Fill Out Your Texas Dwc069 Form
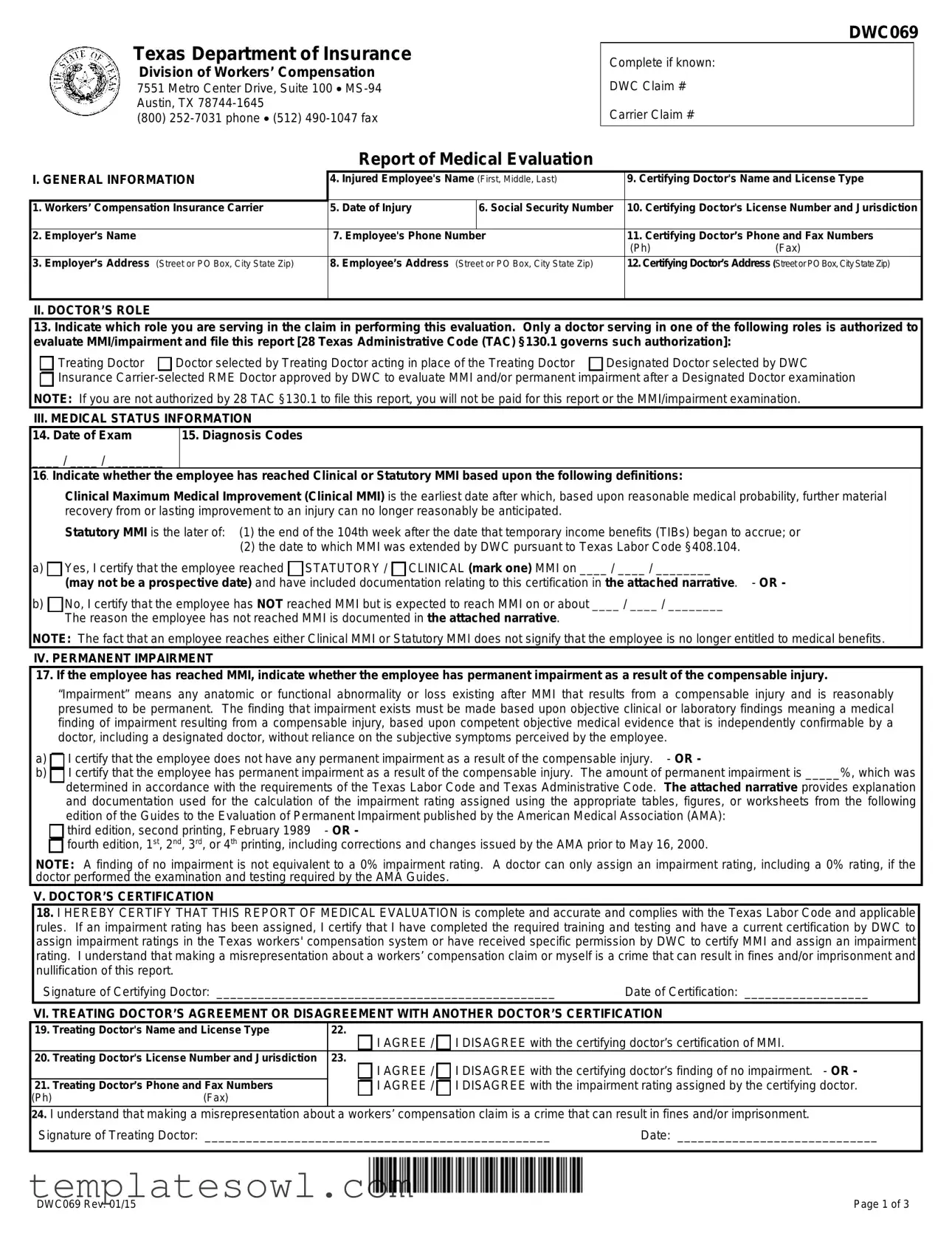
The Texas DWC069 form, officially known as the Report of Medical Evaluation, plays a critical role in the Texas workers’ compensation system. This document is primarily used to communicate essential medical information regarding an injured employee’s condition and progress, particularly in relation to Maximum Medical Improvement (MMI) and any potential permanent impairments as a result of their injury. The form requires detailed information regarding the injured worker, including their name, contact information, and specifics about their employer and insurance carrier. Moreover, the certifying doctor must clarify their relationship to the case—whether they are the treating doctor, a designated doctor assigned by the Texas Department of Insurance, or an insurance carrier-selected doctor. This distinction is vital since only certain types of doctors are authorized to evaluate MMI or assign impairment ratings. The form also captures the doctor’s findings, including diagnoses, medical status, and whether the employee has reached MMI. A certification section is included, where the doctor confirms the accuracy of their report, affirming their qualifications to make such determinations. Additionally, the form addresses the treating doctor’s ability to agree or disagree with the findings made by the certifying doctor, further emphasizing collaboration and communication among medical providers in the workers' compensation process. The completion and filing of the DWC069 form are essential not only for compliance with Texas labor regulations but also for ensuring that injured employees receive the benefits they deserve based on their medical assessments.
Texas Dwc069 Example
Texas Department of Insurance
Division of Workers’ Compensation
7551 Metro Center Drive, Suite 100
(800)
Report of Medical Evaluation
DWC069
Complete if known:
DWC Claim #
Carrier Claim #
I. GENERAL INFORMATION |
4. Injured Employee's Name (First, Middle, Last) |
|||
|
|
|
|
|
1. |
Workers’ Compensation Insurance Carrier |
5. |
Date of Injury |
6. Social Security Number |
|
|
|
|
|
2. |
Employer’s Name |
7. Employee's Phone Number |
|
|
|
|
|
|
|
3. |
Employer’s Address (Street or PO Box, City State Zip) |
8. |
Employee’s Address (Street or PO Box, City State Zip) |
|
|
|
|
|
|
9.Certifying Doctor's Name and License Type
10.Certifying Doctor's License Number and Jurisdiction
11.Certifying Doctor’s Phone and Fax Numbers
(Ph)(Fax)
12.Certifying Doctor’s Address (Street or PO Box, City State Zip)
II. DOCTOR’S ROLE
13.Indicate which role you are serving in the claim in performing this evaluation. Only a doctor serving in one of the following roles is authorized to evaluate MMI/impairment and file this report [28 Texas Administrative Code (TAC) §130.1 governs such authorization]:
Treating Doctor |
Doctor selected by Treating Doctor acting in place of the Treating Doctor |
Designated Doctor selected by DWC |

 Insurance
Insurance
III. MEDICAL STATUS INFORMATION
14. Date of Exam |
15. Diagnosis Codes |
____ / ____ / ________ |
|
16. Indicate whether the |
employee has reached Clinical or Statutory MMI based upon the following definitions: |
Clinical Maximum Medical Improvement (Clinical MMI) is the earliest date after which, based upon reasonable medical probability, further material recovery from or lasting improvement to an injury can no longer reasonably be anticipated.
Statutory MMI is the later of: (1) the end of the 104th week after the date that temporary income benefits (TIBs) began to accrue; or
(2)the date to which MMI was extended by DWC pursuant to Texas Labor Code §408.104.
a) Yes, I certify that the employee reached
Yes, I certify that the employee reached  STATUTORY /
STATUTORY /  CLINICAL (mark one) MMI on ____ / ____ / ________
CLINICAL (mark one) MMI on ____ / ____ / ________
(may not be a prospective date) and have included documentation relating to this certification in the attached narrative. - OR -
b) No, I certify that the employee has NOT reached MMI but is expected to reach MMI on or about ____ / ____ / ________
No, I certify that the employee has NOT reached MMI but is expected to reach MMI on or about ____ / ____ / ________
The reason the employee has not reached MMI is documented in the attached narrative.
NOTE: The fact that an employee reaches either Clinical MMI or Statutory MMI does not signify that the employee is no longer entitled to medical benefits.
IV. PERMANENT IMPAIRMENT
17. If the employee has reached MMI, indicate whether the employee has permanent impairment as a result of the compensable injury.
“Impairment” means any anatomic or functional abnormality or loss existing after MMI that results from a compensable injury and is reasonably presumed to be permanent. The finding that impairment exists must be made based upon objective clinical or laboratory findings meaning a medical finding of impairment resulting from a compensable injury, based upon competent objective medical evidence that is independently confirmable by a doctor, including a designated doctor, without reliance on the subjective symptoms perceived by the employee.
a) I certify that the employee does not have any permanent impairment as a result of the compensable injury. - OR -
I certify that the employee does not have any permanent impairment as a result of the compensable injury. - OR -
b) I certify that the employee has permanent impairment as a result of the compensable injury. The amount of permanent impairment is _____%, which was determined in accordance with the requirements of the Texas Labor Code and Texas Administrative Code. The attached narrative provides explanation and documentation used for the calculation of the impairment rating assigned using the appropriate tables, figures, or worksheets from the following
I certify that the employee has permanent impairment as a result of the compensable injury. The amount of permanent impairment is _____%, which was determined in accordance with the requirements of the Texas Labor Code and Texas Administrative Code. The attached narrative provides explanation and documentation used for the calculation of the impairment rating assigned using the appropriate tables, figures, or worksheets from the following
edition of the Guides to the Evaluation of Permanent Impairment published by the American Medical Association (AMA): 
 third edition, second printing, February 1989 - OR -
third edition, second printing, February 1989 - OR -

 fourth edition, 1st, 2nd, 3rd, or 4th printing, including corrections and changes issued by the AMA prior to May 16, 2000.
fourth edition, 1st, 2nd, 3rd, or 4th printing, including corrections and changes issued by the AMA prior to May 16, 2000.
NOTE: A finding of no impairment is not equivalent to a 0% impairment rating. A doctor can only assign an impairment rating, including a 0% rating, if the doctor performed the examination and testing required by the AMA Guides.
V. DOCTOR’S CERTIFICATION
18.I HEREBY CERTIFY THAT THIS REPORT OF MEDICAL EVALUATION is complete and accurate and complies with the Texas Labor Code and applicable rules. If an impairment rating has been assigned, I certify that I have completed the required training and testing and have a current certification by DWC to assign impairment ratings in the Texas workers' compensation system or have received specific permission by DWC to certify MMI and assign an impairment rating. I understand that making a misrepresentation about a workers’ compensation claim or myself is a crime that can result in fines and/or imprisonment and nullification of this report.
|
Signature of Certifying Doctor: _________________________________________________ |
Date of Certification: __________________ |
|||
|
VI. TREATING DOCTOR’S AGREEMENT OR DISAGREEMENT WITH ANOTHER DOCTOR’S CERTIFICATION |
||||
19. |
Treating Doctor's Name and License Type |
22. |
|
||
|
|
|
|
I AGREE / I DISAGREE with the certifying doctor’s certification of MMI. |
|
20. |
Treating Doctor's License Number and Jurisdiction |
|
23. |
|
|
|
|
|
|
I AGREE / I DISAGREE with the certifying doctor’s finding of no impairment. - OR - |
|
21. |
Treating Doctor’s Phone and Fax Numbers |
|
I AGREE / I DISAGREE with the impairment rating assigned by the certifying doctor. |
||
(Ph) |
(Fax) |
|
|
||
24.I understand that making a misrepresentation about a workers’ compensation claim is a crime that can result in fines and/or imprisonment.
Signature of Treating Doctor: __________________________________________________ |
Date: _____________________________ |
DWC069 Rev. 01/15 |
Page 1 of 3 |
DWC069
Frequently Asked Questions
Report of Medical Evaluation (DWC
INSTRUCTIONS FOR DOCTORS:
Who can file the DWC
Treating Doctor: Doctor chosen by the employee who is primarily responsible for employee's
Doctor Selected by Treating Doctor: Doctor selected by the treating doctor to evaluate permanent impairment and Maximum Medical Improvement (MMI). This doctor acts in the place of the treating doctor. Such a doctor must be selected if the treating doctor is not authorized to certify MMI or assign an impairment rating in those cases in which the employee has permanent impairment. An authorized treating doctor may also choose to select another doctor to perform the evaluation/certification.
Designated Doctor: Doctor selected by the Texas Department of Insurance, Division of Workers’ Compensation (DWC) to resolve a question over MMI or permanent impairment.
Insurance
AUTHORIZATION: In addition to the requirement of acting in an eligible role, 28 Texas Administrative Code §130.1 provides the following requirements:
Employee has permanent impairment: Only a doctor certified by DWC to assign impairment ratings or who receives specific
permission by exception granted by DWC is authorized to certify MMI and to assign an impairment rating.
Employee does not have permanent impairment: A doctor not certified or exempted from certification by DWC is only authorized to determine whether an employee has permanent impairment and, in the event that the employee has no impairment, certify MMI.
INVALID CERTIFICATION: Certification by a doctor who is not authorized is invalid.
Under what circumstances and when am I required to file the DWC
If the employee has reached MMI, you must file the DWC
Where do I file the form?
The DWC
the insurance carrier;
the treating doctor (if a doctor other than the treating doctor files the report);
DWC;
injured employee; and
injured employee’s representative (if any).
The report must be filed by facsimile or electronic transmission unless an exception applies. The specific requirements are shown below. To file this form with DWC, fax to (512)
|
|
Insurance Carrier |
|
Treating Doctor |
|
|
|
DWC |
|
|
|
|
|
|
Designated Doctor |
fax or |
fax or |
||
|
|
|
|
|
Treating Doctor |
|
|
|
fax or |
Doctor Selected by Treating Doctor |
|
fax or |
not provided these numbers; then |
|
Insurance |
|
|
|
by other verifiable means |
Injured Employee
Injured Employee’s Representative
fax or
fax or
Do I have to maintain documentation regarding the examination and report?
The certifying doctor must maintain the original copy of the report and narrative and documentation of the following:
date of the examination;
date any medical records necessary to make the certification of MMI were received, and from whom the medical records were received; and
date, addresses, and means of delivery that required reports were transmitted or mailed by the certifying doctor.
Where can I find more information about the Report of Medical Evaluation?
See 28 TAC §130.1 through §130.4 and §130.6 for the complete requirements regarding the filing of this report, including required documentation. The complete text of these rules is available on the Texas Department of Insurance website at www.tdi.texas.gov/wc/rules/index.html. If you have additional questions, call
DWC069 Rev. 01/15 |
Page 2 of 3 |
DWC069
IMPORTANT INFORMATION FOR INJURED EMPLOYEES:
What if I disagree with the doctor's certification of Maximum Medical Improvement (MMI) and/or permanent impairment rating for my workers' compensation claim?
If this is the first evaluation of your MMI and/or permanent impairment, you or your representative may dispute:
the certification of MMI; and/or
the assigned impairment rating.
To file the dispute, contact your local DWC field office or call
the appointment of a designated doctor (DD), if one has not been appointed; or
a Benefit Review Conference (BRC).
Important Note: Your dispute must be filed within 90 days after the written notice is delivered to you or the certification of MMI and/or the assigned impairment rating may become final.
NOTE: With few exceptions, upon your request, you are entitled to be informed about the information DWC collects about you; receive and review the information (Government Code, §§552.021 and 552.023); and have DWC correct information that is incorrect (Government Code, §559.004).
DWC069 Rev. 01/15 |
Page 3 of 3 |
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | The DWC069 form is used for reporting medical evaluations regarding an injured employee's Maximum Medical Improvement (MMI) and permanent impairment. |
| Governing Law | The form is governed by 28 Texas Administrative Code (TAC) §130.1 and related laws under the Texas Labor Code. |
| Roles in Claims | Authorized individuals include the treating doctor, a doctor selected by the treating doctor, a designated doctor, or an insurance carrier-selected doctor. |
| Certification Requirements | Only doctors certified by DWC may assign impairment ratings and certify MMI according to the Texas Labor Code. |
| Filing Deadline | The DWC069 must be filed no later than the seventh working day after the certifying examination or receipt of necessary medical information. |
| Disagreement Process | Employees can dispute the certification of MMI or assigned impairment ratings within 90 days of receiving the certification notice. |
| Where to File | The completed form must be submitted to the insurance carrier, the treating doctor, DWC, the injured employee, and their representative. |
| Documentation Maintenance | Doctors must keep the original report, the narrative, and any documentation related to the examination and report submission. |
| Important Note for Employees | Employees are entitled to access the information collected about them by DWC and can request corrections for any inaccuracies. |
| Contact Information | For additional inquiries, individuals can call the Texas Department of Insurance at 1-800-372-7713, Option #3. |
Guidelines on Utilizing Texas Dwc069
Filling out the Texas DWC069 form is an important step in dealing with a workers’ compensation claim. It plays a critical role in reporting the medical evaluation results related to an injured employee. Accuracy is essential, as any discrepancies can lead to complications with the claim process. Here’s how to complete this form effectively:
- Start by accessing the form. Ensure you have the latest version of the DWC069 from the Texas Department of Insurance website.
- In the first section, fill in the general information. This includes the workers’ compensation insurance carrier, the employer’s details, and the injured employee’s personal information like name, date of injury, and social security number.
- Next, provide the certifying doctor’s name, license type, phone and fax numbers, and address. This identifies the medical professional responsible for the evaluation.
- Indicate the doctor's role in the evaluation. Mark if the doctor is the treating doctor, a doctor selected by the treating doctor, a designated doctor, or an insurance carrier-selected RME doctor.
- Enter the date of the exam and the diagnosis codes related to the injury. This section documents the medical condition of the employee.
- State whether the employee has reached Maximum Medical Improvement (MMI). Choose between clinical or statutory MMI and provide the date, ensuring it is not a future date.
- If the employee has reached MMI, indicate whether there is permanent impairment. Provide the impairment percentage if applicable, along with an explanation using the AMA Guides to Permanent Impairment.
- In the certification section, ensure the certifying doctor signs and dates the form. This certifies that the report is complete and accurate.
- If there is an agreement or disagreement between the treating doctor and the certifying doctor, include the treating doctor's details and their agreement or disagreement with the certifications noted.
- Finally, make sure to submit the completed form. It should be sent to the insurance carrier, the treating doctor (if applicable), the DWC, and any representatives associated with the injured employee's case.
Please remember to keep a copy of the filled form and any supporting documentation for your records. For additional questions or assistance, don’t hesitate to reach out to the Texas Department of Insurance or your legal representative.
What You Should Know About This Form
What is the Texas DWC069 Form, and what is its purpose?
The Texas DWC069 Form, known as the Report of Medical Evaluation, is a document used by healthcare providers to assess an injured employee's medical condition in the context of workers' compensation. This form captures crucial information regarding the employee’s maximum medical improvement (MMI) status and any permanent impairment resulting from the workplace injury. Completing this form accurately is vital as it impacts the benefits the injured employee may receive, including medical coverage and compensation for lost wages.
Who is authorized to file the DWC069 Form?
Only specific types of doctors can file the DWC069 Form. Authorized individuals include the treating doctor, a doctor selected by the treating physician to act in their place, a designated doctor appointed by the Texas Department of Insurance, and an insurance carrier-selected Required Medical Examination (RME) doctor. Each of these roles has its responsibilities, especially concerning certification of MMI and impairment ratings, which must adhere to particular guidelines established by the Texas Administrative Code.
What should I do if I disagree with the doctor's certification of MMI or permanent impairment?
If you, as an injured employee, do not agree with the certification of your MMI or the assigned impairment rating, you have the right to dispute this assessment. This can be initiated by contacting your local Division of Workers’ Compensation (DWC) field office or calling their information line. It’s crucial to file this dispute within 90 days from the date you receive written notice about the certification, or otherwise the certification may become final.
What are the filing requirements for the DWC069 Form?
The DWC069 Form must be filed no later than the seventh working day following the examination, specifically when the employee has reached MMI. The filing should be directed to the insurance carrier, the treating doctor (if applicable), the DWC, the injured employee, and their representative. It's important to note that the submission should generally occur via fax or electronic transmission unless stated otherwise. This ensures that all parties receive the necessary information in a timely manner.
How can I find more information about the DWC069 Form or related rules?
Comprehensive information on the DWC069 Form and associated rules can be found in the Texas Administrative Code (TAC) under sections 130.1 through 130.4 and 130.6. For direct access to these documents, visit the Texas Department of Insurance's official website. Additionally, should you have any further inquiries, help is readily available by calling the DWC at their toll-free number.
Common mistakes
Filling out the Texas DWC069 form accurately is essential to ensure timely processing of workers' compensation claims. However, there are common errors that can complicate matters. Awareness of these mistakes can significantly improve the accuracy of the form.
One frequent mistake is failing to provide complete and correct general information. This includes the injured employee's name, Social Security number, and date of injury. Omitting any of these details can lead to delays. Each piece of information is crucial for identifying the claim and processing it effectively. Double-checking this section can save time and effort down the road.
Another common error involves the certifying doctor's role. It's vital to indicate the correct role being served, whether as a treating doctor or a designated doctor. If an incorrect role is marked, the certification may be deemed invalid, impacting the employee's benefits. Understanding the roles defined in the form can help to avoid this critical mistake.
As the form progresses, many individuals overlook the need for proper diagnoses and codes. Entering incorrect diagnosis codes, or failing to include them at all, can result in a mismatch between the medical evaluation and the claim. Providing accurate information here is key to supporting the evaluation of the employee's condition.
Certainly, another prevalent mistake is the improper indication of MMI status. When certifying if the employee has reached either Clinical or Statutory MMI, it is essential to mark the correct option and to provide an appropriate date. Incorrectly marking this can create confusion regarding the employee's eligibility for further treatment or benefits. Be diligent in this part of the form to prevent misunderstandings.
Also, the section concerning permanent impairment often suffers from misinterpretations. Some may inaccurately certify that no impairment exists, even when objective clinical findings suggest otherwise. It's essential to base this certification on thorough evaluation and reliable findings following the recommended guidelines from the American Medical Association. Ensure that the rationale for the impairment rating is clearly documented and justified in the narrative.
Lastly, the doctor’s certification section often contains inconsistencies. The certifying doctor must ensure that the signature and date correspond accurately. Misrepresenting the completion of necessary training can lead to liability issues. It is crucial to ensure all aspects of this section are filled out accurately to uphold the integrity of the report and the process surrounding it.
Documents used along the form
The Texas DWC069 form serves as a critical document in the workers' compensation process by reporting the medical evaluation related to a claim. Accompanying this form, there are several other documents which are typically involved. Each of these plays a significant role in ensuring proper administration and processing of claims within the Texas workers’ compensation system.
- DWC Form 1: This form is the Employer's First Report of Injury. It must be filed by the employer within a specific timeframe after an injury occurs. This report provides initial information about the injury, including details about the employee, the nature of the injury, and the circumstances surrounding the incident. Timely submission is vital as it kickstarts the claims process.
- DWC Form 73: This is the Notification of Insurance Coverage form. It confirms that an employer has workers' compensation insurance. It provides necessary details about the employer's insurance carrier including policy numbers, which is essential for maintaining compliance and ensuring employees are covered under the appropriate policy.
- DWC Form 046: Known as the Request for Benefit Review Conference, this form is used when there is a disagreement regarding the benefits awarded in connection to a claim. Filing this form initiates a formal process to address disputes and seek resolution, providing both parties a fair opportunity to present their case.
- DWC Form 33: This is the Employee's Claim for Compensation form. It allows the injured worker to formally apply for compensation benefits. This document should be completed carefully as it outlines the specifics of the claim, including dates, nature of injury, and the type of benefits sought.
- DWC Form 68: This form serves as the Impairment Rating Certificate. It summarizes the medical evaluation results that determine the extent of the impairment due to the work-related injury. A certified doctor fills this out, and it is foundational in calculating the benefits entitled to the injured employee based on their level of impairment.
Each of these forms works hand-in-hand with the DWC069 to create a comprehensive picture of the employee's claim. Understanding how they all relate can help ensure adherence to necessary procedures and accurate processing of claims in Texas. Staying organized and informed about these documents is essential for all parties involved in the workers’ compensation process.
Similar forms
The Texas DWC069 form, known as the Report of Medical Evaluation, shares similarities with several other documents used in the context of workers' compensation and medical evaluations. Below is a list of nine such documents and how they relate to the DWC069:
- DWC Form-053: This form is used for reporting a designated doctor's examination findings. Like the DWC069, it certifies the employee's maximum medical improvement status and can include impairment ratings.
- DWC Form-069B: This is a follow-up form for disputing MMI or impairment ratings. It is similar in purpose, as it addresses the same issues of medical evaluation and impairment determination.
- DWC Form-042: This is the Notice of No Insurance form that serves to notify parties of a lack of insurance coverage. While it focuses on insurance status, it is used in the broader context of workers' compensation documentation.
- DWC Form-007: The Request for Designated Doctor Examination form is used to appoint a designated doctor for disputes over MMI or impairment ratings. This form interacts closely with the DWC069 in cases where there are conflicting evaluations.
- DWC Form-046: This form, the Carrier's Report of Medical Evaluation, is submitted by insurance carriers after an evaluation. It provides similar information regarding MMI and any permanent impairment findings.
- DWC Form-033: The Employee's Notice of Injury or Occupational Disease form consolidates injury information. While primarily focused on the injury report, it is often filed alongside medical evaluations like the DWC069.
- DWC Form-041: The Application for Benefits Review Conference is more formal in nature and addresses disputes over benefits. It can stem from disputes arising from evaluations reported on the DWC069.
- DWC Form-061: This form is used for the report of a dispute regarding MMI or impairment ratings. It also deals directly with the findings documented in the DWC069.
- DWC Form-021: Used for filing a workers’ compensation claim or appeal, this document complements the DWC069 by providing additional context about the injury, condition, and challenges faced by the employee.
These documents often work together within the workers' compensation system, creating a comprehensive framework for managing medical evaluations, insurance claims, and recovery outcomes.
Dos and Don'ts
When filling out the Texas DWC069 form, it is important to be thorough and accurate. Here is a list of things to do and avoid:
- Do ensure all personal information is complete, especially names and dates.
- Do follow the specific instructions for the role you are serving regarding the evaluation.
- Do include documentation and narratives as required by the form.
- Do maintain copies of the form and any related documentation for your records.
- Do file the form on time, adhering to the deadlines specified.
- Don't leave any sections blank unless specified; fill out all relevant areas.
- Don't make any misrepresentations regarding the worker’s compensation claim, as it may lead to serious consequences.
Misconceptions
Misconception 1: Only the Treating Doctor can file the DWC069 form.
This is not entirely true. While the Treating Doctor is often responsible for the evaluation, other doctors, such as the Designated Doctor or an RME Doctor chosen by the insurance carrier, can also file the form if authorized.
Misconception 2: The DWC069 form only pertains to injuries that have permanent impairment.
The form can also be used to certify Maximum Medical Improvement (MMI) even if no permanent impairment is present. It is crucial for documenting the employee's medical status throughout the workers' compensation claim process.
Misconception 3: A doctor’s certification of MMI means the employee will no longer receive treatment.
This is misleading. Certification of MMI does not indicate that medical benefits stop. Employees may still be entitled to medical care even after MMI is reached, depending on their condition.
Misconception 4: The form can be submitted after an indefinite period following the evaluation.
The DWC069 form must be filed within seven working days after the exam or receipt of necessary medical information. Delays can jeopardize the validity of the certification.
Misconception 5: Filing the DWC069 form is optional for the certifying doctor.
This is incorrect. It is mandatory for the doctor to file the form if the employee is evaluated and found to have reached MMI or has a permanent impairment. Failure to do so can result in complications with claims processing.
Misconception 6: All doctors can assign impairment ratings.
Only doctors specifically authorized by the Texas Department of Insurance can assign impairment ratings. Those not certified will have limited authority in the evaluation process.
Misconception 7: Disagreeing with a doctor's evaluation has no practical implications.
In fact, if there is disagreement with an MMI or impairment rating, the affected employee must act quickly. They have 90 days to dispute the evaluation, or the rating may become final. Taking prompt action is essential to ensuring a fair review of the case.
Key takeaways
Here are key takeaways regarding the Texas DWC069 form:
- The form must be completed by authorized doctors, such as treating doctors or designated doctors.
- It requires specific information about the injured employee, including name, date of injury, and healthcare provider details.
- Coding for diagnoses is essential, based on objective clinical findings of impairment.
- The certification of Maximum Medical Improvement (MMI) must be based on clinical or statutory definitions and cannot be future-dated.
- A healthcare provider must maintain proper documentation relating to the evaluation and the filing of the DWC069 form.
- Submission of the form must occur within set timelines, specifically no later than seven working days following the evaluation.
- If an employee disagrees with the evaluation, they must act within 90 days to dispute the MMI certification or impairment rating to avoid finalization.
Understanding these points will help ensure proper use and compliance with the DWC069 form in Texas workers' compensation cases.
Browse Other Templates
Public Title Portal - Fees for processing the MVT 20-1 application must be paid in certified funds.
What Time Does Paychex Direct Deposit Hit - Review your information for accuracy before submission.