Fill Out Your Standard 2809 Form
The Standard Form 2809, commonly known as the Health Benefits Election Form, is essential for federal employees and certain family members who wish to manage their enrollment in the Federal Employees Health Benefits (FEHB) Program. This form facilitates crucial actions, such as enrolling or reenrolling in the program, switching family members who are designated for coverage, or even canceling or suspending an existing enrollment. It caters to a diverse group of users, including current employees, retirees from specific retirement systems, and former spouses eligible under various laws. Notably, details such as Medicare coverage, including Parts A, B, and D, must be accurately reported, particularly if any family member is enrolled in Medicare. Completing SF 2809 accurately ensures that individuals receive the appropriate health benefits based on their unique circumstances, whether they are opting for individual coverage or including family members. The form requires specific information, such as Social Security Numbers and Medicare Beneficiary Identifiers, to confirm eligibility and ensure a smooth enrollment process. Adhering to all instructions provided on the form is crucial for a successful application, as even minor oversights can lead to delays or complications in accessing health benefits.
Standard 2809 Example

Health Benefits Election Form
Form Approved: OMB No.
Uses for Standard Form (SF) 2809
Use this form to:
•Switch designated eligible family member; or Enroll or reenroll in the FEHB Program; or
Elect not to enroll in the FEHB Program (employees only); or Change your FEHB enrollment; or
Cancel your FEHB enrollment; or
Suspend your FEHB enrollment (annuitants or former spouses only).
Who May Use SF 2809
1.Employees eligible to enroll in or currently enrolled in the FEHB Program. Employees automatically participate in premium conversion unless they waive it, see page 6.
2.Annuitants in retirement systems other than the Civil Service Retirement System (CSRS) or Federal Employees Retirement System (FERS), including individuals receiving monthly compensation from the Office of Workers’ Compensation Programs (OWCP).
Note: Civil Service Retirement System (CSRS) and Federal Employees Retirement System (FERS) annuitants and former spouses and children of CSRS/FERS annuitants
3.Former spouses eligible to enroll in or currently enrolled in the FEHB Program under the Spouse Equity law or similar statutes.
4.Individuals eligible for Temporary Continuation of Coverage (TCC) under the FEHB Program, including:
Former employees (who separated from service);
Children who lose FEHB coverage; and
Former spouses who are not eligible for FEHB under item 3 above.
Instructions for Completing SF 2809
Type or Print. We have not provided instructions for those items that have an explanation on the form.
Part A — Enrollee and Family Member Information
You must complete this part.
Item 2.
Item 5.
Item 7.
Item 8.
Item 9. If you are covered by other health insurance, either in your name or under a family member’s policy, check yes and complete item 10.
Item 10. Provide the information requested on any other health insurance that covers you. An FEHB Self Plus One enrollment covers the enrollee and one eligible family member designated by the enrollee. An FEHB Self and Family enrollment covers the enrollee and all eligible family members. If you or a family member is covered under
another FEHB enrollment, check the FEHB box and
stop. Contact your Human Resources office or retirement system immediately as this is a dual coverage situation. Some examples of how this could occur are:
You are enrolling in an FEHB Self Only plan while your spouse has either an FEHB Self Plus One or Self and Family plan, in which you are already covered.
You are enrolling in an FEHB Self Plus One plan while you are also covered under your spouse’s FEHB Self Plus One plan or FEHB Self and Family plan.
You are enrolling in an FEHB Self and Family plan while your spouse is already enrolled in either a FEHB Self Only plan, an FEHB Self Plus One plan that covers you, or an FEHB Self and Family plan that covers you.
You are an employee under age 26 and have no eligible family members. You are enrolling in your own FEHB plan while you are covered under your parent’s FEHB Self Plus One plan or Self and Family plan.
You are an annuitant who is reemployed in the Federal government. You are enrolling in an FEHB plan as an employee while you are covered under your own or a family member’s FEHB plan.
No person may be covered under more than one FEHB enrollment. However, in certain unusual circumstances, your agency may allow you to enroll in order to:
Enable an employee under age 26 who is covered under a parent’s Self Plus One or Self and Family FEHB enrollment to enroll in FEHB to cover his or her own spouse and/or child;
Enable an employee under age 26 who is covered under a parent’s Self Plus One or Self and Family FEHB enrollment, but lives outside his or her parent’s HMO service area, to have FEHB coverage;
Enable an employee who separates or divorces to enroll in FEHB to cover family members who move outside the HMO service area of the covering FEHB Self Plus One or Self and Family enrollment.
In these unusual situations, each enrollee must notify his or her plan as to which family members are covered under which enrollment. See Dual Enrollment information on page 5.
1 |
Standard Form 2809 |
Previous edition is not usable |
Revised November 2019 |
If your enrollment is for Self Plus One or Self and Family, complete the family member information as appropriate. (If you need extra space for additional family members, list them on a separate sheet and attach.)
Important: In order for your Self Plus One FEHB enrollment election to be processed, you must complete the family member information for your designated family member.
The instructions for completing items 13 through 24 for your initial family member also apply to the information you provide for additional family members.
Item 14. Provide the Social Security Number for this family member if he/she has one. If your family member does not have a Social Security Number, leave blank; benefits will not be withheld.
(See Privacy Act Statement on page 5.)
Item 17. Provide the code which indicates the relationship of each eligible family member to you.
Code |
Family Relationship |
|
|
01 |
Spouse |
19 |
Child under age 26 |
09 |
Adopted Child under age 26 |
17 |
Stepchild under age 26 |
10 |
Foster Child under age 26 |
99Disabled child age 26 or older who is incapable of self support because of a physical or mental disability that began before his/her 26th birthday.
Eligible children include your children born within marriage or adopted children; stepchildren; recognized natural children; or foster children who live with you in a regular
Other relatives (for example, your parents) are not eligible for coverage even if they live with you and are dependent upon you.
If you are a former spouse or survivor annuitant, family members eligible for coverage under your Self Plus One or Self and Family enrollment are the natural or adopted children under age 26 of both you
and your former or deceased spouse.
In some cases, a disabled child age 26 or older is eligible for coverage under your Self Plus One or Self and Family enrollment if you provide adequate medical certification of a mental or physical disability that existed before his/her 26th birthday and renders the child incapable of
Note: Your employing office can give you additional details about family member eligibility including any certification or documentation that may be required for coverage. Contact your employing office for more information about covering foster child(ren),“Employing office” means the office of an agency or retirement system that is responsible for health benefits actions for an employee, annuitant, former spouse eligible for coverage under the Spouse Equity provisions, or individual eligible for TCC.
Survivor Benefits
For your surviving family members to continue your FEHB enrollment after your death, all of the following requirements must be met:
Item 18. If your family member does not live with you, enter his/her home address.
Item 19. If your family member has Medicare, check which Parts
(Part A [Hospital Insurance] and/or Part B [Medical Insurance]) he/she has, including prescription drug coverage under Medicare Part D.
Item 20. If your family member has Medicare, enter his/her Medicare Beneficiary Identifier (MBI). This number is on his/her Medicare Card.
Item 21. If your family member is covered by other group insurance, such as private, state, or Medicaid, check the box and complete item 22.
Item 22. Provide the information requested on any other health insurance that covers this family member. If your family
member is covered under another FEHB plan, see instructions for item 10.
Item 23. Enter email address, if applicable, for this family member.
Item 24. Enter preferred telephone number, if applicable, for this family member.
Family Members Eligible for Coverage
Unless you are a former spouse or survivor annuitant, family members eligible for coverage under your Self Plus One enrollment include one eligible family member (spouse or child under age 26) designated by you. A Self and Family enrollment includes you and all of your eligible family members.
Self Plus One
You must have been enrolled for Self Plus One at the time of your death; and
Your designated family member must be entitled to an annuity as your survivor.
Note: The only survivor eligible to continue the health benefits enroll- ment is the designated family member covered under FEHB on the date of death as long as that individual is entitled to a survivor annuity. No other family members are entitled to continue the enrollment even though they may be entitled to a survivor annuity.
Self and Family
You must have been enrolled for Self and Family at the time of your death; and
At least one family member must be entitled to an annuity as your survivor.
Note: All of your survivors who meet the definition of “family member” can continue their health benefits coverage under your enrollment as long as any one of them is entitled to a survivor annuity. If the survivor annuitant is the only eligible family member, the retirement system will automatically change the enrollment to Self Only.
2 |
Standard Form 2809 |
|
Revised November 2019 |
Part B — FEHB Plan You Are Currently Enrolled In
You must complete this part if you are changing, cancelling, or suspending your enrollment.
Item 1. Enter the name of the plan you are enrolled in from the front cover of the plan brochure.
Item 2. Enter your current enrollment code from your plan ID card.
Part C — FEHB Plan You Are Enrolling In or Changing To
Complete this part to enroll or change your enrollment in the FEHB Program.
Item 1. Enter the name of the plan you are enrolling in or changing to. The plan name is on the front cover of the brochure of the plan you want to be enrolled in.
Item 2. Enter the enrollment code of the plan you are enrolling in or changing to. The enrollment code is on the front cover of the brochure of the plan you want to be enrolled in, and shows the plan and option you are electing and whether you are enrolling for Self Only, Self Plus One, or Self and Family.
To enroll in a Health Maintenance Organization (HMO), you must live (or in some cases work) in a geographic area specified by the carrier.
To enroll in an employee organization plan, you must be or become a member of the plan’s sponsoring organization, as specified by the carrier.
Your signature in Part H authorizes deductions from your salary, annuity, or compensation to cover your cost of the enrollment you elect in this item, unless you are required to make direct payments to the employing office.
Part D — Event That Permits You To Enroll, Change, Or Cancel
Item 1. Enter the event code that permits you to enroll, change, or cancel based on a Qualifying Life Event (QLE) from the Table of Permissible Changes in Enrollment that applies to you.
Following each number is a letter, which identifies a specific Qualifying Life Event (QLE); for example, the event code “1A” refers to the initial opportunity to enroll for an employee who elected to participate in premium conversion.
Item 2. Enter the date of the QLE using numbers to show month, day, and complete year; e.g., 06/30/2011. If you are electing to enroll, enter the date you became eligible to enroll (for example, the date your appointment began). If you are making an open season enrollment or change, enter the date on which the open season begins.
Part E — Election NOT to Enroll
Place an “X” in the box only if you are an employee and you do NOT wish to enroll in the FEHB Program. Be sure to read the information
titled Employees Who Elect Not to Enroll or Who Cancel Their Enrollment.
Part F — Cancellation of FEHB
Place an “X” in the box only if you wish to cancel your FEHB enrollment. Also enter your current plan name and enrollment code in
Part B. Be sure to read the information titled Employees Who Elect Not to Enroll or Who Cancel Their Enrollment.
Note For Parts E and F. If you are Electing Not to Enroll or Cancelling your enrollment because you are covered as a spouse or child under another FEHB enrollment, your agency must enter the enrollee’s name, Social Security number, and FEHB enrollment code in REMARKS.
Cancellation of Enrollment
Employees participating in premium conversion may cancel their FEHB enrollment only during the open season or when they experience a Qualifying Life Event. Employees who waived participation in premium conversion, annuitants, former spouses, and individuals enrolled under TCC may cancel their enrollment at any time. However, if you cancel, neither you nor any family member covered by your enrollment are entitled to a
Explanation of Table of Permissible Changes in Enrollment
The tables on pages 6 through 16 illustrate when: an employee who participates in premium conversion; annuitant; former spouse; person eligible for TCC; or employee who waived participation in premium conversion may enroll or change enrollment. The tables show those permissible events that are found in the regulations at 5 CFR Parts 890 and 892.
The tables have been organized by enrollee category. Each category is designated by a number, which identifies the enrollee group, as follows:
1.Employees who participate in premium conversion
2.Annuitants (other than CSRS/FERS annuitants), including individuals receiving monthly compensation from the Office of Workers’ Compensation Programs
3.Former spouses eligible for coverage under the Spouse Equity provision of FEHB law
4.TCC enrollees
5.Employees who waived participation in premium conversion
Employees Who Elect Not to Enroll (Part E) or Who Cancel Their Enrollment (Part F)
To be eligible for an FEHB enrollment after you retire, you must retire:
Under a retirement system for Federal civilian employees, and
On an immediate annuity.
In addition, you must be currently enrolled in a plan under the FEHB Program and must have been enrolled (or covered as a family member) in a plan under the Program for:
The 5 years of service immediately before retirement (i.e., commencing date of annuity entitlement), or
If fewer than 5 years, all service since your first opportunity to enroll. (Generally, your first opportunity to enroll is within 60 days after your first appointment [in your Federal career] to a position under which you are eligible to enroll under conditions that permit a Government contribution toward the enrollment.)
If you do not enroll at your first opportunity or if you cancel your enrollment, you may later enroll or reenroll only under the circumstances
3
Standard Form 2809 Revised November 2019
explained in the table beginning on page 6. Some employees delay their enrollment or reenrollment until they are nearing 5 years before retirement in order to qualify for FEHB coverage as a retiree; however, there is always the risk that they will retire earlier than expected and not be able to meet the
Note for temporary [under 5 U.S.C. 8906a] employees eligible for FEHB without a Government contribution: Your decision not to enroll
or to cancel your enrollment will not affect your future eligibility to continue FEHB enrollment after retirement.
Note 1: If you become covered by a regular enrollment in the FEHB Program, either in your own right or under the enrollment of someone else, your TCC enrollment is suspended. You will need to send documentation of the new enrollment to the employing office maintaining your TCC enrollment so that they can stop the TCC enrollment. If your new FEHB coverage stops before the TCC enrollment would have expired, the TCC enrollment can be reinstated for the remainder of the original eligibility period (18 months for separated employees or 36 months for eligible family members who lose coverage).
Note 2: Former spouses (Spouse Equity) and TCC enrollees who fail to pay their premiums within specified timeframes are considered to have voluntarily cancelled their enrollment.
Annuitants Who Cancel Their Enrollment
CSRS and FERS annuitants and their eligible family members should not use this form but use form RI
Cancellation/Suspension Confirmation, which is available at
Generally, you cannot reenroll as an annuitant unless you are continuously covered as a family member under another person’s enrollment in the FEHB Program during the period between your cancellation and reenrollment. Your employing office or retirement system can advise you on events that allow eligible annuitants to reenroll. If you cancel your enrollment because you are covered under another FEHB enrollment, you can reenroll from 31 days before through 60 days after you lose that coverage under the other enrollment.
If you cancel your enrollment for any other reason, you cannot later reenroll, and you and any family members covered by your enrollment are not entitled to a
Former Spouses (Spouse Equity) Who Cancel Their Enrollment
Generally, if you cancel your enrollment in the FEHB Program, you cannot reenroll as a former spouse. However, if you cancel the enrollment because you become covered under FEHB as a new spouse or employee, your eligibility for FEHB coverage under the Spouse Equity provisions continues. You may reenroll as a former spouse from 31 days before through 60 days after you lose coverage under the other FEHB enrollment.
If you cancel your enrollment for any other reason, you cannot later reenroll, and you and any family members covered by your enrollment are not entitled to a
Temporary Continuation of Coverage (TCC) Enrollees Who Cancel Their Enrollment
If you cancel your TCC enrollment, you cannot reenroll. Your family members who lose coverage because of your cancellation cannot enroll for TCC in their own right nor can they convert to a nongroup policy.
Family members who are Federal employees or annuitants may enroll in the FEHB Program when you cancel your coverage if they are eligible for FEHB coverage in their own right.
Part G — Suspension of FEHB
CSRS and FERS annuitants and their eligible family members should not use this form but use form RI
Cancellation/Suspension Confirmation, which is available at
Place an “X” in the box only if you are an annuitant or former spouse and wish to suspend your FEHB enrollment. Also enter your current plan name and enrollment code in Part B.
You may suspend your FEHB enrollment because you are enrolling in one of the following programs:
A Medicare Advantage plan or Medicare HMO,
Medicaid or similar
TRICARE (including Uniformed Services Family Health Plan or TRICARE for Life),
CHAMPVA, or
Peace Corps.
You can reenroll in the FEHB Program if your other coverage ends. If your coverage ends involuntarily, you can reenroll from 31 days before your other coverage ends through 60 days after your other coverage ends. If your coverage ends voluntarily because you disenroll, you can reenroll during the next open season.
You must submit documentation of eligibility for coverage under the
Part H — Signature
Your agency, retirement system, or office maintaining your enrollment cannot process your request unless you complete this part.
If you are registering for someone else under a written authorization from him or her to do so, sign your name in Part H and attach the written authorization.
If you are registering for a former spouse eligible for coverage under the Spouse Equity provisions or for an individual eligible for TCC as his or her
4 |
Standard Form 2809 |
|
Revised November 2019 |

Part I - Agency or Retirement System Information and Remarks
Leave this section blank as it is for agency or retirement system use only.
Electronic Enrollments
Many agencies use automated systems that allow their employees to make changes using a
If you are not sure whether the electronic enrollment option is available to you, contact your employing office.
Dual Enrollment
No person (enrollee or family member) is entitled to receive benefits under more than one enrollment in the FEHB Program. Normally, you are not eligible to enroll if you are covered as a family member under someone else’s enrollment in the Program. However, such dual enrollments may be permitted under certain circumstances in order to:
Protect the interests of children who otherwise would lose coverage as family members, or
Enable an employee who is under age 26 and covered under a parent’s enrollment and marries or becomes the parent of a child to enroll for Self Plus One or Self and Family coverage.
Each enrollee must notify his or her plan of the names of the persons to be covered under his or her enrollment who are not covered under the other enrollment. See instructions for item 10 for more information.
For the eligible former spouse of an enrollee, the enrollee or the former spouse must notify the employing office within 60 days after the former spouse’s change in status; e.g., the date of the divorce.
An individual eligible for TCC who wants to continue FEHB coverage may choose any plan, option, and type of enrollment for which he or she is eligible. The time limit for a former employee, child, or former spouse to enroll with the employing office is within 60 days after the Qualifying Life Event, or receiving notice of eligibility, whichever is later.
Effective Dates
Except for open season, most enrollments and changes of enrollment are effective on the first day of the pay period after the employing office receives this form and that follows a pay period during any part of which the employee is in pay status. Your employing office can give you the specific date on which your enrollment or enrollment change will take effect.
Note 1: If you are changing your FEHB enrollment from Self Plus One or Self and Family to Self Only so that your spouse can enroll for Self Only, you should coordinate the effective date of your spouse’s enrollment with the effective date of your enrollment change to avoid a gap in your spouse’s coverage.
Note 2: If you are cancelling your FEHB enrollment and intend to be covered under someone else’s enrollment at the time you cancel, you should coordinate the effective date of your cancellation with the effective date of your new coverage to avoid a gap in your coverage.
Temporary Continuation of Coverage (TCC)
The employing office must notify a former employee of his or her eligibility for TCC. The enrollee, child, former spouse, or their representative must notify the employing office when a child or former spouse becomes eligible.
For the eligible child of an enrollee, the enrollee must notify the employing office within 60 days after the qualifying event occurs; e.g., child reaches age 26.
Agency Distribution of SF 2809
Agencies must distribute one copy of the completed SF 2809 to each of the following, as appropriate:
Official Personnel Folder
New Carrier
Old Carrier
Payroll Office
Enrollee
Privacy Act Statement
Pursuant to 5 U.S.C. § 552a (e)(3), this Privacy Act Statement explains why OPM is requesting the information on this form. Authority: OPM is authorized to collect the information requested on this form pursuant to Title 5, U.S.C. Chapter 89 and Title 5 of the Code of Federal Regulations, Part 890 pertaining to enrollment in the Federal Employees Health Benefits (FEHB) Program. OPM is authorized to collect your Social Security Number (SSN) by Executive Order 9397 (November 22, 1943), as amended by Executive Order 13478 (November 18, 2008). Purpose: The principal use of this information will be to share it with the health insurance carrier you select so that it may (1) identify your enrollment in the plan, (2) verify your and/or your family’s eligibility for payment of a claim for health benefits services or supplies, and (3) coordinate payment of claims with other insurance carriers with whom you might also make a claim for payment of benefits. Your SSN and the SSNs of your covered family members may be used as individual identifiers in the FEHB Program. Routine Uses: The information you provide on this form may also be disclosed externally to other Federal agencies or Congressional offices which may have a need to know it in connection with your application for a job, license, grant, or other benefit. It may also be shared and is subject to verification, via paper, electronic media, or through the use of computer matching programs, with national, state, local, or other charitable or Social Security administrative agencies to determine and issue benefits under their programs or to obtain information necessary for determination or continuation of benefits under the FEHB program. In addition, to the extent this information indicates a possible violation of civil or criminal law, it may be shared and verified with an appropriate Federal, state, or local law enforcement agency. A list of routine uses associated with this form can be found in the Privacy Act System of Records Notice (SORN), OPM/CENTRAL 1 Civil Service Retirement and Insurance, available at www.opm.gov/privacy. Consequences of Failure to Provide Information: Providing this information is voluntary, however failure to provide it may result in a delay in processing your enrollment. In addition, failure to furnish your SSN and/or Medicare Beneficiary Identifier may result in the OPM’s inability to ensure the prompt payment of your and/or your family members’ claims for health benefits services or supplies, proper coordination with Medicare, or proper health insurance status reporting to the IRS.
Public Burden Statement
We estimate this form takes an average of 30 minutes to complete, including the time for reviewing instructions, getting the needed data, and reviewing the completed form. Send comments regarding our time estimate or any other aspect of this form, including suggestions for reducing completion time, to the Office of Personnel Management, Retirement Services Publications Team,
5
Standard Form 2809
Revised November 2019
Federal Employees Receiving Premium Conversion Tax Benefits
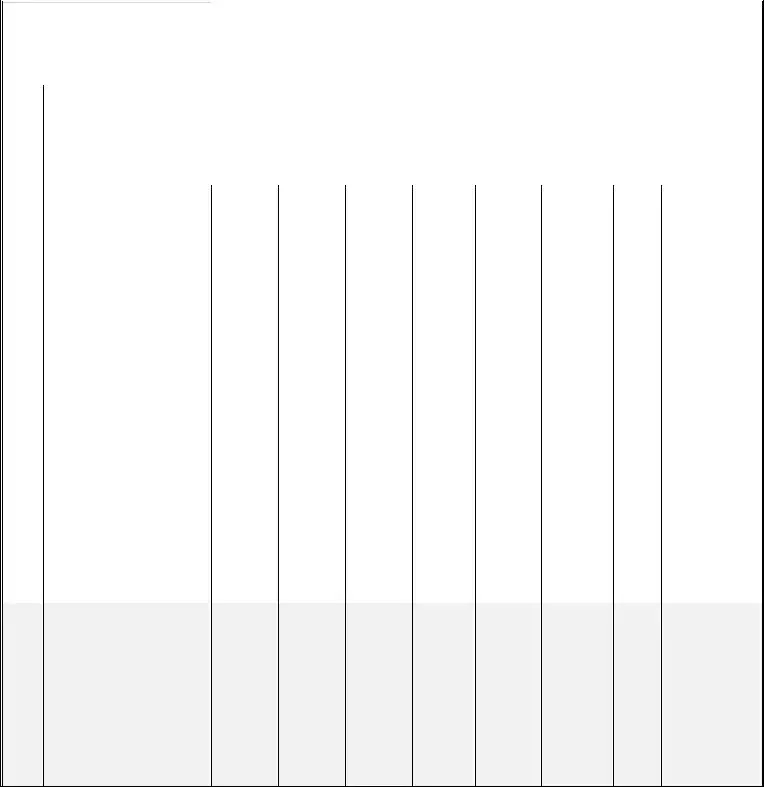
Table of Permissible Changes in FEHB Enrollment and Premium Conversion Election
Premium Conversion allows employees who are eligible for FEHB the opportunity to pay for their share of FEHB premiums with
|
|
Qualifying Life Events (QLE’s) that |
|
|
|
|
|
|
Change that May Be Permitted |
|
|
|
|
|
|
Premium |
|
|
|
Time Limits in |
|
||||||||||||||||
|
|
|
May Permit Change in FEHB |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Conversion Change |
|
|
|
which Change |
|
||||||
|
|
Enrollment, Designated Family |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
that May Be |
|
|
|
May Be |
|
|||||||
|
|
Member or Premium Conversion |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Permitted |
|
|
|
Permitted |
|
|||||||
|
|
|
|
|
Election |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Event |
|
|
Event |
|
|
From Not |
|
|
From Self |
|
|
From One |
|
|
Cancel or |
|
|
Switch |
|
|
Participate |
|
|
Waive |
|
|
When You Must |
||||||||
|
|
Code |
|
|
|
|
|
Enrolled To |
|
|
Only to Self |
|
|
Plan or |
|
|
Change to |
|
|
Designated |
|
|
|
|
|
|
|
|
|
|
File Health Benefits |
||||||
|
|
|
|
|
|
|
|
Enrolled |
|
|
Plus One or |
|
|
Option to |
|
|
Self Plus |
|
|
Family |
|
|
|
|
|
|
|
|
|
|
Election Form With |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
Self and |
|
|
Another |
|
|
One or Self |
|
|
Member |
|
|
|
|
|
|
|
|
|
|
Your Employing |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
Family |
|
|
|
|
|
|
Only |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Office |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1 |
|
Employee electing to receive or receiving premium conversion tax benefits |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1A |
|
Initial opportunity to enroll, for |
|
|
Yes |
|
|
N/A |
|
|
N/A |
|
|
N/A |
|
|
N/A |
|
|
Automatic |
|
|
Yes |
|
|
Within 60 days |
|||||||||
|
|
|
|
example: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unless |
|
|
|
|
|
|
after becoming |
|||
|
|
|
|
• |
New employee |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Waived |
|
|
|
|
|
|
eligible |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
• |
Change from excluded |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
position |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• |
Temporary employee who |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
completes 1 year of service |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
and is eligible to enroll under |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5 USC 8906a |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
1B |
|
Open Season |
|
|
Yes |
|
|
|
Yes |
|
|
|
Yes |
|
|
|
Yes |
|
|
|
Yes |
|
|
|
Yes |
|
|
|
Yes |
|
|
|
As announced by |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
OPM |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
1C |
|
Change in family status that |
|
|
Yes |
|
|
Yes |
|
|
Yes |
|
|
Yes1 |
|
|
Yes |
|
|
Yes |
|
|
Yes |
|
|
Within 60 days after |
|||||||||
|
|
|
|
results in increase or decrease in |
|
|
Employees |
|
|
Employees |
|
|
Employees |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
change in family |
|||||
|
|
|
|
number of eligible family |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
status |
||||||||
|
|
|
|
|
|
may enroll |
|
|
may enroll |
|
|
may enroll |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
members, for example: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
or change |
|
|
or change |
|
|
or change |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
• |
Marriage, divorce, annulment |
|
|
beginning |
|
|
beginning |
|
|
beginning |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
• |
Birth, adoption, acquiring |
|
|
31 days |
|
|
31 days |
|
|
31 days |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
foster child or stepchild, |
|
|
before the |
|
|
before the |
|
|
before the |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
issuance of court order |
|
|
event. |
|
|
event. |
|
|
event. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
requiring employee to provide |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
coverage for child |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Last child loses coverage, for |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
example, child reaches age |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
26, disabled child becomes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
capable of |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
acquires other coverage by |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
court order |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Death of spouse or eligible |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
family member |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
1D |
|
Any change in employee’s |
|
|
Yes |
|
|
|
N/A |
|
|
|
N/A |
|
|
|
N/A |
|
|
|
No |
|
|
|
Automatic |
|
|
|
Yes |
|
|
|
Within 60 days |
|
|
|
|
|
|
employment status that could |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Unless |
|
|
|
|
|
|
|
after employment |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
result in entitlement to coverage, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Waived |
|
|
|
|
|
|
|
status change |
|
|
|
|
|
|
for example: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
•Reemployment after a break in service of more than 3 days
•Return to pay status from nonpay status, or return to receiving pay sufficient to cover premium withholdings, if coverage terminated (If coverage did not terminate, see 1G.)
6
|
Qualifying Life Events (QLE’s) that |
|
|
|
Change that May Be Permitted |
|
|
Premium |
|
|
Time Limits in |
|
||||||||
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
May Permit Change in FEHB |
|
|
|
|
|
|
|
|
|
Conversion Change |
|
|
which Change |
|
||||
|
Enrollment, Designated Family |
|
|
|
|
|
|
|
|
|
that May Be |
|
|
May Be |
|
|||||
|
Member or Premium Conversion |
|
|
|
|
|
|
|
|
|
Permitted |
|
|
Permitted |
|
|||||
|
|
|
|
Election |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Event |
|
|
Event |
From Not |
|
From Self |
From One |
|
Cancel or |
Switch |
|
Participate |
|
Waive |
|
When You Must |
|||
|
Code |
|
|
|
|
Enrolled To |
|
Only to Self |
Plan or |
|
Change to |
Designated |
|
|
|
|
|
|
File Health Benefits |
|
|
|
|
|
|
|
Enrolled |
|
Plus One or |
Option to |
|
Self Plus |
Family |
|
|
|
|
|
|
Election Form With |
|
|
|
|
|
|
|
|
|
Self and |
Another |
|
One or Self |
Member |
|
|
|
|
|
|
Your Employing |
|
|
|
|
|
|
|
|
|
Family |
|
|
Only |
|
|
|
|
|
|
|
Office |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1E |
|
|
Any change in employee’s |
Yes |
|
Yes |
Yes |
|
Yes |
No |
|
Yes |
|
Yes |
|
Within 60 days |
|||
|
|
|
|
employment status that could |
|
|
|
|
|
|
|
|
|
|
|
|
|
after employment |
||
|
|
|
|
affect cost of insurance, including: |
|
|
|
|
|
|
|
|
|
|
|
|
|
status change |
||
|
|
|
|
• Change from temporary |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
appointment with eligibility |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
for coverage under 5 USC |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
8906a to appointment that |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
permits receipt of government |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
contribution |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Change from full time to part- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
time career or the reverse |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1F |
|
|
Employee restored to civilian |
Yes |
|
Yes |
Yes |
|
Yes |
No |
|
Yes |
|
Yes |
|
|
Within 60 days after |
|
|
|
|
|
|
position after serving in uniformed |
|
|
|
|
|
|
|
|
|
|
|
|
|
return to civilian |
|
|
|
|
|
|
services2. |
|
|
|
|
|
|
|
|
|
|
|
|
|
position |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
1G |
|
|
Employee, spouse or eligible |
No |
|
No |
No |
|
Yes |
No |
|
Yes |
|
Yes |
|
Within 60 days |
|||
|
|
|
|
family member: |
|
|
|
|
|
|
|
|
|
|
|
|
|
after employment |
||
|
|
|
|
• Begins nonpay status or |
|
|
|
|
|
|
|
|
|
|
|
|
|
status change |
||
|
|
|
|
insufficient pay3 or |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Ends nonpay status or |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
insufficient pay if coverage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
continued |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• (If employee’s coverage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
terminated, see 1D.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• (If spouse’s or eligible family |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
member’s coverage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
terminated, see 1M.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1H |
|
|
Salary of temporary employee |
|
N/A |
|
No |
Yes |
|
Yes |
No |
|
Yes |
|
Yes |
|
|
Within 60 days |
|
|
|
|
|
insufficient to make withholdings |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
after receiving |
|
|
|
|
|
for plan in which enrolled. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
notice from |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
employing office |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1I |
|
|
Employee (or covered family |
N/A |
|
Yes |
Yes |
|
N/A |
Yes |
|
No |
|
No |
|
Upon notifying |
|||
|
|
|
|
member) enrolled in FEHB health |
|
|
|
|
|
|
|
|
|
|
|
|
|
employing office of |
||
|
|
|
|
maintenance organization (HMO) |
|
|
|
|
|
(see 1M) |
|
|
(see 1M) |
|
(see |
|
move |
|||
|
|
|
|
moves or becomes employed |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1M) |
|
|
|
|||
|
|
|
|
outside the geographic area from |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
which the FEHB carrier accepts |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
enrollments or, if already outside |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
the area, moves further from this |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
area.4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1J |
|
|
Transfer from post of duty within |
|
Yes |
|
Yes |
Yes |
|
Yes |
Yes |
|
Yes |
|
Yes |
|
|
Within 60 days after |
|
|
|
|
|
a State of the United States or the |
|
. Employees |
|
Employees |
Employees |
|
|
|
|
|
|
|
|
|
arriving at new post |
|
|
|
|
|
District of Columbia to post of |
|
may enroll |
|
may enroll |
may enroll |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
duty outside a State of the United |
|
or change |
|
or change |
or change |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
States or District of Columbia, or |
|
beginning |
|
beginning |
beginning |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
reverse. |
|
31 days |
|
31 days |
31 days |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
before |
|
before |
before |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
leaving the |
|
leaving the |
leaving the |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
old post of |
|
old post of |
old post of |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
duty. |
|
duty. |
duty. |
|
|
|
|
|
|
|
|
|
|
|
|
1K |
|
|
Separation from Federal |
Yes |
|
Yes |
Yes |
|
N/A |
No |
|
N/A |
|
N/A |
During employee’s |
||||
|
|
|
|
employment when the employee or |
|
|
|
|
|
|
|
|
|
|
|
|
final pay period |
|||
|
|
|
|
employee’s spouse is pregnant. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
7
|
Qualifying Life Events (QLE’s) that |
|
|
|
|
Change that May Be Permitted |
|
|
Premium |
|
|
Time Limits in |
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
May Permit Change in FEHB |
|
|
|
|
|
|
|
|
|
|
|
|
|
Conversion Change |
|
|
which Change |
|
|||||
|
Enrollment, Designated Family |
|
|
|
|
|
|
|
|
|
|
|
|
|
that May Be |
|
|
May Be |
|
||||||
|
Member or Premium Conversion |
|
|
|
|
|
|
|
|
|
|
|
|
|
Permitted |
|
|
Permitted |
|
||||||
|
|
|
|
Election |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Event |
|
|
Event |
|
From Not |
|
From Self |
|
From One |
|
Cancel or |
Switch |
|
Participate |
|
Waive |
|
When You Must |
||||||
|
Code |
|
|
|
|
|
Enrolled To |
|
Only to Self |
|
Plan or |
|
Change to |
Designated |
|
|
|
|
|
|
|
File Health Benefits |
|||
|
|
|
|
|
|
|
Enrolled |
|
Plus One or |
|
Option to |
|
Self Plus |
Family |
|
|
|
|
|
|
|
Election Form With |
|||
|
|
|
|
|
|
|
|
|
Self and |
|
Another |
|
One or Self |
Member |
|
|
|
|
|
|
|
Your Employing |
|||
|
|
|
|
|
|
|
|
|
Family |
|
|
|
|
Only |
|
|
|
|
|
|
|
|
Office |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1L |
|
|
Employee becomes entitled to |
|
|
No |
|
No |
|
Yes |
|
|
N/A |
|
No |
|
N/A |
|
|
N/A |
|
|
Any time beginning |
|
|
|
|
|
Medicare and wants to change to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
on the 30th day |
|
|
|
|
|
another plan or option.5 |
|
|
|
|
|
|
(Changes |
|
|
(see 1P) |
|
|
|
(see 1P) |
|
|
(see |
|
|
before becoming |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
eligible for |
|
||||
|
|
|
|
|
|
|
|
|
|
|
may be |
|
|
|
|
|
|
|
|
|
1P) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medicare |
|
||
|
|
|
|
|
|
|
|
|
|
|
made |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
only |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
once.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1M |
|
|
Employee or eligible family |
|
Yes |
|
Yes |
|
Yes |
|
Yes |
Yes |
|
Yes |
|
Yes |
|
Within 60 days after |
||||||
|
|
|
|
member loses coverage under |
|
Employees |
|
Employees |
|
Employees |
|
|
|
|
|
|
|
|
|
|
|
loss of coverage |
|||
|
|
|
|
FEHB or another group insurance |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
may enroll |
|
may enroll |
|
may enroll |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
plan including the following: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
or change |
|
or change |
|
or change |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
• Loss of coverage under |
|
beginning |
|
beginning |
|
beginning |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
another FEHB enrollment due |
|
31 days |
|
31 days |
|
31 days |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
to termination, cancellation, or |
|
before the |
|
before the |
|
before the |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
change to Self Plus One or |
|
event. |
|
event. |
|
event. |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
Self Only of the covering |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
enrollment |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Loss of coverage due to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
termination of membership in |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
employee organization |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
sponsoring the FEHB plan6 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Loss of coverage under |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
another |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
health benefits program, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
including: TRICARE, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medicare, Indian Health |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Service |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Loss of coverage under |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medicaid or similar State- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
sponsored program of medical |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
assistance for the needy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Loss of coverage under a non- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Federal health plan, including |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
foreign, state or local |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
government, private sector |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Loss of coverage due to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
change in worksite or |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
residence (Employees in an |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FEHB HMO, also see 1I.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
1N |
|
|
Loss of coverage under a non |
|
|
Yes |
|
Yes |
|
Yes |
|
|
Yes |
|
Yes |
|
Yes |
|
|
Yes |
|
|
From 31 days |
|
|
|
|
|
Federal group health plan because |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
before the |
|
|
|
|
|
an employee moves out of the |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
employee leaves |
|
|
|
|
|
commuting area to accept another |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
the commuting |
|
|
|
|
|
position and the employee’s non- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
area to 180 days |
|
|
|
|
|
Federally employed spouse |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
after arriving in the |
|
|
|
|
|
terminates employment to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
new commuting |
|
|
|
|
|
accompany the employee. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
area |
|
|
1O |
|
|
Employee or eligible family |
|
Yes |
|
Yes |
|
Yes |
|
Yes |
Yes |
|
Yes |
|
Yes |
|
During open season, |
||||||
|
|
|
|
member loses coverage due to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
unless OPM sets a |
||
|
|
|
|
discontinuance in whole or part of |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
different time |
||
|
|
|
|
FEHB plan.7 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
8
|
Qualifying Life Events (QLE’s) that |
|
|
|
Change that May Be Permitted |
|
|
Premium |
|
|
Time Limits in |
|
|||||
|
|
|
|
|
|
|
|
|
|||||||||
|
|
May Permit Change in FEHB |
|
|
|
|
|
|
|
|
Conversion Change |
|
|
which Change |
|
||
|
Enrollment, Designated Family |
|
|
|
|
|
|
|
|
that May Be |
|
|
May Be |
|
|||
|
Member or Premium Conversion |
|
|
|
|
|
|
|
|
Permitted |
|
|
Permitted |
|
|||
|
|
|
Election |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Event |
|
Event |
From Not |
|
From Self |
From One |
Cancel or |
Switch |
|
Participate |
Waive |
|
When You Must |
|||
|
Code |
|
|
|
Enrolled To |
|
Only to Self |
Plan or |
Change to |
Designated |
|
|
|
|
|
File Health Benefits |
|
|
|
|
|
|
Enrolled |
|
Plus One or |
Option to |
Self Plus |
Family |
|
|
|
|
|
Election Form With |
|
|
|
|
|
|
|
|
Self and |
Another |
One or Self |
Member |
|
|
|
|
|
Your Employing |
|
|
|
|
|
|
|
|
Family |
|
Only |
|
|
|
|
|
|
Office |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1P |
|
Enrolled employee or eligible |
No |
|
No |
No |
Yes9 |
Yes |
|
Yes |
Yes |
|
|
Within 60 days after |
|
|
|
|
|
family member gains coverage |
|
|
|
|
|
|
|
|
|
|
|
QLE |
|
|
|
|
|
under FEHB or another group |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
insurance plan, including the |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
following: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Medicare (Employees who |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
become eligible for Medicare |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
and want to change plans or |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
options, see 1L.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• TRICARE for Life, due to |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
enrollment in Medicare. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• TRICARE due to change in |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
employment status, including: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(1) entry into active military |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
service, (2) retirement from |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
reserve military service under |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Chapter 67, title 10. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Health insurance acquired due |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
to change of worksite or |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
residence that affects |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
eligibility for coverage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Health insurance acquired due |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
to spouse’s or eligible family |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
member’s change in |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
employment status (includes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
state, local, or foreign |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
government or private sector |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
employment).8 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1Q |
|
Change in spouse’s or eligible |
No |
|
No |
No |
Yes9 |
Yes |
|
Yes |
Yes |
|
Within 60 days after |
|||
|
|
|
family member’s coverage options |
|
|
|
|
|
|
|
|
|
|
|
QLE |
||
|
|
|
under a health plan, for example: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Employer starts or stops |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
offering a different type of |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
coverage (If no other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
coverage is available, also see |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1M.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Change in cost of coverage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• HMO adds a geographic |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
service area that now makes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
spouse eligible to enroll in |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
that HMO |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• HMO removes a geographic |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
area that makes spouse |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ineligible for coverage under |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
that HMO, but other plans or |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
options are available (If no |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
other coverage is available, |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
see 1M) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
1R |
|
Employee or eligible family |
|
Yes |
|
Yes |
Yes |
Yes9 |
Yes |
|
Yes |
Yes |
|
|
Within 60 days |
|
|
|
|
member becomes eligible for |
|
|
|
|
|
|
|
|
|
|
|
|
after the date the |
|
|
|
|
assistance under Medicaid or a |
|
|
|
|
|
|
|
|
|
|
|
|
employee or |
|
|
|
|
State Children’s Health Insurance |
|
|
|
|
|
|
|
|
|
|
|
|
family member |
|
|
|
|
Program (CHIP). |
|
|
|
|
|
|
|
|
|
|
|
|
becomes eligible |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
for assistance. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
9
(If you are a United States Postal Service employee, these rules may be different. Consult your employing office or information provided by your agency.)
1.Employees may change to Self Only outside of open season only if the QLE caused the enrollee to be the last eligible family member under the FEHB enrollment. Employees may change to Self Plus One outside ofOpen Season only if the QLE causes only one family member to be eligible under the FEHB enrollment. Employees may cancel enrollment outside of open season only if the QLE caused the enrollee and all eligible family members to acquire other health insurance coverage.
2.Employees who enter active military service are given the opportunity to terminate coverage. Termination for this reason does not count against the employee for purposes of meeting the requirements for continuing coverage after retirement. Additional information on the FEHB coverage of employees who return from active military service is available in the Frequently Asked Questions section of the FEHB website at
3.Employees who begin nonpay status or insufficient pay must be given an opportunity to elect to continue or terminate coverage. A termination differs from a cancellation as it allows conversion to nongroup coverage and does not count against the employee for purposes of meeting the requirements for continuing coverage after retirement.
4.This code reflects the FEHB regulation that gives employees enrolled in an FEHB HMO who change from Self Only or Self Plus One to Self and Family or from one plan or option to another a different timeframe than that allowed under 1M. For change to
5.This code reflects the FEHB regulation that gives employees enrolled in FEHB a
6.If employee’s membership terminates (e.g., for failure to pay membership dues), the employee organization will notify the agency to terminate the enrollment.
7.Employee’s failure to select another FEHB plan is deemed a cancellation for purposes of meeting the requirements for continuing coverage after retirement.
8.Under IRS rules, this includes start/stop of employment or nonpay status, strike or lockout, and change in worksite.
9.Employees may change to Self Only outside of Open Season only if the QLE caused all eligible family members to acquire other health insurance coverage. Employees may change to Self Plus One outside of Open Season only if the QLE caused all but one eligible family member to acquire other health insurance coverage. Employees may cancel enrollment outside of Open Season only if the QLE caused the enrollee and all eligible family members to acquire other health insurance coverage.
10
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose of SF 2809 | This form is used by federal employees to manage enrollment in the Federal Employees Health Benefits (FEHB) Program, including enrollment, changes, and cancellations. |
| Eligibility for Use | Employees, annuitants (excluding CSRS/FERS), former spouses under Spouse Equity law, and individuals eligible for Temporary Continuation of Coverage (TCC) can use this form. |
| Medicare Information | Those with Medicare must check which Parts they have and provide their Medicare Beneficiary Identifier (MBI), which is on their Medicare card. |
| Dual Enrollment Restrictions | No individual can receive benefits from more than one FEHB enrollment. Special rules apply to protect children’s coverage in certain cases. |
| Forms Approval | The SF 2809 form is officially approved under OMB No. 3206-0160, allowing its use in enrollment processes. |
| Privacy Act Statements | Privacy Act statements are included to inform users about how their information will be used and the consequences of not providing information. |
| Type of Enrollment Options | Individuals can enroll in various options including Self Only, Self Plus One, or Self and Family plans, depending on their needs. |
| Governing Laws | This form is governed by Title 5, U.S. Code Chapter 89 and Title 5 of the Code of Federal Regulations, involving regulations around health benefits. |
Guidelines on Utilizing Standard 2809
Filling out the Standard Form 2809 is an essential step in managing your health benefits enrollment with the Federal Employees Health Benefits (FEHB) Program. This form allows you to make various changes to your enrollment status or to add eligible family members. To ensure a smooth process, carefully follow these steps to complete the form accurately.
- Part A — Enrollee and Family Member Information: Fill in your personal details such as name, Social Security Number, and other required information in the designated fields.
- Indicate if you are covered by any other health insurance and provide necessary details if applicable.
- Complete the family member information if you are enrolling them, ensuring to list their relationship codes.
- If your family member has Medicare, check the relevant boxes for the parts they are enrolled in and provide their Medicare Beneficiary Identifier.
- Complete the sections for any additional family members as needed, ensuring all required information is included.
- Part B — FEHB Plan You Are Currently Enrolled In: Enter the name of your current health plan and your enrollment code.
- Part C — FEHB Plan You Are Enrolling In or Changing To: Provide the name and enrollment code of the new plan you wish to join or switch to.
- Part D — Event That Permits You To Enroll, Change, Or Cancel: Specify the event code that corresponds with your qualifying life event and the date of the event.
- Part E — Election NOT to Enroll: Mark this section only if you choose not to enroll in the FEHB Program.
- Part F — Cancellation of FEHB: Check this box if you intend to cancel your enrollment and include your current plan name and enrollment code from Part B.
- Part G — Suspension of FEHB: Indicate if you wish to suspend your enrollment by marking the appropriate box.
- Part H — Signature: Sign and date the form. This is crucial for your agency to process your request.
- Part I — Agency or Retirement System Information and Remarks: Leave this section blank. It is meant for agency officials.
After completing the form, review it to ensure all sections are filled out correctly. Double-check for any missing information. Once finalized, submit the form to your Human Resources office or the appropriate retirement system. They will process your request based on the information provided.
What You Should Know About This Form
What is the purpose of the Standard Form 2809?
The Standard Form 2809 serves multiple purposes regarding the Federal Employees Health Benefits (FEHB) Program. It is primarily used to enroll in, change, cancel, or suspend health insurance enrollment. You may also use this form to switch a designated eligible family member or indicate that you do not wish to enroll. Understanding these options ensures that federal employees, former spouses, and eligible family members can effectively manage their health benefits coverage.
Who is eligible to use the Standard Form 2809?
The eligibility to use the Standard Form 2809 is primarily restricted to federal employees currently enrolled in the FEHB Program or those eligible to enroll. This includes annuitants from retirement systems, former spouses qualified under the Spouse Equity law, and individuals eligible for Temporary Continuation of Coverage (TCC). It's crucial to note that Civil Service Retirement System (CSRS) and Federal Employees Retirement System (FERS) annuitants and their families should use a different form, OPM 2809, for their health benefits actions.
What information is required when filling out the form?
When completing the Standard Form 2809, you must provide comprehensive information about yourself and the family members you wish to be covered. Specifically, details such as names, Social Security Numbers, and Medicare Beneficiary Identifiers (if applicable) are needed. Additionally, you must indicate any other health insurance coverage you or your family members may have. This information is vital for determining eligibility and ensuring that benefits are appropriately coordinated.
What happens if I wish to cancel my FEHB enrollment?
If you decide to cancel your FEHB enrollment, you must mark the appropriate box on the form and provide your current plan name and enrollment code. Employees participating in premium conversion can only cancel during the open season or after experiencing a Qualifying Life Event. Be aware that if you cancel, neither you nor any covered family members can enroll in a 31-day temporary extension of coverage. It is advisable to carefully consider the consequences of cancellation, especially regarding future coverage options.
Common mistakes
Filling out the Standard Form 2809 can be a straightforward task, but there are common mistakes that often occur. One prevalent issue is forgetting to indicate whether you are covered by other health insurance. If you are covered, you must check "yes" and provide the necessary information in Item 10. Failing to include this information can lead to complications later in your enrollment process.
Another mistake involves the completion of family member information. When enrolling in a Self Plus One or Self and Family plan, individuals sometimes neglect to provide the required details about their designated family member. Omitting this crucial information can delay the processing of your application. It is essential to ensure that all family member information is filled out correctly.
People often overlook the importance of including social security numbers for eligible family members in Item 14. If your family member has a social security number, it must be included; if they do not have one, simply leave the section blank. Missing this detail can hinder eligibility verification and affect benefits in the long run.
Additionally, some individuals misinterpret the section regarding relationship codes. Each eligible family member requires designation with the correct code in Item 17. Mislabeling the relationship can lead to denied coverage or enrollment errors, so it's crucial to check and verify these codes carefully.
Failing to check the Medicare status for family members eligible for Medicare is another common mistake. In Item 19, it is essential to indicate if they have Parts A, B, or D of Medicare. Neglecting this step could result in issues with coverage coordination between FEHB and Medicare.
Another frequent error occurs in Part D, where individuals might enter the date of a qualifying life event incorrectly. The date format is critical, as it should consist of month, day, and complete year. Misstating this information could result in an inability to process changes related to enrollment accurately.
People sometimes forget to sign the form in Part H, which is necessary for processing the enrollment request. Without a signature, the agency or retirement system cannot proceed, leading to unnecessary delays.
Some individuals also misunderstand the implications of choosing not to enroll or canceling their enrollment. If you wish to take such actions, it’s important to ensure that these sections are filled out accurately to avoid complications with future benefits.
It is common for people to confuse the limits on dual enrollment in the FEHB Program. If you are covered by another enrollment, it is vital to understand that you cannot be enrolled in more than one FEHB plan. If this situation arises, contacting your Human Resources office is essential.
Lastly, many individuals fail to keep track of required documentation that must accompany the form. Friends and family can be a helpful resource, but it is ultimately your responsibility to ensure that everything is submitted properly. Missing documentation may lead to an incomplete application, further delaying your benefits.
Documents used along the form
The Standard Form 2809 is a crucial document for federal employees who need to manage their health benefits enrollment. There are several other forms and documents that often accompany this form, enabling individuals to complete various processes related to health benefits. Understanding these related documents can help ensure a smoother experience when modifying health insurance choices.
- Form RI 79-9: Health Benefits Cancellation/Suspension Confirmation is typically used by Civil Service Retirement System (CSRS) and Federal Employees Retirement System (FERS) annuitants. This form confirms the cancellation or suspension of health benefits and is required for managing these specific cases.
- SF 2808: This form is used to designate eligible family members for health benefits. It helps identify who is covered under a specific FEHB enrollment, ensuring clarity on coverage for family members.
- Temporary Continuation of Coverage (TCC): This option allows former employees, children, and certain former spouses to maintain their health coverage under the FEHB Program temporarily after leaving federal service. TCC documentation is essential for those eligible to apply for continued coverage.
- SF 2807: This is the Health Benefits Election Form for a new employee. It is used when someone is entering federal service and helps establish their initial health care enrollment.
- Form 1-9: The Employment Eligibility Verification form is essential for all employees. While it does not directly relate to health benefits, it verifies the identity and employment authorization of individuals, which can affect their eligibility for federal health plans.
- OPM Form 42: This form is used for reporting family member status changes to the Office of Personnel Management (OPM). It assists in updating information relevant to family members covered under the health benefits program.
- Medicare Part D Enrollment Form: When individuals are eligible for Medicare, they must complete this form to enroll in prescription drug coverage. This document is crucial for those managing dual coverage under FEHB and Medicare.
- SF 2801: Application for Death Benefits for Federal Employees or Retirees is vital when dealing with health benefits after the death of an enrollee. It outlines the processes for family members seeking health coverage continuation in such circumstances.
- Form 8821: The Tax Information Authorization form allows individuals to authorize the IRS to disclose tax return information to the designated individuals, which could affect eligibility for specific health programs based on income considerations.
Using these documents efficiently can streamline the process of enrolling in or modifying health benefits. Ensuring that the details are accurate and timely helps federal employees and their families access the healthcare services they need without unnecessary complications.
Similar forms
- Form SF 2808: This document is utilized to apply for or change health benefits coverage. Like the Standard 2809, it facilitates changes in enrollment and is focused on health benefits for federal employees.
- Form SF 2807: This form is used to request an annuity for retirement. Both documents support ongoing health and financial wellbeing, indicating changes in personal status.
- Form RI 79-9: Used for health benefits cancellation/suspension confirmation. Similar to SF 2809, it assists in managing health benefits during significant life changes.
- Form SF 2810: This is a notice of change in health benefits enrollment. It similarly addresses changes due to qualifying life events.
- FEHB Enrollment Change Form: This form specifically allows federal employees to make changes in their health benefits coverage, like that of the Standard 2809.
- Form SF 2823: This document is used to designate a beneficiary for life insurance under the Federal Employees' Group Life Insurance program. Both forms aim to provide protection for individuals and their families.
- Form TSP-1: This form allows federal employees to make changes to their Thrift Savings Plan. Similar to the Standard 2809, it helps individuals manage their investments and future financial security.
- Form 1095-B: This is used for reporting health coverage. While not a direct enrollment form, it shares the goal of ensuring individuals have the necessary health coverage.
- Medicare Enrollment Application: This application is for enrolling in Medicare, parallel to how the Standard 2809 manages enrollment in health coverage programs.
Each of these forms, while serving specific purposes, supports the overarching need for individuals and families to manage health and financial benefits effectively. They are designed to assist users in navigating significant transitions related to their benefits.
Dos and Don'ts
Things to Do When Filling Out Standard Form 2809:
- Provide accurate information for Part A, including your name and contact details.
- Clearly indicate if you are covered by other health insurance in Item 10.
- Double-check that you have included your Medicare Beneficiary Identifier (MBI) if applicable.
- Use the correct enrollment code for the plan you are currently in and the one you are switching to.
- Complete family member information if enrolling in a Self Plus One or Self and Family option.
- Sign and date the form in Part H to authorize the requested changes.
Things to Avoid When Filling Out Standard Form 2809:
- Do not leave any mandatory fields in Part A incomplete.
- Avoid using a Social Security Number for family members if they do not have one; leave that field blank.
- Do not check the FEHB box if you or a family member is already covered under another FEHB plan.
- Refrain from submitting the form without reviewing the Privacy Act Statement and Public Burden Statement.
- Do not forget to attach any necessary documentation if required, especially for dual enrollments.
- Do not leave Part I blank if your agency requires information about their processing; comment as needed.
Misconceptions
- Misconception 1: You need to be divorced to stop covering your spouse under the FEHB program.
- Misconception 2: Medicare coverage is irrelevant for filling out the Standard Form 2809.
- Misconception 3: Only current employees can use the Standard Form 2809.
- Misconception 4: You can cover anyone under your FEHB plan as long as they live with you.
- Misconception 5: You must use the Standard Form 2809 even if you are a CSRS or FERS annuitant.
- Misconception 6: Completing the form is straightforward, and you don’t need to worry about dual enrollments.
- Misconception 7: Once you submit the form, your enrollment changes take effect immediately.
- Misconception 8: Cancelling your FEHB coverage is the same as opting not to enroll.
In reality, if you are separated but not divorced, you are still considered married. Thus, your spouse remains eligible for coverage under the FEHB program until a legal divorce occurs.
This is untrue. If you or a family member has Medicare, the form requires checking which Parts are held, including the prescription drug coverage found under Medicare Part D. This information is critical for accurate health benefits enrollment.
While current employees can certainly use it, this form is also available for annuitants or former spouses eligible to enroll in the FEHB program. It's designed to accommodate a variety of situations.
This is misleading. Only specific family members, like children or a spouse, can be covered. Other relatives, such as parents or siblings, are not eligible for coverage under your plan.
Instead of this form, CSRS and FERS annuitants should use form RI 79-9 for health benefits actions. Using the wrong form could delay processing your needs.
It's essential to be mindful of dual coverage situations. If you or a family member is already under another FEHB enrollment, this can complicate your coverage and you may need to contact your Human Resources office for assistance.
This isn't the case. Most changes are effective on the first day of the pay period after your request is processed. Understanding the timeline helps to prevent lapses in your coverage.
These are different actions with different consequences. Cancelling your coverage can have significant implications for you and your family, including not being eligible for a temporary continuation of coverage.
Key takeaways
When filling out and using the Standard Form 2809, there are several important points to keep in mind:
- Understand Eligibility: Only certain individuals can use this form, such as employees, annuitants, former spouses, and those eligible for Temporary Continuation of Coverage (TCC).
- Qualifying Events Matter: A specific event must prompt your enrollment, change, or cancellation. Examples include a marriage, divorce, or loss of other health coverage.
- Dual Enrollment Restrictions: No one can receive benefits from more than one enrollment in the FEHB Program. Check for existing coverage before proceeding.
- Complete Required Sections: Make sure to fill out Parts A through H as applicable. Missing information can delay processing or lead to enrollment issues.
- Medicare Details Required: If you or your family members are covered by Medicare, include pertinent Medicare details such as the Medicare Beneficiary Identifier.
- Submit Promptly: Ensure you submit the completed form to your employing office as soon as possible to avoid coverage gaps.
- Document Retention: Keep copies of the form and any correspondence related to your health benefits for your records.
By following these key takeaways, you can navigate the process of using the Standard Form 2809 more efficiently and ensure that your health benefits are properly managed.
Browse Other Templates
Disclosure Form - Each signature denotes consent to the terms and validity of the services detailed.
Electrical Test Sheet - This electrical installation certificate confirms compliance with British Standard 7671.
California Resale Certificate Form - Signatures of authorized representatives confirm the information provided.