Fill Out Your Treatment Plan Form
Creating a comprehensive Treatment Plan is essential for effective patient care, as it guides both the therapist and the patient throughout the treatment journey. This form captures important goals that should be specific, objective, and measurable, helping to track progress over time. Each goal is paired with estimated time frames for completion, fostering accountability. Collaboration is key; the patient’s input is crucial, and their agreement, as shown by a signature, solidifies mutual understanding. The form also addresses various goals, such as reducing risk factors and alleviating major symptoms. It focuses on coping strategies and stabilizing crises, ensuring a well-rounded approach to treatment. Planned interventions are listed, reflecting the patient’s active participation in their own healing process. Additionally, the Treatment Plan outlines potential referrals and emphasizes the use of personal strengths and community resources. By documenting obstacles to change and estimating timeframes for each goal, the plan remains adaptable, making it a vital tool in the therapeutic relationship.
Treatment Plan Example
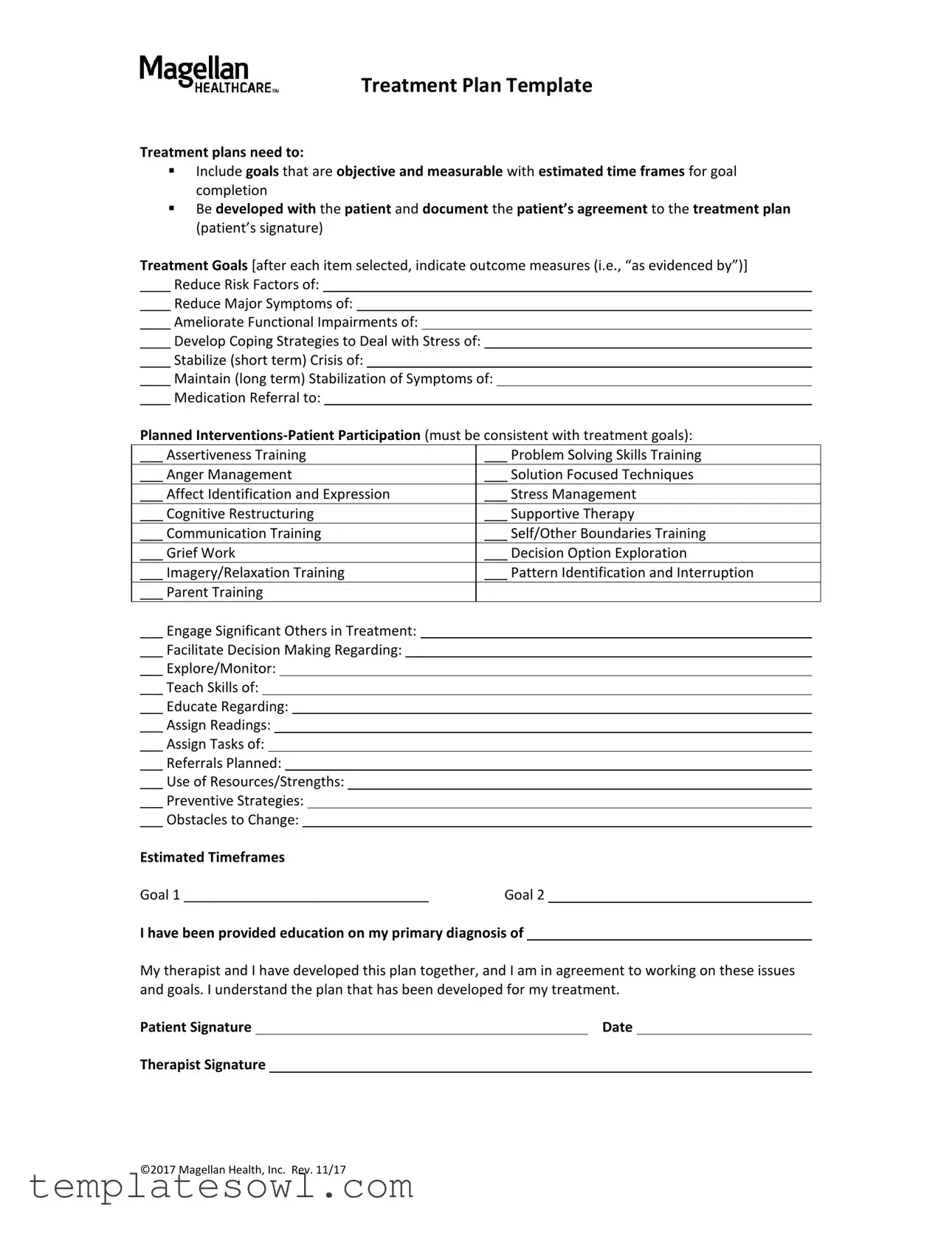
Treatment Plan Template
Treatment plans need to:
▪Include goals that are objective and measurable with estimated time frames for goal completion
▪Be developed with the patient and document the patient’s agreement to the treatment plan (patient’s signature)
Treatment Goals [after each item selected, indicate outcome measures (i.e., “as evidenced by”)]
____ Reduce Risk Factors of:
____ Reduce Major Symptoms of:
____ Ameliorate Functional Impairments of:
____ Develop Coping Strategies to Deal with Stress of:
____ Stabilize (short term) Crisis of:
____ Maintain (long term) Stabilization of Symptoms of:
____ Medication Referral to:
Planned
___ Assertiveness Training |
___ Problem Solving Skills Training |
|||||||||||||
___ Anger Management |
___ Solution Focused Techniques |
|||||||||||||
___ Affect Identification and Expression |
___ Stress Management |
|||||||||||||
___ Cognitive Restructuring |
___ Supportive Therapy |
|||||||||||||
___ Communication Training |
___ Self/Other Boundaries Training |
|||||||||||||
___ Grief Work |
___ Decision Option Exploration |
|||||||||||||
___ Imagery/Relaxation Training |
___ Pattern Identification and Interruption |
|||||||||||||
___ Parent Training |
|
|
|
|||||||||||
___ Engage Significant Others in Treatment: |
|
|
|
|
||||||||||
___ Facilitate Decision Making Regarding: |
|
|
|
|
||||||||||
___ Explore/Monitor: |
|
|
|
|
||||||||||
___ Teach Skills of: |
|
|
|
|
||||||||||
___ Educate Regarding: |
|
|
|
|
||||||||||
___ Assign Readings: |
|
|
|
|
||||||||||
___ Assign Tasks of: |
|
|
|
|
||||||||||
___ Referrals Planned: |
|
|
|
|
||||||||||
___ Use of Resources/Strengths: |
|
|
|
|
||||||||||
___ Preventive Strategies: |
|
|
|
|
||||||||||
___ Obstacles to Change: |
|
|
|
|
||||||||||
Estimated Timeframes |
|
|
|
|||||||||||
Goal 1 ________________________________ |
Goal 2 |
|
|
|||||||||||
I have been provided education on my primary diagnosis of
My therapist and I have developed this plan together, and I am in agreement to working on these issues and goals. I understand the plan that has been developed for my treatment.
Patient Signature |
|
Date |
Therapist Signature
©2017 Magellan Health, Inc. Rev. 11/17
Form Characteristics
| Fact Name | Details |
|---|---|
| Objective and Measurable Goals | Treatment plans must contain goals that are both objective and measurable. Each goal should include an estimated time frame for completion. |
| Patient Involvement | The treatment plan should be developed collaboratively with the patient, ensuring that their perspective is included in the process. |
| Patient Signature | Documentation of the patient's agreement to the treatment plan requires their signature. This confirms their commitment to the outlined goals and interventions. |
| Types of Goals | Goals may include reducing risk factors, managing symptoms, and developing coping strategies, among others. Each goal should have corresponding outcome measures. |
| Therapeutic Interventions | Possible interventions involve various techniques like assertiveness training, stress management, and cognitive restructuring to support patient participation. |
| Referral Plans | Plans may include referrals for medication or other resources. The treatment plan must clarify how these resources fit into overall patient care. |
| Obstacles to Change | Identifying potential obstacles to treatment is essential. Addressing these issues can improve the likelihood of achieving treatment goals. |
| Governing Laws | Depending on the state, different laws apply to treatment plans, including confidentiality and consent requirements. Familiarity with state-specific regulations is crucial. |
Guidelines on Utilizing Treatment Plan
After completing the Treatment Plan form, the next step involves reviewing it with the patient to ensure clarity and cooperation. This collaboration is essential for establishing a shared commitment to the outlined goals. It is important that both the therapist and the patient understand the objectives and agree on the steps to be taken. Now, you can proceed to fill out the form by following these steps.
- Start by documenting the patient's primary diagnosis in the designated section.
- Clearly outline the treatment goals. Each goal should be objective and measurable.
- After selecting each goal, provide specific outcome measures by indicating how success will be demonstrated (e.g., “as evidenced by”).
- Identify interventions that the patient will participate in, ensuring they align with the treatment goals.
- Encircle or check the relevant interventions such as coping strategies, skills training, or supportive therapies that will aid in the patient's treatment.
- Facilitate communication regarding any resources, referrals, or education that may be necessary for the patient’s progress.
- Discuss and document any potential obstacles to change that may impact achieving treatment goals.
- Estimate timeframes for each goal, specifying how long you anticipate each goal will take to complete.
- Finally, ensure both the therapist and patient sign and date the form to confirm agreement and understanding of the treatment plan.
What You Should Know About This Form
What is a Treatment Plan form and why is it important?
A Treatment Plan form is a crucial document used in therapy settings to outline the specific goals and interventions tailored for a patient. It is important because it helps create a structured approach to treatment, ensuring that both the therapist and the patient are aligned on the objectives of care. This shared understanding enhances collaboration and accountability, ultimately contributing to better outcomes. By detailing measurable goals and desired outcomes, the plan also facilitates progress tracking throughout the treatment process.
What key components must be included in a Treatment Plan?
A comprehensive Treatment Plan must include specific, objective, and measurable goals that come with estimated time frames for completion. It should also document the collaborative development of the plan between the therapist and the patient, requiring the patient’s signature to confirm their agreement. The plan encompasses identified goals—such as reducing symptoms or developing coping strategies—along with the planned interventions and the patient's participation in those interventions. Regular review and updates to the plan are essential to address changing needs and progress.
How are goals determined in a Treatment Plan?
Goals in a Treatment Plan are determined through discussions between the therapist and the patient. The process involves assessing the patient's current situation, identifying key issues that need to be addressed, and understanding the patient’s personal objectives. This collaborative approach enables the development of goals that are not only relevant but also motivating to the patient. Each goal should be quantifiable, allowing both parties to track progress effectively. For each goal, the treatment plan will detail specific outcome measures to demonstrate progress.
What role does the patient play in the Treatment Plan?
The patient's role in the Treatment Plan is central. They actively participate in the formulation of the goals and interventions. This involvement ensures that the treatment aligns with their needs and preferences, enhancing motivation and commitment to the process. Additionally, by signing the plan, the patient demonstrates their agreement and understanding of the proposed treatment. Ongoing communication and feedback from the patient are vital as the treatment plan evolves, ensuring it remains relevant and effective over time.
How often should a Treatment Plan be reviewed and updated?
A Treatment Plan should be reviewed regularly, typically every few weeks or at significant treatment milestones. The frequency of these reviews can depend on the individual patient's needs, the severity of their condition, and the pace of their progress. During these reviews, the therapist and patient will assess progress toward the established goals, discuss any challenges, and make adjustments as necessary. This ongoing evaluation ensures that the treatment remains aligned with the patient's evolving circumstances and goals, ultimately supporting a more effective therapeutic process.
Common mistakes
Filling out a Treatment Plan form can be intricate due to its detailed requirements. Many individuals make common mistakes that can hinder the effectiveness of the plan. One major mistake is failing to set specific and measurable goals. Goals must outline exactly what is to be achieved and include quantifiable outcomes. For instance, instead of stating a goal as "reduce anxiety," it should specify "reduce anxiety levels by 30% within three months," making it more tangible.
Another frequent error involves neglecting to collaborate with the patient in developing the treatment plan. It is essential that the patient’s insights and preferences guide the plan’s creation. A lack of patient involvement can lead to a disconnection from their treatment, making them less likely to comply with the outlined goals and interventions.
Additionally, many individuals incorrectly assume that the estimated timeframes for goal completion are optional. Timeframes not only provide a clear timeline for achieving goals, but they also promote accountability. This oversight can result in indefinite delays in treatment progress, reducing the effectiveness of the therapeutic process.
Some people may also overlook the importance of documenting the patient’s agreement to the treatment plan through their signature. Without this signature, there is no formal acknowledgment that the patient understands and agrees to the terms, which could lead to misunderstandings about the treatment path.
In the context of planned interventions, a common mistake is selecting too many options without prioritization. While it may seem beneficial to incorporate various strategies, focusing on a few key interventions can lead to more effective treatment. This approach ensures that the patient is not overwhelmed and allows for a more structured progression during therapy.
Lastly, individuals often forget to address potential obstacles to change within the Treatment Plan. Identifying challenges up front allows for the development of strategies to overcome these barriers. Failure to consider these obstacles might lead to disruptions in the treatment process, undermining the progress towards achieving set goals.
Documents used along the form
The Treatment Plan form is an essential tool in healthcare settings, especially when working collaboratively with patients. However, several other documents are often used to complement the Treatment Plan, ensuring that all aspects of patient care are documented clearly and efficiently. Below is a list of these documents, each serving a unique function in the treatment process.
- Assessment Form: This document evaluates the patient’s current mental and physical health status. It gathers baseline information, including medical history, presenting problems, and psychosocial factors that could impact treatment.
- Progress Notes: These are written records that detail a patient's journey throughout treatment. Progress Notes document the patient’s advancements, setbacks, and any modifications made to the Treatment Plan based on ongoing assessments.
- Consent for Treatment: This form confirms that the patient understands and agrees to the proposed treatment, acknowledging the potential risks and benefits. It often includes legal information about patient rights.
- Referral Form: A Referral Form is used when a patient requires services beyond the capabilities of the primary care provider. This document outlines the reasons for referral and provides necessary patient information to the specialist.
- Discharge Summary: Upon completion of treatment, the Discharge Summary provides a comprehensive overview of the patient’s progress, final treatment outcomes, and recommendations for ongoing care or follow-up.
- Intake Form: This foundational document is completed during the initial visit. It collects vital information such as demographics, insurance details, and a detailed account of the patient's concerns to create a personalized treatment approach.
- Medication Management Form: This document tracks prescribed medications, dosages, and the patient's adherence to the medication regimen. It serves as a critical tool for managing pharmacological treatments effectively.
- Family Involvement Plan: This plan outlines how family members will participate in the patient’s treatment, detailing their roles and responsibilities, which can enhance the effectiveness of the overall treatment.
- Behavioral Intervention Plan: A structured plan focusing on specific behavioral issues. It details strategies to address these behaviors and includes measurable goals for tracking progress over time.
Each of these documents plays a vital role in supporting the Treatment Plan. Together, they provide a comprehensive framework for understanding the patient's needs, tracking progress, and optimizing treatment outcomes.
Similar forms
- Individualized Education Plan (IEP): Similar to a treatment plan, an IEP outlines specific educational goals tailored to a student with special needs, ensuring measurable goals and regular assessments.
- Treatment Summary Report: This document summarizes the progress of a patient during treatment, including goals achieved and future objectives, maintaining a focus on measurable outcomes.
- Behavioral Intervention Plan (BIP): A BIP details specific interventions for managing challenging behaviors, similar to how a treatment plan addresses symptoms and functional impairments.
- Care Plan: This document outlines healthcare interventions for patients, emphasizing collaboration with the patient and ensuring they agree with the proposed plan.
- Recovery Plan: A recovery plan sets out steps for individuals recovering from mental health issues, paralleling the treatment plan’s structure of goals and interventions tailored to the patient’s needs.
- Psychosocial Rehabilitation Plan: This plan focuses on rebuilding the skills and supports needed for patients to function in their communities, similar to the treatment plan's focus on functional improvements and coping strategies.
- Client Service Plan: Used in social work, this document identifies the needs of clients and outlines specific goals, aligning closely with the treatment plan’s goal-setting framework.
- Wellness Plan: A wellness plan focuses on lifestyle changes and interventions aimed at improving overall health and well-being, much like how a treatment plan targets various aspects of a patient’s health.
- Risk Management Plan: This plan identifies potential risks and outlines strategies to mitigate them, which parallels the treatment plan's goal of reducing risk factors for patients.
Dos and Don'ts
When filling out the Treatment Plan form, consider the following dos and don’ts to ensure clarity and compliance.
- Do include specific and measurable goals that have estimated time frames.
- Do collaborate with the patient to develop the treatment plan.
- Do obtain the patient's signature to confirm their agreement with the plan.
- Do indicate outcome measures for each selected treatment goal.
- Do use clear language that is easy for the patient to understand.
- Don't leave goals vague or subjective; specify what success looks like.
- Don't exclude the patient from the planning process.
- Don't forget to document the patient's understanding of the plan.
- Don't use technical jargon that might confuse the patient.
- Don't overlook the need for follow-up on the treatment goals.
Misconceptions
Understanding the Treatment Plan form is essential for both patients and healthcare providers. However, several misconceptions surround this important document. Below are some of the common misunderstandings:
- Treatment plans are only for mental health treatments. This is false. Treatment plans can be used in various healthcare settings, addressing physical, behavioral, and mental health needs.
- Only the therapist develops the treatment plan. In reality, treatment plans must be developed collaboratively with the patient to ensure their needs and goals are adequately addressed.
- All goals in a treatment plan must be achieved within a short time frame. While some goals may have specific deadlines, many are ongoing, reflecting the complexity of recovery.
- A treatment plan is a fixed document and cannot be changed. Treatment plans are dynamic and can be adjusted as necessary to reflect the patient's progress and changing needs.
- Patients do not need to sign the treatment plan. Patients must agree to the plan, which is typically documented with their signature to signify their understanding and commitment.
- The treatment plan is only for the healthcare provider's reference. This is incorrect; the plan should be a shared tool, guiding both the provider and the patient in their work together.
- All interventions listed in the treatment plan must be utilized. Not all interventions are appropriate for every patient. Providers should personalize approaches based on the patient's specific needs.
- Once the treatment plan is created, no follow-up is necessary. Regular follow-ups are vital for assessing progress, making adjustments, and ensuring the plan remains relevant.
- Completing the treatment plan automatically leads to recovery. While the treatment plan is a crucial step, recovery is a personalized journey that involves ongoing commitment and effort from the patient.
- Only doctors can understand the treatment plan. Treatment plans are designed to be clear and accessible for patients, allowing them to engage fully in their treatment process.
By dispelling these misconceptions, patients and providers can work together more effectively, resulting in better health outcomes.
Key takeaways
Here are key takeaways for effectively filling out and utilizing the Treatment Plan form:
- Set Clear Goals: The treatment plan should include goals that are both objective and measurable. This ensures clarity in what the patient aims to achieve.
- Involve the Patient: Development of the treatment plan requires collaboration. The patient's active participation is essential, and their agreement must be documented through a signature.
- Identify Specific Areas: An effective plan addresses specific issues such as risk factors, major symptoms, functional impairments, and coping strategies.
- Outline Interventions: List the planned interventions that align with treatment goals. This helps in providing clear guidance on the steps to be taken during therapy.
- Utilize Outcome Measures: After identifying each treatment goal, indicate outcome measures. This can include phrases like "as evidenced by," which help track progress.
- Set Time Frames: Each goal should have an estimated time frame for completion. This keeps the treatment process on track and allows for timely adjustments if needed.
- Address Barriers: Identify any obstacles to change the patient may face. This allows for strategic planning to overcome these barriers.
- Continuous Review: The treatment plan is a living document. Regularly review and adjust it based on the patient's progress and changing needs.
Browse Other Templates
Bmo Harris Payment - This form is for setting up direct deposit into your BMO Harris Bank account.
Maryland Tax Withholding Exemption Form,MD Income Tax Adjustment Certificate,Maryland Withholding Adjustment Form,Maryland Income Tax Exemption Application,Employee Tax Exemption Certificate,Maryland Tax Allowance Worksheet,Maryland Income Tax Withho - The tax relief provided by claiming exemptions can help increase take-home pay throughout the year.
Ifta 21 - This application monitors fuel tax liability accurately across state lines, aiding businesses in compliance.