Fill Out Your Superior Prior Authorization Form
The Superior Prior Authorization form is an essential document designed to facilitate patient access to prescribed medications while ensuring that those medications are medically necessary. This request form is tailored specifically for Superior Health Plan members in Texas, and it is important to note that it should not be used for biopharmaceutical products. When completing the form, healthcare providers need to provide crucial information, including their details, the member’s identification and medication history, as well as specific information about the drug being requested. Each form addresses one drug request, ensuring clarity in processing. Additionally, a section is dedicated to justifying the request with pertinent clinical information that demonstrates medical necessity. To streamline the process, it is crucial that all necessary documentation is included, as incomplete forms can result in delays. Providers will receive a response within 24 hours of submitting the request, making it imperative to provide accurate and comprehensive information upfront. By understanding the critical elements captured in the Superior Prior Authorization form, patients, and healthcare providers can work together efficiently to navigate the approval process for essential medications.
Superior Prior Authorization Example
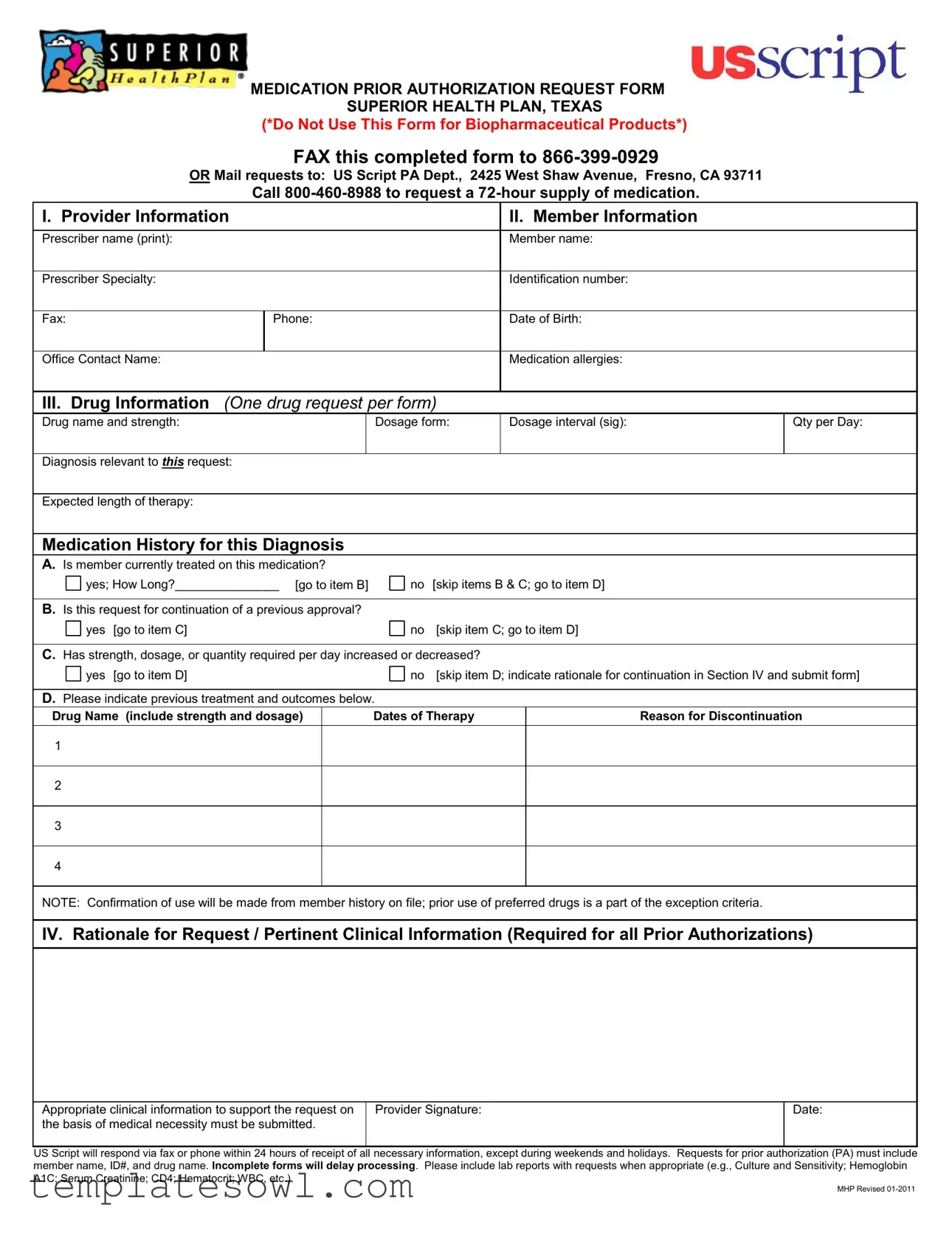
MEDICATION PRIOR AUTHORIZATION REQUEST FORM SUPERIOR HEALTH PLAN, TEXAS
(*Do Not Use This Form for Biopharmaceutical Products*)
FAX this completed form to
OR Mail requests to: US Script PA Dept., 2425 West Shaw Avenue, Fresno, CA 93711
Call
I. Provider Information |
|
II. Member Information |
|
|
|
Prescriber name (print): |
|
Member name: |
|
|
|
Prescriber Specialty: |
|
Identification number: |
|
|
|
Fax: |
Phone: |
Date of Birth: |
|
|
|
Office Contact Name: |
|
Medication allergies: |
|
|
|
III.Drug Information (One drug request per form)
Drug name and strength:
Dosage form:
Dosage interval (sig):
Qty per Day:
Diagnosis relevant to THIS request:
Expected length of therapy:
Medication History for this Diagnosis
A.Is member currently treated on this medication?
yes; How Long?_______________ [go to item B] |
no [skip items B & C; go to item D] |
B.Is this request for continuation of a previous approval?
yes [go to item C] |
no [skip item C; go to item D] |
C.Has strength, dosage, or quantity required per day increased or decreased?
yes [go to item D] |
|
no [skip item D; indicate rationale for continuation in Section IV and submit form] |
D.Please indicate previous treatment and outcomes below.
Drug Name (include strength and dosage)
Dates of Therapy
Reason for Discontinuation
1
2
3
4
NOTE: Confirmation of use will be made from member history on file; prior use of preferred drugs is a part of the exception criteria.
IV. Rationale for Request / Pertinent Clinical Information (Required for all Prior Authorizations)
Appropriate clinical information to support the request on the basis of medical necessity must be submitted.
Provider Signature:
Date:
US Script will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends and holidays. Requests for prior authorization (PA) must include member name, ID#, and drug name. Incomplete forms will delay processing. Please include lab reports with requests when appropriate (e.g., Culture and Sensitivity; Hemoglobin A1C; Serum Creatinine; CD4; Hematocrit; WBC, etc.).
MHP Revised
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | This form is used to request prior authorization for medication from Superior Health Plan in Texas. It is not applicable for biopharmaceutical products. |
| Submission Methods | Completed forms can be faxed to 866-399-0929 or mailed to the US Script PA Department in Fresno, California. |
| Urgent Prescription Needs | For urgent medication needs, providers can call 800-460-8988 to request a 72-hour supply while the authorization is pending. |
| Required Information | The form requires detailed provider and member information, including medication history and rationale for the request related to medical necessity. |
| Response Time | After the necessary information is submitted, US Script will respond within 24 hours, excluding weekends and holidays. |
| Incomplete Requests | Forms that are incomplete will slow down the processing time, so it’s crucial to include all relevant information and documentation. |
Guidelines on Utilizing Superior Prior Authorization
Completing the Superior Prior Authorization form is crucial for obtaining the necessary approval for medications. Following the outlined steps ensures that all information is accurately submitted, facilitating a smoother process. This proactive approach helps avoid delays in accessing required treatments.
-
Fill out the Provider Information section:
- Print the prescriber's name.
- Indicate the prescriber's specialty.
- Provide the prescriber's fax number and phone number.
- List the office contact name.
-
Complete the Member Information section:
- Enter the member's full name.
- Include the member's identification number.
- Specify the member's date of birth.
- List any medication allergies.
-
Provide Drug Information:
- Write the drug name and strength.
- Choose the dosage form.
- Specify the dosage interval.
- Indicate the quantity per day.
- State the diagnosis relevant to the request.
- Estimate the expected length of therapy.
-
Detail the Medication History:
- Confirm if the member is currently treated on this medication and note the duration.
- If applicable, indicate if this request is for the continuation of a previous approval.
- If dosage has changed, specify the new strength, dosage, or quantity required.
- Provide previous treatment details, including drug name, dates of therapy, and reasons for discontinuation.
-
Fill in the Rationale for Request:
- Include relevant clinical information to support the request based on medical necessity.
-
Sign and date the form:
- The provider must sign the form and fill out the date of completion.
-
Submit the completed form:
- Fax the form to 866-399-0929 or mail it to: US Script PA Dept., 2425 West Shaw Avenue, Fresno, CA 93711.
- Contact 800-460-8988 to request a 72-hour supply of medication if necessary.
What You Should Know About This Form
What is the Superior Prior Authorization form used for?
The Superior Prior Authorization form is a document required for certain medications to determine whether a specific treatment is medically necessary before approval. This process helps ensure that prescribed drugs are covered by insurance and are appropriate for the member's needs. It’s important to note that this form should not be used for biopharmaceutical products.
How do I submit the form?
You can submit the completed Superior Prior Authorization form by faxing it to 866-399-0929 or mailing it to US Script PA Dept., 2425 West Shaw Avenue, Fresno, CA 93711. Always double-check to ensure all required sections are completed to avoid delays.
What information do I need to provide on the form?
The form requires detailed information about the provider, the member, and the specific medication request. You’ll need to include the prescriber’s name, member identification number, drug name, dosage, and diagnosis, among other details related to the member's treatment history.
Are there guidelines for filling out the medication history section?
Yes, in the medication history section, you should note whether the member is currently being treated with the requested medication, if this request relates to a continuation of a previous approval, and any changes to dosage or quantity. Furthermore, detailing past treatments and their outcomes can strengthen your request.
What happens after submission of the form?
Once the form is submitted, US Script will review the request. You can expect a response via fax or phone within 24 hours, provided all necessary information is included. Keep in mind that responses may be delayed during weekends and holidays.
What if I need a medication urgently?
If you require an urgent supply of medication, you can call 800-460-8988 to request a 72-hour supply while the prior authorization is being processed. This can provide immediate relief for critical situations while waiting for formal approval.
What happens if I submit an incomplete form?
An incomplete form may result in delays in processing your request. To avoid any setbacks, ensure that all sections are filled out thoroughly, particularly the rationale for the request and any pertinent clinical information that supports the need for the medication.
Is additional documentation needed?
Yes, when appropriate, it’s advisable to include lab reports with your submission. Documents such as Culture and Sensitivity reports, Hemoglobin A1C levels, or other relevant tests can substantiate the medical necessity of the requested medication.
What should I do if I have questions about the form?
If you have questions or need assistance while filling out the form, it is a good idea to reach out to the Superior Health Plan customer service or the prescriber’s office for guidance. They can provide clarity and support to ensure that your submission is correct and complete.
Common mistakes
Filling out the Superior Prior Authorization form correctly is crucial to ensure timely access to necessary medications. Many individuals make common mistakes that can delay approval. Here are eight frequent errors to avoid.
First, failing to provide complete provider and member information is a significant oversight. Every field, including the prescriber’s name, specialty, and contact information, must be filled out fully. Incomplete contact details can lead to unnecessary delays as the review team may struggle to reach the prescriber for clarifications.
Second, neglecting to enter the correct drug information can result in denial of the request. The drug name, strength, dosage form, and interval are critical details. If any of these elements are incorrect or missing, the authorization process will be hampered, leading to further delays in treatment.
Third, some individuals skip the medication history section, which is a vital part of the request. It is essential to specify whether the member is currently being treated with the medication and to detail past treatments, including reasons for discontinuation. Skipping this section can signal a lack of thoroughness in the treatment plan.
Fourth, misunderstanding the rationale for the request can cause issues. Providers must include appropriate clinical information that supports the medical necessity of the prescribed medication. Providing this context helps reviewers understand why this specific drug is required, avoiding the risk of denial based on insufficient justification.
Fifth, not submitting supporting documentation can severely impact the request. It is important to include pertinent lab reports and any other relevant clinical data. Omitting this can lead to additional requests for information, prolonging the approval process.
Sixth, some individuals forget the importance of indicating any changes in dosage or therapy. If there has been an increase or decrease in strength, dosage, or quantity per day, this information must be clearly stated. This oversight might result in the denial of the request if the reviewer thinks that the prescription does not align with prior approvals.
Seventh, incomplete rationale for the request often hinders approval. Providers must explain why continuation of therapy is necessary, especially if there hasn't been a change in dosage or medication. Failure to provide a comprehensive rationale can lead to confusion and potential rejection of the authorization.
Finally, individuals sometimes neglect to sign and date the form. An unsigned form cannot be processed. Ensuring that all sections are completed, including the provider’s signature, is essential for a smooth submission process.
By avoiding these common mistakes, individuals can help facilitate a more efficient authorization process, ensuring that patients receive the necessary medication in a timely manner.
Documents used along the form
When requesting medication through the Superior Prior Authorization form, additional forms and documents may be needed to streamline the approval process. Each serves a specific purpose in providing necessary information to support your request. Here’s a list of commonly used forms alongside the Superior Prior Authorization form:
- Patient Medical History Form: This form collects detailed background information on the patient's health conditions and previous treatments, which can provide context for the medication request.
- Healthcare Provider's Letter of Medical Necessity: A letter from the prescribing healthcare provider detailing why the requested medication is essential for the patient's treatment, including possible side effects of not using it.
- Clinical Documentation: This may include lab results, imaging studies, or any relevant clinical notes that support the need for the specific medication being requested.
- Formulary Exception Form: If the requested medication isn’t listed in the health plan's formulary, this form helps to petition for an exception due to medical necessity.
- Medication Reconciliation Form: A record used to ensure that the medications the patient is currently taking are considered, preventing potential drug interactions during treatment.
- Payer-Specific Authorization Form: Some insurance providers have their own forms that need to be filled out in addition to the Superior Prior Authorization form to meet their unique requirements.
- Patient Consent Form: A document obtaining consent from the patient for sharing medical information with the insurance provider and for proceeding with the proposed treatment.
- Progress Notes: Written documentation from the healthcare provider that reflects the patient's ongoing health status and the rationale for the medication being requested.
- Medication Administration Record (MAR): A log showing when medications were administered and any observed responses, which can help support the need for prior authorization.
- Appeal Letter: In case of a denial, this letter outlines the reasons for overturning the decision, along with the necessary argumentation and supporting documentation.
Using these forms alongside the Superior Prior Authorization form can help ensure a smoother approval process. Gathering and submitting comprehensive documentation increases the chances of a favorable response, ultimately benefiting patient care.
Similar forms
The Superior Prior Authorization form is similar to several other documents in the medical field. Here is a list of those similar forms:
- Medicaid Prior Authorization Request Form: Like the Superior form, this document is also used to request approval for specific medications based on medical necessity. Both require detailed patient and provider information.
- Medicare Part D Prior Authorization Form: This form is used for Medicare recipients to obtain prior approval for certain medications, similar to the process outlined in the Superior form.
- Insurance Pre-Authorization Form: This document is often needed for various medical services and treatments, requiring justification for the requested service, just as the Superior form does for medications.
- Drug Utilization Review (DUR) Form: This form helps assess medication usage based on established guidelines. It focuses primarily on ensuring patient safety and drug efficacy, paralleling the information collected on the Superior form.
- Critical Drug Review Request: This request is for specific drugs that may have higher risks. The process is similar to the Superior form, requiring a detailed clinical rationale.
- Medication Reconsideration Request: When there is a need to revisit a prior decision on medication coverage, this form collects patient history and prescriber feedback, akin to the requirements of the Superior form.
- Clinical Decision Support Request Form: Used by healthcare providers to seek additional support or second opinions on treatment options, this also echoes the detail-oriented nature of the Superior form.
Dos and Don'ts
When filling out the Superior Prior Authorization form, attention to detail is crucial. Here are four key do's and don'ts to ensure the process goes smoothly.
- Do double-check all personal information for accuracy, including the provider and member details.
- Do supply all required clinical information to support the medical necessity of the requested medication.
- Do send the completed form to the correct fax number or mailing address as specified.
- Do follow up with a phone call if you do not receive a response within 24 hours.
- Don't submit multiple drug requests on a single form; each request must be on its own form.
- Don't leave any sections of the form blank, as incomplete submissions will delay processing.
- Don't use this form for biopharmaceutical products, as it is not designed for that purpose.
- Don't forget to include any relevant lab reports when submitting your request, if applicable.
Misconceptions
Misconceptions about the Superior Prior Authorization form can lead to confusion and delays in medication approval. Here’s a list of common misunderstandings:
- This form can be used for any medication. The Superior Prior Authorization form is not intended for biopharmaceutical products. Ensure you're using the right form for your needs.
- Prior Authorization can be submitted without supporting information. Every request requires pertinent clinical information to justify the medical necessity, preventing unnecessary delays.
- Requests can be submitted without a prescriber signature. A valid prescriber signature is required on the form to authenticate the request and ensure accountability.
- The processing time is always 24 hours. While US Script aims to respond within 24 hours, this only applies if all necessary information is provided. Missing details can extend the timeline.
- Once the form is submitted, there's no need to follow up. Monitoring the request is advisable. If there are complications, following up with US Script can clarify status.
- Laboratory reports are optional. Including lab reports when relevant is strongly recommended. They provide critical evidence supporting the medical necessity.
- You can submit multiple drugs on one form. Only one drug request is permitted per form. This helps streamline the review process.
- All medications will be approved after submission. Approval is contingent upon meeting medical necessity criteria. Not every request will be granted.
- Incompleted forms are acceptable. Incomplete submissions will delay processing. Always ensure that all required fields are filled out before sending.
- The form can be mailed without a fax option. While mailing is an option, faxing the form to 866-399-0929 is often quicker and more reliable.
By understanding these misconceptions, users can more effectively navigate the prior authorization process and ensure timely approval for necessary medications.
Key takeaways
When it comes to navigating the Superior Health Plan's Prior Authorization process, certain key points can enhance understanding and increase efficiency. Below are four essential takeaways that can help streamline the completion and submission of the authorization request form.
- Accurate Information is Crucial: Always ensure that the provider and member information fields are filled out accurately. This includes the prescriber’s name, contact details, and the member's identification number. Mistakes in this area can introduce significant delays.
- One Drug Per Form: The form is designed for a single medication request. Submitting multiple requests for different drugs on one form can lead to confusion and potential rejection of the application.
- Document Previous Treatments: A section of the form requires you to outline any previous treatments and their outcomes. Providing robust clinical information enhances the likelihood of approval and ensures that the request is reviewed thoroughly.
- Timely Follow-Up: Once the form has been submitted, follow up within 24 hours if you have not received a response. Be aware that weekends and holidays may extend this timeline. Keeping communication lines open can help address any issues swiftly.
By keeping these takeaways in mind, users can better navigate the Prior Authorization process and foster a more efficient interaction with the Superior Health Plan.
Browse Other Templates
Texas Resale Certificate Instructions - The AP 201 1 form not only facilitates tax permits but also lays the groundwork for sustainable business practices.
Gic Canada Amount - Funds for the GIC can be transferred from any bank in India where you hold an account.
Heat Work Authorization,Spark Work Clearance,Flame Safety Permit,Thermal Work Approval,Welding and Cutting Permit,Open Flame Work Permit,Heat Generation Authorization,Fire Risk Assessment Form,Combustion Activity Permit,Fire Hazard Mitigation Permit - All personnel should understand their roles in ensuring safety during hot work.