Fill Out Your Tb Test Form
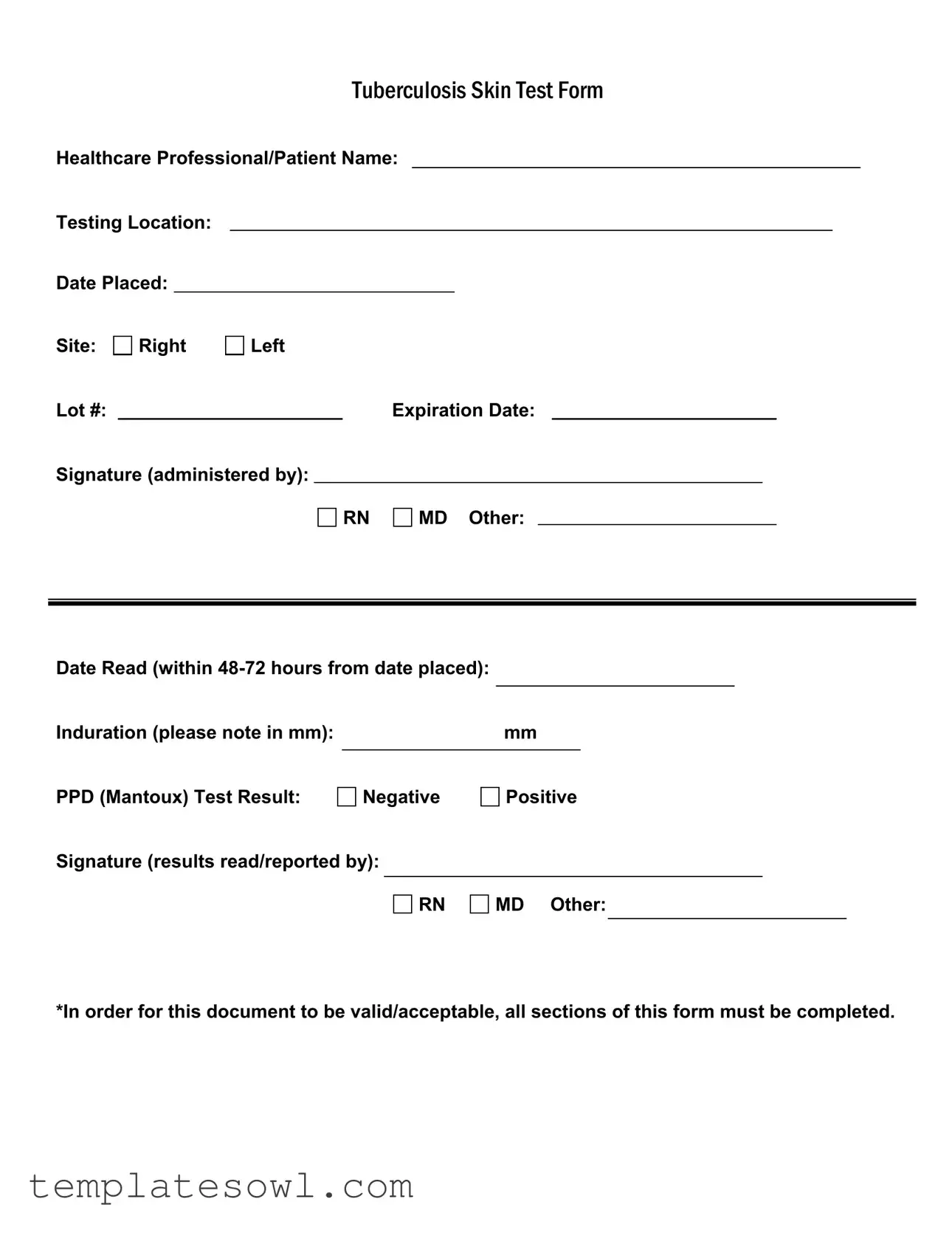
The Tuberculosis (TB) Skin Test Form is an essential document in identifying and assessing exposure to tuberculosis. This form plays a pivotal role in both healthcare settings and patient interactions, ensuring accurate communication between healthcare professionals and patients. Key sections include the names of the healthcare professional and patient, the testing location, as well as important dates such as when the test was placed and read. Additionally, it provides space to denote the exact site of the test—whether on the right or left arm—and critical details like the lot number and expiration date of the testing material. The healthcare professional administering the test must sign the form, indicating their qualifications, which may include a registered nurse (RN) or medical doctor (MD). To understand the test results, one must note the induration measurement in millimeters, followed by a clear indication of whether the PPD (Mantoux) test result is negative or positive. Lastly, the form requires a signature from the professional reading and reporting the results to establish accountability. It is crucial that all sections of this document are completed for it to be considered valid and acceptable in any medical context.
Tb Test Example
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose of the Form | This form is used to document the administration and results of the Tuberculosis (TB) skin test. |
| Required Information | All sections must be filled out, including patient and healthcare professional details, test placement, reading date, and results. |
| Testing Timeframe | The test must be read within 48-72 hours after placement for accurate results. |
| Test Result Interpretation | Results are categorized as negative or positive based on the measurement of induration in millimeters. |
| Governing Laws | Vary by state; many states follow regulations per the CDC and may require completion for school or employment-related health assessments. |
Guidelines on Utilizing Tb Test
After you complete the Tb Test form, the next steps involve submitting it to the appropriate healthcare professional. They will review the information and determine the results based on the test characteristics. Accurate completion of the form is essential for valid documentation.
- Write your name in the Healthcare Professional/Patient Name section.
- Fill in the Testing Location where the test is being conducted.
- Enter the Date Placed on the form, which is the date you receive the test.
- Indicate the injection Site of the test as either Right or Left.
- Record the Lot # of the test material used.
- Write the Expiration Date of the test material.
- Sign your name in the Signature (administered by) section where you will indicate if you are RN, MD, or Other.
- After the test has been read, enter the Date Read, which must be within 48-72 hours from the date placed.
- Note down the Induration size in millimeters (mm).
- Select the PPD (Mantoux) Test Result, marking it as Negative or Positive.
- Sign in the Signature (results read/reported by) section, indicating if you are RN, MD, or Other.
What You Should Know About This Form
What is the purpose of the TB Test form?
The TB Test form is used to record important information about the administration and results of a tuberculosis (TB) skin test, specifically the PPD or Mantoux test. This form captures key details such as the healthcare professional’s name, the testing location, dates, and test results. It helps ensure that the test is properly documented and can be referenced in future medical evaluations.
What information is required on the TB Test form?
To ensure the form is valid and acceptable, all sections must be completed. This includes providing the names of both the healthcare professional and patient, the testing location, and specific dates for when the test was placed and read. The form also requires details about the site of the injection, information about the lot and expiration date of the test solution, and signatures from the administering and reading professionals. Noting the induration measurement in millimeters is crucial for determining the result.
How quickly should the results of the TB test be read?
The results of the TB test should be read within 48 to 72 hours from the date the test was placed. It is important to adhere to this timeline because reading the test outside of this window may lead to inaccurate interpretation of the results. The induration—swelling at the test site—is measured in millimeters to determine whether the test result is negative or positive.
What does a positive result on the TB Test form signify?
A positive result on the TB Test form means that there is a significant induration at the test site, indicating a potential TB infection. However, it does not confirm active tuberculosis disease. A positive result may require further testing, such as a chest X-ray or additional laboratory tests, to determine if the individual has active TB or if they have been exposed to the bacteria at some point. It is important for healthcare providers to interpret the results in the context of the patient’s medical history and risk factors.
Common mistakes
Filling out the Tuberculosis (TB) Test form can seem straightforward, but there are common mistakes that people often make. First, leaving out critical information is a frequent issue. All sections of the form must be filled out for it to be valid. Omitting details like the name of the healthcare professional or the testing location can lead to delays and complications.
Another mistake is not paying attention to the dates. It’s essential to accurately record the date the test was placed and the date it’s read. The test results must be noted within 48-72 hours from the date placed. Failing to do this can result in inaccurate information and possible re-testing.
The handling of the result is also a point of concern. Some individuals incorrectly check the result box or do not fill in the induration measurement in millimeters. It’s important that the induration is correctly noted. This measurement is crucial in determining whether the test result is negative or positive.
Signature requirements should not be overlooked. The form must be signed by the administering healthcare professional, whether it’s an RN, MD, or other. Not providing a signature or using a title that isn’t indicated can lead to questions about your test's validity.
Many individuals confuse the interpretation of the PPD test result. Understanding the difference between a negative and a positive result is vital. Misunderstanding these terms could create unnecessary anxiety or lead to additional health checks if the results are not clear.
Lastly, if there’s any change in the testing protocols due to new health guidelines, make sure you are aware. Changes could affect how the form needs to be filled out or interpreted. Staying informed ensures that the form is completed accurately and helps in getting the right outcome regarding your health.
Documents used along the form
The Tuberculosis (TB) Test form is crucial for healthcare providers and patients to document the administration and results of the TB skin test. Alongside this form, several other documents are often necessary for comprehensive health assessments and to maintain proper records. Below is a list of related forms that are commonly used in conjunction with the TB test.
- Patient Medical History Form: This form gathers essential information about a patient's previous illnesses, treatments, surgeries, and medications. It helps healthcare providers understand the patient’s health background, which could influence the TB test results.
- Informed Consent Form: Before administering the TB test, healthcare providers often require patients to sign an informed consent form. This document ensures that the patient understands the procedure, its purpose, and any potential risks associated with the test.
- TB Test Log: A TB Test Log is used by healthcare facilities to track all administered TB tests. It typically includes patient identification, test dates, result status, and healthcare provider information, ensuring an organized system for recordkeeping.
- Follow-Up Assessment Form: Should a patient test positive for TB, a follow-up assessment form becomes necessary. This document aids in documenting the patient’s symptoms, treatment plan, and further necessary evaluations to monitor the patient's health status.
These supporting forms work in tandem with the TB Test form to create a thorough health profile. It is important to ensure that all documentation is completed accurately to provide optimal patient care and maintain compliance with health regulations.
Similar forms
-
Vaccination Record Form: This document contains personal details about the patient, alongside the vaccination dates and types received. Like the TB Test form, it requires signatures from healthcare providers, ensuring the authenticity of the vaccination information.
-
Health Assessment Form: Patients provide information about their medical history and current health status on this form. Similar to the TB Test form, it requires input from healthcare professionals to evaluate potential health risks and ensure all sections are completed for accuracy.
-
Consent Form for Medical Procedures: This document captures the patient's agreement to undergo specific medical procedures. Both forms must be signed by the patient and a healthcare provider, attesting to the informed consent nature and ensuring all necessary sections are filled out.
-
Patient Referral Form: This document facilitates the transfer of a patient from one healthcare provider to another. It includes essential details about the patient and the reason for referral, mirroring the TB Test form’s emphasis on complete information and signatures from involved healthcare professionals.
-
Medication Administration Record (MAR): The MAR tracks medication doses given to a patient. This form is similar to the TB Test form in that it requires accurate documentation, including signatures from healthcare professionals to validate that medications were administered or tests were performed.
Dos and Don'ts
When filling out the TB Test form, it is important to follow specific guidelines to ensure accuracy and compliance. Here are some dos and don'ts to consider:
- Do complete all sections of the form before submission.
- Do use clear and legible handwriting when filling out the form.
- Do double-check that the date placed and date read are within the required timeframe.
- Do ensure the appropriate healthcare professional signs the form.
- Don't leave any sections blank; incomplete forms may be rejected.
- Don't use correcting fluid or tape on the form; this could lead to confusion.
- Don't input the induration measurement without measuring accurately in mm.
- Don't forget to sign the results section after they are read and reported.
Misconceptions
Understanding the TB Test form is crucial for both healthcare professionals and patients. However, several misconceptions often arise. Below is a clarification of these misconceptions.
- Misconception 1: The TB test can be interpreted immediately.
- Misconception 2: Only healthcare professionals can fill out the form.
- Misconception 3: The test is only valid if a doctor administers it.
- Misconception 4: The lot number is not necessary.
- Misconception 5: No signature is needed for the results to be accepted.
- Misconception 6: Induration size is not important.
- Misconception 7: A negative result means no risk of tuberculosis.
- Misconception 8: The form is not important once the test is administered.
- Misconception 9: The TB test only needs to be done once.
The TB test requires between 48 to 72 hours for the results to be accurately read.
While a healthcare professional administers the test, patients should also provide essential information, such as their name and the testing location.
A registered nurse (RN) can also administer the TB test, making it valid regardless of who performs the test.
The lot number and expiration date are important to ensure the validity and effectiveness of the test materials used.
For the form to be complete, signatures from those administering the test and reading the results must be included.
The size of the induration in millimeters is critical in determining whether the test result is positive or negative.
A negative result can indicate no current infection, but it does not eliminate the possibility of exposure or future infection.
The form must be retained for record-keeping and future reference, as it contains essential information related to the test.
Depending on risk factors and exposure, individuals may need periodic retesting, and each test requires a new form.
Key takeaways
When filling out the TB Test form, keep these key takeaways in mind:
- Complete All Sections: It's crucial to fill out every part of the form. An incomplete form may not be considered valid.
- Provide Accurate Details: Make sure to include the patient's name, testing location, and the date the test was placed. This ensures proper record-keeping.
- Induration Measurement: The measurement of induration is vital. Record this value in millimeters to interpret the test result accurately.
- Timely Reading: Test results must be read 48 to 72 hours after placement. Ensure that this timeframe is followed so that the results are valid.
- Professional Signatures: The form requires signatures from healthcare professionals for both administration and result interpretation. This adds credibility to the document.
Browse Other Templates
Bank Application Form - Fill in your home phone number to provide an alternate contact method.
Rmv Driving Test - Ensure your Service Type section lists the desired CDL endorsements clearly.