Fill Out Your Texas Pre Authorization Request Form
Navigating the complexities of healthcare can be daunting, particularly when it comes to the intricacies of medication coverage. In Texas, the Pre Authorization Request Form serves a vital role in ensuring that patients receive the medications they need while adhering to the rules set forth by Medicaid. This form is specifically designed for Global Prescription Exceptions, helping healthcare providers communicate necessary information clearly and efficiently. It includes crucial details like the patient's name, ID, and the prescribed drug, as well as the physician's contact information. Moreover, the form features important questions that guide prescribers through the authorization process, determining eligibility based on factors such as FDA approval, previous treatment failures, and dosing guidelines. Understanding how to accurately complete this form not only streamlines the approval process but also helps ensure that patients receive timely access to their prescribed therapies, ultimately contributing to better health outcomes.
Texas Pre Authorization Request Example
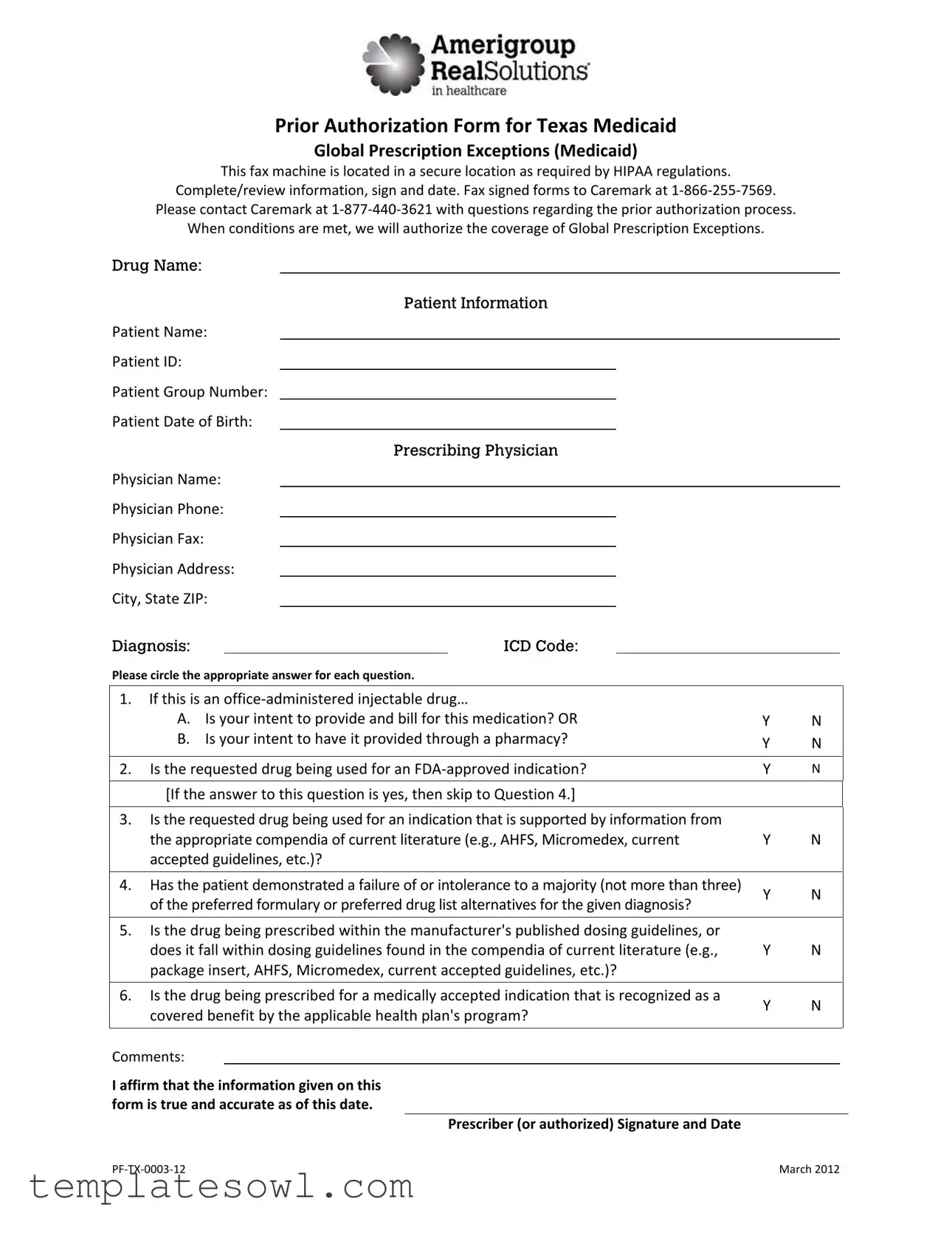
Prior Authorization Form for Texas Medicaid
Global Prescription Exceptions (Medicaid)
This fax machine is located in a secure location as required by HIPAA regulations.
Complete/review information, sign and date. Fax signed forms to Caremark at 1‐866‐255‐7569.
Please contact Caremark at 1‐877‐440‐3621 with questions regarding the prior authorization process.
When conditions are met, we will authorize the coverage of Global Prescription Exceptions.
Drug Name:
Patient Name:
Patient ID:
Patient Group Number: Patient Date of Birth:
Physician Name:
Physician Phone:
Physician Fax:
Physician Address: City, State ZIP:
Patient Information
Prescribing Physician
Diagnosis: |
|
ICD Code: |
Please circle the appropriate answer for each question.
1. |
If this is an office‐administered injectable drug… |
|
|
|
A. Is your intent to provide and bill for this medication? OR |
Y |
N |
|
B. Is your intent to have it provided through a pharmacy? |
Y |
N |
|
|
||
|
|
|
|
2. |
Is the requested drug being used for an FDA‐approved indication? |
Y |
N |
|
[If the answer to this question is yes, then skip to Question 4.] |
|
|
|
|
|
|
3.Is the requested drug being used for an indication that is supported by information from
the appropriate compendia of current literature (e.g., AHFS, Micromedex, current |
Y |
N |
|
accepted guidelines, etc.)? |
|
|
|
|
|
|
|
4. Has the patient demonstrated a failure of or intolerance to a majority (not more than three) |
Y |
N |
|
of the preferred formulary or preferred drug list alternatives for the given diagnosis? |
|||
|
|
5.Is the drug being prescribed within the manufacturer's published dosing guidelines, or
does it fall within dosing guidelines found in the compendia of current literature (e.g., |
Y |
N |
|
package insert, AHFS, Micromedex, current accepted guidelines, etc.)? |
|
|
|
|
|
|
|
6. Is the drug being prescribed for a medically accepted indication that is recognized as a |
Y |
N |
|
covered benefit by the applicable health plan's program? |
|||
|
|
Comments:
I affirm that the information given on this form is true and accurate as of this date.
Prescriber (or authorized) Signature and Date
PF‐TX‐0003‐12 |
March 2012 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The Texas Pre Authorization Request form is used to obtain prior authorization for Global Prescription Exceptions under Texas Medicaid. |
| Submission Method | Signed forms can be faxed to Caremark at the designated fax number: 1-866-255-7569. |
| Contact Information | For inquiries about the prior authorization process, call Caremark at 1-877-440-3621. |
| HIPAA Compliance | The form is faxed from a secure location, adhering to HIPAA regulations to protect patient information. |
| Required Information | The form requires complete patient and prescribing physician information, including diagnosis and relevant codes. |
| Regulatory Framework | This form is governed by Texas Medicaid regulations and federal healthcare laws regarding prior authorizations. |
| Signature Requirement | A signature from the prescriber or an authorized representative is necessary, affirming the truth and accuracy of the submitted information. |
Guidelines on Utilizing Texas Pre Authorization Request
To proceed with your Texas Pre Authorization Request form, careful attention to detail is essential. Completing this form accurately will help ensure a smooth submission process to Caremark for the requested authorization.
- Begin by entering the Drug Name at the top of the form.
- Fill in the Patient Name, Patient ID, Patient Group Number, and Patient Date of Birth.
- Provide the Physician Name, Physician Phone, Physician Fax, Physician Address, City, State, ZIP.
- Document the Prescribing Physician Diagnosis and the corresponding ICD Code.
- Respond to question 1 by circling either Y for yes or N for no.
- If you answered Y to question 1, move to question 2. Circle Y or N for whether the requested drug is FDA-approved.
- If you answered N to question 2, answer question 3 similarly.
- Proceed to question 4 and indicate your response.
- Answer question 5 by circling either Y or N.
- For question 6, indicate your answer.
- In the comments section, provide any additional relevant information.
- Sign and date the form at the bottom to affirm the accuracy of the provided information.
- Fax the signed form to Caremark at 1‐866‐255‐7569.
If you have any questions during the process, reach out to Caremark at 1‐877‐440‐3621 for assistance.
What You Should Know About This Form
What is the Texas Pre Authorization Request form?
The Texas Pre Authorization Request form is a document used to request prior authorization for certain medications under the Texas Medicaid program. Specifically, it’s focused on Global Prescription Exceptions, allowing healthcare providers to obtain approval before prescribing specific drugs, ensuring patients have access to necessary treatments while conforming to Medicaid guidelines.
Who needs to complete the form?
This form should be completed by healthcare providers who intend to prescribe medications that require prior authorization for their patients enrolled in Texas Medicaid. It is crucial that the provider gathers all relevant patient and medical information before submission.
How do I submit the completed form?
Once you have completed the form, fax it to Caremark at 1-866-255-7569. Ensure that all required fields are accurately filled out, and the form is signed and dated. Failure to provide complete information can lead to delays in authorization.
What information is required on the form?
The form requires detailed patient and physician information, such as the drug name, diagnosis, relevant ICD code, and the intent for administering the drug (either in-office or through a pharmacy). Be thorough—accuracy is key for a smooth process.
What factors are considered for drug approval?
The approval process takes several factors into account, such as whether the drug is being used for an FDA-approved indication, if alternative treatments have been exhausted, and adherence to dosing guidelines as per current medical literature and manufacturer instructions.
What should I do if I have questions during the process?
If you have questions about filling out the form or the prior authorization process itself, you can contact Caremark at 1-877-440-3621. They are equipped to assist with any inquiries you may have, ensuring you understand how to navigate the process effectively.
What happens after the form is submitted?
After submission, Caremark will review the information. If the documented conditions are met, they will grant the prior authorization so that the requested medication can be dispensed under Texas Medicaid. Expect a prompt response, but be prepared for the possibility of needing additional documentation if requested.
What is the significance of HIPAA compliance in this form?
The form is designed to be submitted via a secure fax machine, which adheres to HIPAA regulations. This compliance is critical as it protects the privacy and security of patient information throughout the authorization process. Keeping patient data secure must always remain a top priority.
Common mistakes
When filling out the Texas Pre Authorization Request form, it's important to be aware of common mistakes that can lead to delays or denials in processing. One significant error is failing to provide complete patient information. Each section, from the Patient Name to the Patient ID, must be thoroughly filled out. Incomplete data can result in confusion or miscommunication with the healthcare provider.
Another mistake to avoid is not answering the questions clearly. For instance, when asked whether the requested drug is for an FDA-approved indication, be sure to circle “Y” for yes or “N” for no. Ambiguity in responses can stall the approval process. It is crucial to answer all questions directly and honestly to ensure the request is processed promptly.
Additionally, many people forget to check the medication dosing guidelines. Question 5 specifically asks if the prescription aligns with manufacturer guidelines or accepted dosages. Neglecting this can lead to requests being denied. Always consult the relevant compendia or package insert to confirm that the prescribed drug is being administered according to appropriate medical standards.
There’s a tendency to overlook the necessity for supporting documentation. If the drug is being used for an indication not specifically FDA-approved, providing additional information from reputable literature is essential. Failing to include this can detract from the strength of the request and may cause it to be rejected outright.
Furthermore, individuals often forget to include personal contact details for the prescribing physician. The Physician Name, Phone, and Fax fields must be accurate to facilitate communication. This ensures that any follow-up questions can be addressed without unnecessary delays.
Lastly, many people neglect to double-check their signature and the date. The final affirmation of truth in the information provided is a critical step. Without the prescriber’s signature and the respective date, the form might be considered incomplete and rejected. Diligently reviewing each element of the form before submission can save time and effort in the long run.
Documents used along the form
The Texas Pre Authorization Request form is an important document for securing coverage for specific medications under Texas Medicaid. It serves to collect essential information about the patient and the prescribed drug. However, this form is often accompanied by other related documents that provide additional context or fulfill specific requirements of the authorization process. Below are common forms and documents used alongside the Texas Pre Authorization Request form.
- Texas Medicaid Enrollment Form: This document is used for patients who are seeking to enroll in Texas Medicaid. It captures personal, financial, and health information necessary for determining eligibility.
- Clinical Information Summary: This summary includes detailed medical history and current treatment plan. It helps clarify why a specific drug is necessary for the patient’s care.
- Drug Utilization Review (DUR) Report: Patients may need to submit a DUR report, which evaluates medication therapy for appropriateness, safety, and effectiveness in light of the patient's overall health and other medications.
- Statement of Medical Necessity: This document outlines why a particular medication is medically necessary for the patient. It often includes evidence from medical literature or guidelines supporting the use of the drug.
- Preferred Drug List (PDL): This list may accompany the pre-authorization request to show which medications are preferred by Medicaid and to identify alternatives that the patient may have tried.
In summary, while the Texas Pre Authorization Request form is crucial for obtaining medication coverage, accompanying documents further elucidate the patient's medical needs and treatment history. Each of these supporting documents plays a vital role in the approval process, ensuring a comprehensive evaluation by the healthcare plan.
Similar forms
- Prior Authorization Form for Medicare Advantage Plans: Similar to the Texas Pre Authorization Request form, this document is required to obtain approval for specific services or medications before they are provided to ensure coverage under Medicare Advantage plans.
- Prior Authorization Request for Commercial Health Insurance: This request form serves a similar purpose of obtaining prior approval for medications and treatments, ensuring that requested services meet the insurer's guidelines again, mirroring the intent of the Texas form.
- Pharmacy Benefits Manager (PBM) Prior Authorization Form: This document works analogously, as it is used to establish medical necessity for certain prescription medications covered under a specific pharmacy benefits plan.
- Outpatient Pre-Certification Request Form: This form is required for outpatient procedures and tests to verify that the treatments meet established clinical guidelines and are covered by the patient's health plan, closely paralleling the Texas Pre Authorization Request form.
- Provider Enrollment Forms: These forms may be required to register with various health plans, ensuring compliance with required protocols for prior authorization, thereby aligning with the objectives of the Texas form.
- Medical Necessity Form: Often requested by insurance providers, this document establishes that the requested treatment or service is essential for the patient’s well-being, akin to the medical necessity validation sought in the Texas Pre Authorization Request form.
Dos and Don'ts
When filling out the Texas Pre Authorization Request form, it’s essential to follow specific guidelines to ensure accuracy and efficiency. Here are some important dos and don’ts to keep in mind.
- Do double-check all the information you provide.
- Do sign and date the form before submission.
- Do ensure that you have circled the correct answers for each question.
- Do confirm that the drug is for an FDA-approved indication.
- Don’t leave any sections blank; every part must be completed.
- Don’t forget to fax the signed form to the correct number: 1‐866‐255‐7569.
Filling out this form accurately is crucial in obtaining the necessary authorizations. If you have questions, remember that contacting Caremark at 1‐877‐440‐3621 can provide further assistance.
Misconceptions
Understanding the Texas Pre Authorization Request form is essential for patients and healthcare providers alike. Unfortunately, several misconceptions about this form can lead to confusion. Here are ten common misunderstandings clarified:
- Misconception 1: The form is only for urgent cases.
- Misconception 2: Only doctors can submit the form.
- Misconception 3: All drugs require prior authorization.
- Misconception 4: Once submitted, the form guarantees approval.
- Misconception 5: There is no need for documentation of previous treatments.
- Misconception 6: If the drug is FDA-approved, it will automatically be approved.
- Misconception 7: The form can be submitted via email.
- Misconception 8: Patients will know immediately if their request has been approved.
- Misconception 9: Only Texas residents can use this form.
- Misconception 10: There are no penalties for submitting incorrect information.
The Texas Pre Authorization Request form is not limited to urgent situations. It can be used for any prescription that requires prior approval, regardless of the urgency.
While the prescribing physician typically submits the form, other authorized personnel can also complete it on their behalf with the proper documentation.
Not every medication requires prior authorization. Only specific drugs that are classified under the Texas Medicaid guidelines must go through this approval process.
Submitting the form does not ensure approval. Coverage is contingent upon meeting certain criteria laid out by the Medicaid system.
Documentation is crucial. The form asks whether the patient has shown intolerance to other medications, so medical history should be prepared in advance.
Even if a drug is FDA-approved, it must still meet the specific guidelines and criteria set by Texas Medicaid for coverage.
The form must be faxed to Caremark at the specified number. Email submissions are not accepted due to security regulations.
Patients may not receive immediate confirmation. The approval process can take some time, and it’s best to follow up directly with Caremark for updates.
This form is specifically tailored for Texas Medicaid, so it’s designed for residents covered under that program. Other states have different procedures.
Submitting false or inaccurate information can have serious consequences, including denial of the authorization request and potential legal implications.
Clarifying these misconceptions reduces anxiety surrounding the process and encourages informed participation in obtaining necessary medical care. Always ensure that you or your healthcare provider take the time to complete the Texas Pre Authorization Request form accurately and comprehensively.
Key takeaways
Filling out and using the Texas Pre Authorization Request form is an important step in ensuring coverage for Global Prescription Exceptions. Below are key takeaways to help navigate this process effectively.
- Accurate Information: Ensure all fields are filled out accurately, including patient and prescribing physician details.
- Sign and Date: Don’t forget to sign and date the form. An unsigned form may lead to delays.
- Intent of Administration: Clearly indicate if the drug will be administered in-office or through a pharmacy.
- FDA Approval: Confirm if the drug is being used for an FDA-approved indication. If yes, you can skip to Question 4.
- Healthcare Guidelines: Be prepared to justify the requested drug with appropriate clinical guidelines or compendia references.
- Failure of Alternatives: Document any previous failures or intolerances to preferred formulary alternatives. This is critical for approval.
- Dosing Guidelines: Ensure that the prescription adheres to the manufacturer's dosing guidelines or recognized literature.
- Benefit Coverage: Verify that the prescribed drug aligns with medically accepted indications recognized as a benefit by your health plan.
- Contact Information: Keep Caremark's contact information handy for any questions during the process. Reach them at 1-877-440-3621.
By following these takeaways, you can streamline the prior authorization process and enhance the likelihood of receiving the needed coverage in a timely manner.
Browse Other Templates
N1 Form Ontario Pdf - The effective date on this form indicates when the approved supplement will take effect.
Wells Fargo Letterhead - Employees can learn about the expectations regarding appearance and demeanor.
Work Order Completion Form - Ensure no liens are placed against the property after repairs.