical patient data in a structured manner. Similar to the Stable Program, it focuses on clinical signs and symptoms to aid in proper care delivery.
- Developmental Milestone Checklist: This checklist evaluates an infant's growth and development, paralleling the focus of the Stable Program on early identification of potential complications that may need intervention.
Dos and Don'ts
When filling out the S.T.A.B.L.E. Program Pre-Assessment form, it's important to keep a few best practices in mind. Here’s a list of things to do and to avoid:
- DO: Read the instructions carefully before you start filling out the form.
- DO: Write your answers clearly and legibly on the answer sheet provided.
- DO: Pay close attention to each multiple-choice question and select the best answer based on the options given.
- DO: Keep track of time to ensure you complete the assessment within the allotted period.
- DO: Double-check your answers, especially for questions that may seem tricky or confusing.
- DON'T: Rush through the assessment. Take your time to read each question thoroughly.
- DON'T: Use ink that is difficult to read, as it may affect how your answers are interpreted.
Following these guidelines can help ensure your completion of the form is successful. Good luck!
Misconceptions
- Misconception 1: The S.T.A.B.L.E. Pre Assessment form is only for medical professionals.
- Misconception 2: The assessment relies solely on theoretical knowledge and does not consider practical application.
- Misconception 3: All questions in the assessment have the same level of difficulty.
- Misconception 4: Completing the form guarantees certification or competency in neonatal care.
- Misconception 5: The assessment focuses only on specific medical conditions and ignores broader neonatal care principles.
- Misconception 6: There are no resources available to help prepare for the assessment.
- Misconception 7: Performance on the assessment does not reflect the ability to work in a clinical setting.
- Misconception 8: The assessment format is rigid and does not allow for personal interpretation of questions.
- Misconception 9: Completing the assessment is a one-time requirement and does not need to be revisited.
This form is designed for anyone involved in the care of newborns. This includes nurses, respiratory therapists, and even medical students. The goal is to ensure that all caregivers have a solid understanding of essential neonatal care principles.
The assessment includes questions that assess both theoretical knowledge and practical scenarios. Respondents are evaluated based on their ability to apply knowledge to real-life situations involving infant care.
The questions vary in complexity. Some are straightforward, while others require deeper clinical reasoning and critical thinking to arrive at the correct answer.
The completion of the S.T.A.B.L.E. Pre Assessment is one step in the learning process. It helps gauge knowledge but does not guarantee that an individual is fully competent in neonatal care.
This assessment covers a wide range of topics, emphasizing not just specific conditions but also general care strategies and physiological responses in newborns.
Numerous resources, including textbooks, online courses, and study groups, can assist individuals in preparing for the S.T.A.B.L.E. Pre Assessment. Utilizing these resources can enhance understanding and retention.
While performance on the assessment is not the sole indicator of clinical ability, it does provide insights into one's foundational knowledge, which is crucial for effective practice in a neonatal setting.
Though the assessment is multiple-choice, respondents must analyze each scenario critically. Different clinical experiences may influence how one interprets the questions.
Knowledge in neonatal care can change over time with advances in research and practice. Regularly revisiting the assessment and its content ensures that caregivers stay updated on best practices.
Key takeaways
Completing the S.T.A.B.L.E. Program Pre-Assessment form is essential for those involved in neonatal care. Here are key takeaways regarding the form's usage.
- Accurate Information: Participants must provide accurate personal information and responses to ensure proper assessment results and follow-up.
- Multiple-Choice Format: The assessment features multiple-choice questions where only the best answer should be selected for each question.
- Time Management: It is advisable to allocate sufficient time to complete the assessment thoroughly, as rushed answers may lead to errors.
- Focus on Clinical Scenarios: Questions are based on clinical scenarios, requiring a solid understanding of neonatal care principles and protocols.
- Review Resources: Familiarity with standard neonatal care guidelines and resources can enhance performance on the assessment.
- Post-Assessment Follow-Up: After completing the assessment, participants should review their results and seek clarification on any topics that were challenging.
These takeaways can assist individuals in effectively utilizing the S.T.A.B.L.E. Program Pre-Assessment form to enhance their knowledge and skills in neonatal care.
Browse Other Templates
What Is Written on the Back of a Deposit Slip - For urgent transactions, use the overnight mailing instructions provided.
R and D Tax Credits - Taxpayers must calculate averages of their gross receipts for certain lines.
Fresno State Official Transcripts - Requests for transcripts can be crucial for job applications or further education.