Fill Out Your Suboxone Wellcare Form
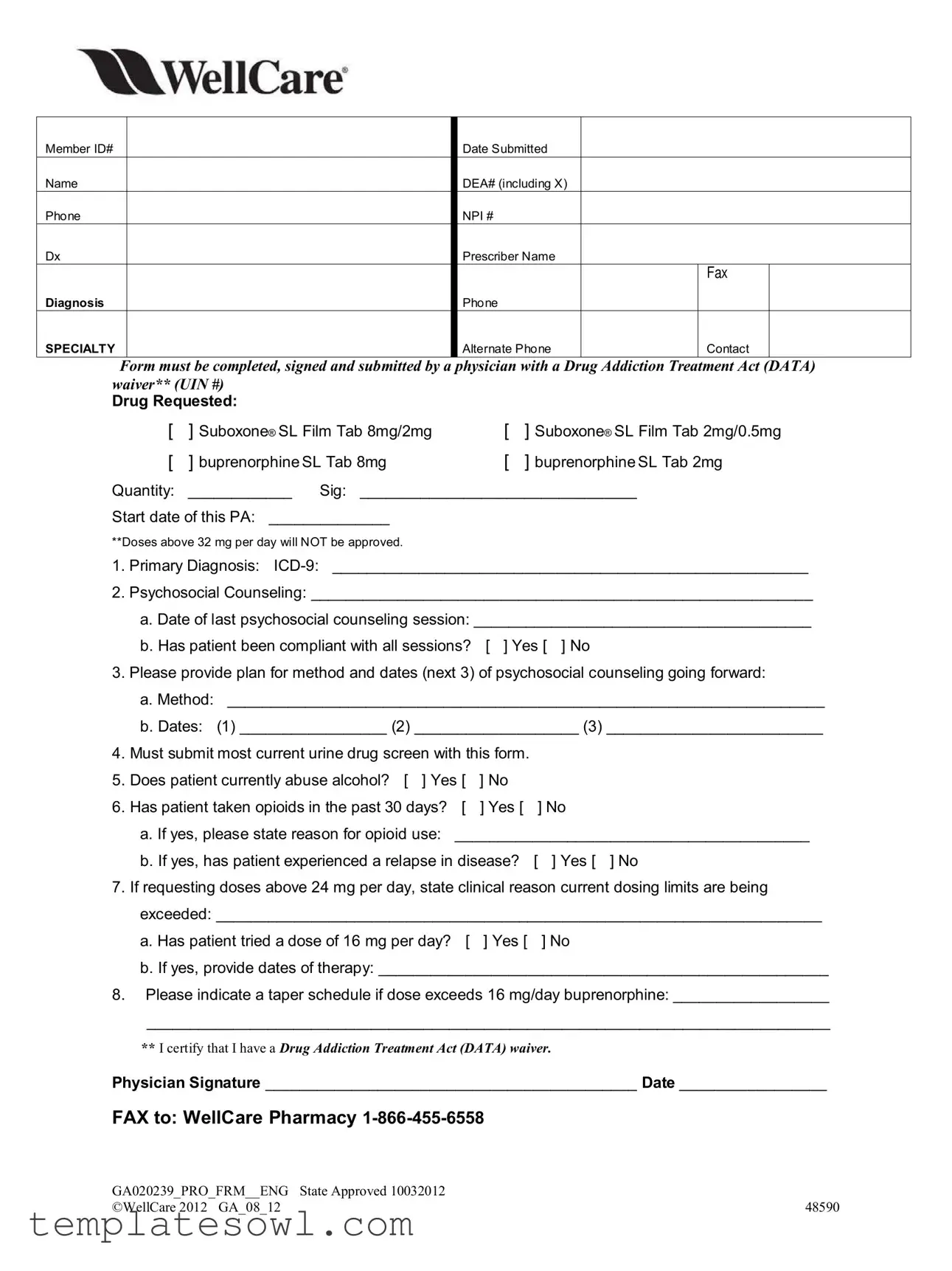
The Suboxone Wellcare form serves as a critical tool in the process of accessing necessary medications for individuals grappling with opioid use disorder. Designed specifically for healthcare providers, this document requires careful completion to ensure that patients receive the appropriate treatment they need. Key sections of the form outline essential information such as member identification and contact details, including the prescriber's DEA and NPI numbers. Healthcare professionals must provide specific details about the requested medication, including the type of Suboxone or buprenorphine, dosages, and the quantity needed. It also emphasizes the importance of psychosocial counseling by inquiring about past sessions and future counseling plans, while ensuring that recent urine drug screens are submitted alongside the application. A commitment to detailed documentation extends to inquiries about the patient's alcohol use and history of opioid consumption. All these facets underscore the need for practitioners to certify their credentialing under the Drug Addiction Treatment Act (DATA), ensuring that the care offered is not just effective, but also compliant with regulatory standards. Hence, this form is not merely a bureaucratic requirement; it serves as a vital touchpoint for patient care and advocacy, promoting a pathway to recovery for those in need.
Suboxone Wellcare Example
Member ID#
Name
Phone
Dx
Diagnosis
SPECIALTY
Date Submitted
DEA# (including X)
NPI #
Prescriber Name
FAX
Phone
Alternate Phone |
Contact |
Form must be completed, signed and submitted by a physician with a Drug Addiction Treatment Act (DATA) waiver** (UIN #)
Drug Requested:
[ |
] Suboxone® SL Film Tab 8mg/2mg |
[ |
] Suboxone® SL Film Tab 2mg/0.5mg |
[ |
] buprenorphineSL Tab 8mg |
[ |
] buprenorphineSL Tab 2mg |
Quantity: |
____________ Sig: ________________________________ |
||
Start date of this PA: ______________
**Doses above 32 mg per day will NOT be approved.
1.Primary Diagnosis:
2.Psychosocial Counseling: __________________________________________________________
a. Date of last psychosocial counseling session: _______________________________________
b. Has patient been compliant with all sessions? [ ] Yes [ ] No
3.Please provide plan for method and dates (next 3) of psychosocial counseling going forward:
a.Method: _____________________________________________________________________
b.Dates: (1) _________________ (2) ___________________ (3) _________________________
4.Must submit most current urine drug screen with this form.
5. |
Does patient currently abuse alcohol? [ ] Yes [ |
] No |
|
|
6. |
Has patient taken opioids in the past 30 days? |
[ |
] Yes [ |
] No |
|
a. If yes, please state reason for opioid use: _________________________________________ |
|||
|
b. If yes, has patient experienced a relapse in disease? |
[ ] Yes [ ] No |
||
7. |
If requesting doses above 24 mg per day, state clinical reason current dosing limits are being |
|||
|
exceeded: ______________________________________________________________________ |
|||
|
a. Has patient tried a dose of 16 mg per day? |
[ |
] Yes [ |
] No |
b. If yes, provide dates of therapy: ____________________________________________________
8.Please indicate a taper schedule if dose exceeds 16 mg/day buprenorphine: __________________
_______________________________________________________________________________
**I certify that I have a Drug Addiction Treatment Act (DATA) waiver.
Physician Signature ___________________________________________ Date _________________
FAX to: WellCare Pharmacy
GA020239_PRO_FRM__ENG |
State Approved 10032012 |
©WellCare 2012 GA_08_12 |
48590 |
Form Characteristics
| Fact Name | Details |
|---|---|
| Required Prescriber | The form must be completed and signed by a physician with a Drug Addiction Treatment Act (DATA) waiver. |
| Drug Options | Physicians can request specific drug types: Suboxone® SL Film Tabs and buprenorphine SL Tabs. |
| Submission Requirements | A current urine drug screen must accompany the submission of this form. |
| Compliance Questions | Questions regarding the patient's substance use and counseling compliance are mandatory. |
| Dosage Limits | Doses above 32 mg per day will not be approved unless justified with clinical reasons. |
| Governing Law | The form follows regulations outlined under the Drug Addiction Treatment Act (DATA). |
Guidelines on Utilizing Suboxone Wellcare
Completing the Suboxone Wellcare form involves several steps to ensure accurate information is provided for the medication request. Once your form is filled out, it should be signed and sent to WellCare Pharmacy for processing.
- Begin by entering the Member ID# at the top of the form.
- Fill in the Name, Phone, and Dx Diagnosis fields.
- Enter the Date Submitted.
- Provide the DEA# (including X) and NPI #.
- Write the Prescriber Name, FAX Phone, and Alternate Phone Contact information.
- Check the appropriate box for the Drug Requested (Suboxone® SL Film or buprenorphineSL Tab).
- Specify the Quantity and Sig (instructions for use).
- Indicate the Start date of this PA.
- For the primary diagnosis, fill in the ICD-9 code next to Primary Diagnosis.
- Provide details regarding Psychosocial Counseling, including:
- The Date of last counseling session.
- Whether the patient has been compliant with all sessions (Yes or No).
- Outline the plan for method and dates of psychosocial counseling going forward.
- Submit the most recent urine drug screen with this form.
- Answer whether the patient currently abuses alcohol (Yes or No).
- Indicate if the patient has taken opioids in the past 30 days (Yes or No), and if applicable, specify the reason for opioid use.
- If opioids were used, state if there has been a relapse (Yes or No).
- If requesting doses above 24 mg, provide a clinical reason for exceeding current dosing limits.
- Specify if the patient has tried a dose of 16 mg per day (Yes or No) and, if yes, provide dates of therapy.
- If the dose exceeds 16 mg/day buprenorphine, indicate the taper schedule.
- Finally, sign and date the form as a certification of having a Drug Addiction Treatment Act (DATA) waiver.
- Fax the completed form to WellCare Pharmacy at 1-866-455-6558.
What You Should Know About This Form
What is the purpose of the Suboxone Wellcare form?
The Suboxone Wellcare form serves as a request for prior authorization when a prescriber aims to prescribe Suboxone or other buprenorphine formulations for a patient. It ensures that the prescribing physician has the appropriate qualifications and that the patient meets the necessary criteria for treatment. This helps to promote responsible prescribing practices and keep patients safe.
Who can complete and submit the Suboxone Wellcare form?
The form must be completed, signed, and submitted by a physician who holds a valid Drug Addiction Treatment Act (DATA) waiver. Only physicians who have this specific certification can prescribe Suboxone, ensuring they are trained in treating individuals with substance use disorders.
What information is required on the form?
Essential details include the member's ID number, name, phone number, diagnosis, and prescriber information such as the DEA number and NPI number. The drug being requested, quantity, signature of the prescriber, and clinical information regarding the patient’s treatment history and compliance with counseling sessions must also be provided.
What are the restrictions on dosing for Suboxone?
The form notes that doses exceeding 32 mg per day will not be approved. If a prescriber requests doses above 24 mg per day, they must provide a clinical reason to justify this request and confirm whether the patient has attempted lower dosing levels, including a specific mention of any experience with 16 mg therapy.
Is documentation of psychosocial counseling required?
Yes, the form requires the physician to provide information about the patient’s psychosocial counseling. This includes patient compliance and the schedule for upcoming counseling sessions. Documentation assures that the patient is receiving comprehensive care to support their recovery efforts.
What should be submitted alongside the form?
A current urine drug screen is mandatory. This test helps to verify the patient’s substance use history and assists in the clinical decision-making process. Submitting this information is critical for the approval of the prior authorization request.
What if the patient has a history of alcohol abuse or recent opioid use?
The form inquires whether the patient currently abuses alcohol or has taken opioids in the past 30 days. If opioid use is evident, the prescriber must state the reason for that use and indicate if a relapse has occurred. Such questions are pertinent for assessing the risk factors associated with the patient's treatment plan.
How do prescribers indicate their qualification to prescribe?
At the end of the form, the prescriber must certify their DATA waiver status by signing and dating the document. This signature confirms their authority to prescribe medications for substance use disorders and indicates their commitment to following the regulations governing such prescriptions.
Common mistakes
Filling out the Suboxone Wellcare form can be straightforward, but mistakes are often made. These errors can delay treatment or lead to complications. Addressing these issues upfront can save time and facilitate access to necessary care.
One common mistake is neglecting to include a valid Member ID. This essential identifier allows the insurer to locate the patient’s information efficiently. Failing to provide this detail may lead to unnecessary delays in processing the request.
Another frequent error is providing incomplete or inaccurate patient information. For example, not including the correct diagnosis or leaving out the Drug Addiction Treatment Act (DATA) waiver information can derail the application. Every section of the form must be filled out accurately to avoid rejection.
Omitting the quantity and specific drug requested can become a significant hurdle. This includes not specifying whether the prescription is for Suboxone® SL Film or buprenorphine. Consequently, each item requested should be checked clearly to ensure that the right medication is dispensed.
Failing to provide the date of the last psychosocial counseling session is another mistake. This detail is critical for assessing the patient’s treatment progress. Additionally, it is crucial to note whether the patient has been compliant with their counseling sessions. If “no” is marked, providing explanations can help gain approval.
Another area that can lead to confusion is the failure to submit a current urine drug screen. This requirement is mandatory and should accompany the completed form. Omitting it can halt the approval process entirely.
Responding incorrectly to questions about alcohol and opioid use can also be problematic. Be honest and accurate in answering whether the patient currently abuses alcohol or has taken opioids in the past 30 days. Misrepresentation here could lead to serious repercussions and delay in treatment.
Additionally, providing insufficient clinical reasoning for higher dose requests can undermine the entire application. If the required doses exceed 24 mg, clear justification must be given as to why this is needed. Failing to do so will result in rejection of the request.
Finally, forgetfulness regarding the taper schedule can create complications. If the dose exceeds 16 mg per day, a taper plan must be outlined. Neglecting this step leaves the application incomplete and likely unapproved.
Documents used along the form
When navigating the process of obtaining medication such as Suboxone, it is common to encounter several forms and documents that are essential for various purposes. Each serves a unique role in ensuring that both patients and healthcare providers comply with regulations and properly document treatment. Understanding these documents may help streamline the process.
- Prior Authorization Form: This document is needed to obtain approval from an insurance company before a prescribed medication is covered. It usually requires details about the patient's medical history, treatment plan, and the specific medication being requested.
- Urine Drug Screening Results: A current urine drug test is typically required to provide evidence of the patient's compliance with their treatment plan. This screening helps to monitor substance use and ensure the patient's safety during therapy.
- Patient Medication Agreement: This agreement outlines the responsibilities of both the physician and the patient regarding the prescribed treatment. It often includes information about potential risks, rules on medication use, and consequences for non-compliance.
- Psychosocial Assessment Form: This form gathers information about the patient's psychosocial history, including mental health status and social circumstances. It is crucial for developing a comprehensive treatment plan and identifying any necessary support services.
Familiarizing oneself with these forms can provide clarity and support during the treatment process. Each document plays a critical role in ensuring that care is delivered responsibly and effectively, ultimately contributing to better health outcomes.
Similar forms
- Prior Authorization Form: Similar to the Suboxone Wellcare form, it requires detailed patient information, diagnosis, and treatment background. Both forms must be completed by a qualified healthcare provider.
- Medication Request Form: These forms offer a systematic approach to specifying medications, dosages, and requested treatment plans. Each also needs collaboration between the provider and the patient.
- Patient Medical History Form: Both documents collect information about the patient's past medical and treatment history, aiding in understanding the patient's current condition.
- Substance Abuse Assessment Form: Designed to evaluate substance use disorders, this form gathers information on the frequency and reasons for substance use similar to how the Suboxone Wellcare form does.
- Psycho-Social Evaluation Form: Like the Suboxone form, it emphasizes the necessity of psychosocial counseling and the patient’s compliance with sessions.
- Informed Consent for Treatment Form: This document relates to the understanding of the treatment process and implications, much like the need for the physician's acknowledgment in the Suboxone form.
- Drug Screening Consent Form: Both documents stress the importance of drug screening to ensure safe treatment, requiring confirmation of recent tests and compliance with screening protocols.
- Patient Care Plan Documentation: Both forms outline a tailored care plan, including medication dosage and management strategies, while ensuring ongoing evaluation of the patient's condition.
Dos and Don'ts
When filling out the Suboxone Wellcare form, it's important to approach the process thoughtfully. Here are some helpful guidelines to consider:
- Do: Ensure that all required fields are filled out completely.
- Do: Use accurate member identification numbers and prescriber details.
- Do: Keep a copy of the completed form for your records.
- Do: Confirm that the prescriber has a valid Drug Addiction Treatment Act (DATA) waiver.
- Do: Provide clear and honest information about the patient’s current treatment and diagnoses.
- Don't: Skip the submission of the most current urine drug screen.
- Don't: Provide false information or make assumptions about the patient's drug use.
- Don't: Forget to sign the form, as an unsigned form will delay or void the request.
- Don't: Indicate a quantity or dosage that exceeds the approved limits without providing a clinical rationale.
- Don't: Delay submitting the form, as it can impact the patient's access to treatment.
Misconceptions
- Misconception 1: The form can be completed by anyone.
- Misconception 2: Any dosage of Suboxone is approved without restrictions.
- Misconception 3: The patient’s psychosocial counseling history is irrelevant to the approval process.
- Misconception 4: The form does not need a current urine drug screen.
- Misconception 5: Alcohol abuse history is not a factor in prescribing Suboxone.
- Misconception 6: Past opioid use does not need to be reported.
- Misconception 7: The tapering schedule is optional if the dose exceeds 16 mg per day.
This is incorrect. Only a physician with a Drug Addiction Treatment Act (DATA) waiver can complete and submit the Suboxone Wellcare form. This ensures that only qualified professionals are involved in the treatment process.
In reality, doses above 32 mg per day will not be approved. The form outlines clear dosage limits to ensure patient safety and effective management of treatment.
This is a misunderstanding. The form requires details about the patient's psychosocial counseling sessions, including compliance with those sessions, to determine eligibility for treatment.
In fact, a current urine drug screen must be submitted with the form. This requirement helps evaluate the patient's substance use and compliance.
This misconception is false. The form specifically asks whether the patient currently abuses alcohol, as this can impact the approach to treatment and overall patient safety.
That is incorrect. The form requires information about any opioid use in the past 30 days, including the reasons for use and any potential relapse. This information is crucial for assessing risk factors in the treatment plan.
This is a misunderstanding. If the requested dose exceeds 16 mg per day, the form explicitly requests a taper schedule. This helps ensure that dosages are managed carefully to promote safe and effective treatment.
Key takeaways
Filling out and using the Suboxone Wellcare form can be straightforward if you keep in mind the following essential points:
- Eligibility Requirement: The form must be completed by a physician who holds a Drug Addiction Treatment Act (DATA) waiver. This means only qualified healthcare providers can submit it.
- Accurate Patient Information: Ensure that all fields are filled out correctly, including patient details like Member ID#, name, phone number, and diagnosis. Mistakes can lead to delays.
- Drug Information: Specify the medication requested clearly, whether it's Suboxone SL Film or buprenorphine SL Tab, along with the dosages. This section is critical for approval.
- Psycho-social Counseling: Document the psychosocial counseling history accurately. Include the last session date and confirm the patient's compliance, as this information will be scrutinized.
- Urine Drug Screen: A current urine drug screen must accompany the form. Make sure this is obtained and included, as it is mandatory for submission.
- Signature and Submission: The physician must sign and submit the form via fax to the WellCare Pharmacy. Verify the fax number is correct for successful processing.
Browse Other Templates
Nj Certified Payroll - Fringe benefits may be reported as cash payments or contributions to benefit plans, as required.
License Suspension Nc - A declaration of truthfulness must be signed by the supervising driver.
Tele Placement - Documents room number and admit date for tracking patient location.