Fill Out Your Tufts Prior Authorization Form
The Tufts Prior Authorization form is an essential tool for healthcare providers looking to obtain approval for specific pharmacy requests that necessitate prior review by Tufts Health Plan. This form plays a vital role in ensuring that patients receive the medications they need while adhering to the health plan's policies and guidelines. The form is particularly relevant for those enrolled in various Tufts Medicare plans, including the Medicare Preferred HMO and the Medicare Preferred PDP. One of its key features is the requirement for detailed patient and prescriber information, along with specific drug details like its name, strength, dosage form, and the requested duration of treatment. Additionally, there is a dedicated section for clinical justification, allowing prescribers to explain the rationale behind the medication request. This could entail detailing prior medications, any adverse reactions, and the necessary background to support the need for the requested drug. In cases where expedited review is necessary—such as when the patient's health may be at risk—the form provides an option to indicate this urgency. By facilitating the exchange of critical information between healthcare providers and Tufts Health Plan, the Prior Authorization form ultimately aims to enhance patient care while managing costs and ensuring appropriate medication use.
Tufts Prior Authorization Example
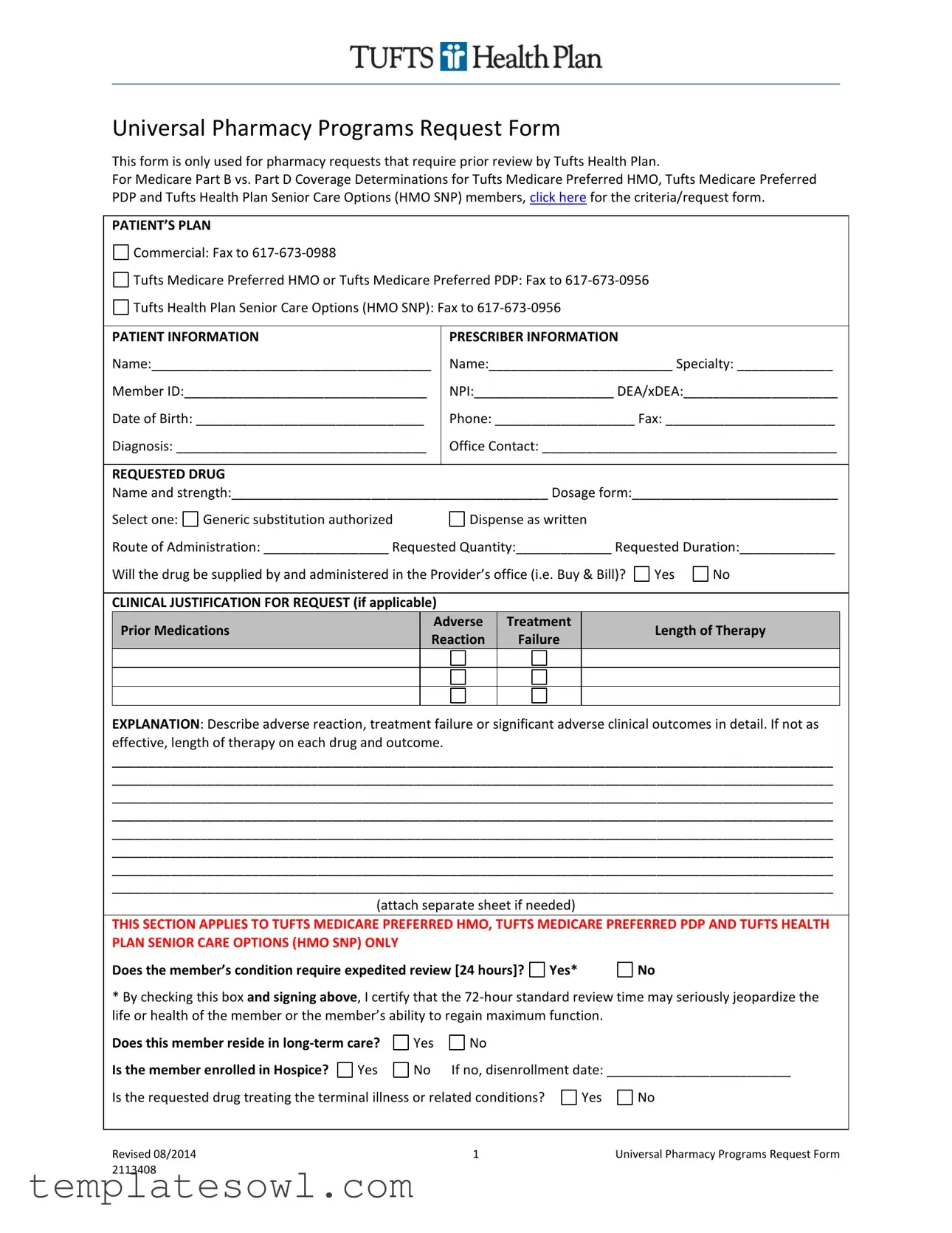
Universal Pharmacy Programs Request Form
This form is only used for pharmacy requests that require prior review by Tufts Health Plan.
For Medicare Part B vs. Part D Coverage Determinations for Tufts Medicare Preferred HMO, Tufts Medicare Preferred PDP and Tufts Health Plan Senior Care Options (HMO SNP) members, click here for the criteria/request form.
PATIENT’S PLAN
Commercial: Fax to
Tufts Medicare Preferred HMO or Tufts Medicare Preferred PDP: Fax to
Tufts Health Plan Senior Care Options (HMO SNP): Fax to
PATIENT INFORMATION
Name:______________________________________
Member ID:_________________________________
Date of Birth: _______________________________
Diagnosis: __________________________________
PRESCRIBER INFORMATION
Name:_________________________ Specialty: _____________
NPI:___________________ DEA/xDEA:_____________________
Phone: ___________________ Fax: _______________________
Office Contact: ________________________________________
REQUESTED DRUG
Name and strength:___________________________________________ Dosage form:____________________________
Select one:
Generic substitution authorized
Dispense as written
Route of Administration: _________________ Requested Quantity:_____________ Requested Duration:_____________
Will the drug be supplied by and administered in the Provider’s office (i.e. Buy & Bill)?
Yes
No
CLINICAL JUSTIFICATION FOR REQUEST (if applicable)
|
Prior Medications |
|
|
Adverse |
|
|
Treatment |
|
|
Length of Therapy |
|
|
|
|
Reaction |
|
|
Failure |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EXPLANATION: Describe adverse reaction, treatment failure or significant adverse clinical outcomes in detail. If not as effective, length of therapy on each drug and outcome.
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
(attach separate sheet if needed)
THIS SECTION APPLIES TO TUFTS MEDICARE PREFERRED HMO, TUFTS MEDICARE PREFERRED PDP AND TUFTS HEALTH PLAN SENIOR CARE OPTIONS (HMO SNP) ONLY
Does the member’s condition require expedited review [24 hours]?
Yes*
No
*By checking this box and signing above, I certify that the
Does this member reside in
Is the member enrolled in Hospice? |
Yes |
Yes
No
No
If no, disenrollment date: _________________________
Is the requested drug treating the terminal illness or related conditions?
Yes
No
Revised 08/2014 |
1 |
Universal Pharmacy Programs Request Form |
2113408 |
|
|
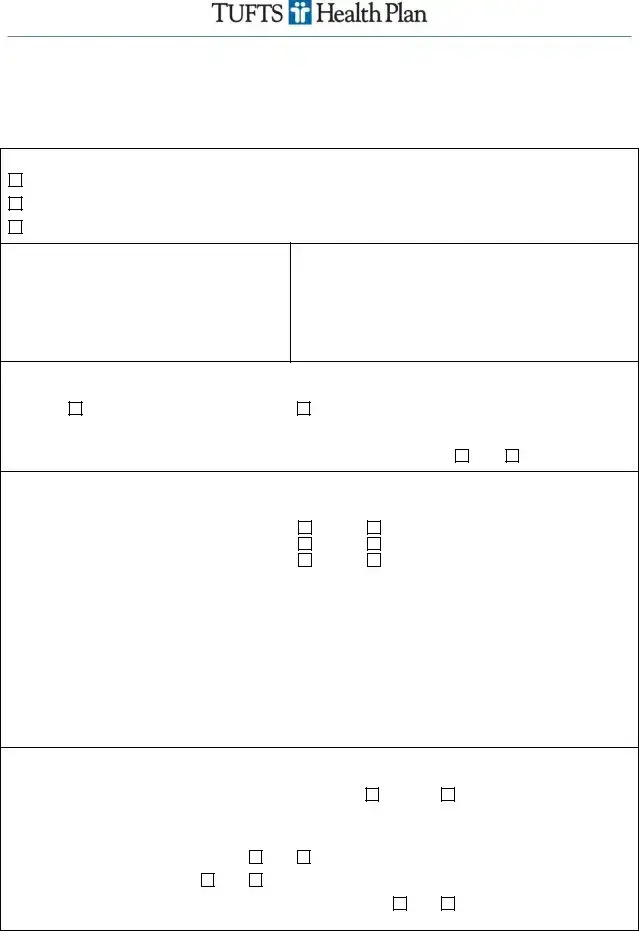
Provide an explanation of why the drug is being prescribed if not to treat the terminal illness/related conditions:
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
Rationale for prior authorization or exception request. Check statement(s) that apply, and include supporting documentation under the Clinical Justification and Explanation sections above:
Alternate formulary drug(s) contraindicated or previously tried, but with adverse outcome.
Document drug name, adverse outcome and, if therapeutic failure, length of therapy on drug.

 Complex patient with one or more chronic conditions is stable on current drug(s); high risk of significant adverse clinical outcome with medication change. Document anticipated significant adverse clinical outcome.
Complex patient with one or more chronic conditions is stable on current drug(s); high risk of significant adverse clinical outcome with medication change. Document anticipated significant adverse clinical outcome.

 Medical need for different dosage form and/or higher dosage. Document dosage form(s) and/or dosage(s) tried and explain medical reason.
Medical need for different dosage form and/or higher dosage. Document dosage form(s) and/or dosage(s) tried and explain medical reason.
Is this a request for a tier exception*?
Yes
No
*All formulary/preferred drug(s) on lower tier(s) contraindicated to the member’s condition or were tried and failed, or not as effective as requested drug. Specialty tier is excluded from tiering exception.
Indication: _________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
Prescriber Signature (required):______________________________________________ Date:_____________________
Provider Services
Provider Relations
Revised 08/2014 |
2 |
Universal Pharmacy Programs Request Form |
Form Characteristics
| Fact Name | Details |
|---|---|
| Purpose of the Form | This form is used for pharmacy requests that necessitate prior review by Tufts Health Plan, ensuring the requested medication is covered under the patient's specific plan. |
| Submitting Organizations | Commercial plans and Medicare plans, such as Tufts Medicare Preferred HMO and Tufts Health Plan Senior Care Options, require specific fax numbers for submission of the request form. |
| Information Required | Essential patient and prescriber information must be included, such as member ID, dates of birth, diagnosis, and details regarding the drug being requested for prior authorization. |
| Expedited Review | Requests for expedited review can be made if the member’s health condition warrants it. A checkmark in the specified box certifies that the standard review time may jeopardize the member’s health. |
| Documentation for Rationale | Detailed explanations and supporting documentation are necessary to justify the prior authorization request. This includes information on previous medications, adverse reactions, and specific medical needs. |
Guidelines on Utilizing Tufts Prior Authorization
Filling out the Tufts Prior Authorization form is straightforward. Ensure that all relevant information is accurate and complete, as this will facilitate a smoother approval process. Follow the steps outlined below to correctly fill out the form.
- Start by indicating the patient’s plan. Select the appropriate fax number based on the patient's plan type:
- Commercial: Fax to 617-673-0988
- Tufts Medicare Preferred HMO or PDP: Fax to 617-673-0956
- Tufts Health Plan Senior Care Options (HMO SNP): Fax to 617-673-0956
- Fill in the patient information section with:
- Patient Name
- Member ID
- Date of Birth
- Diagnosis
- Provide the prescriber information, including:
- Prescriber Name
- Specialty
- NPI
- DEA/xDEA
- Phone number
- Fax number
- Office contact name
- Enter details about the requested drug:
- Name and strength of the drug
- Dosage form
- Choose one: Generic substitution authorized or Dispense as written
- Route of administration
- Requested quantity
- Requested duration
- Indicate if the drug will be supplied and administered in the provider’s office (Buy & Bill).
- Detail any clinical justification for the request, including prior medications, adverse reactions, treatment lengths, and failures. Write a detailed description in the specified area.
- If applicable, answer the additional questions regarding the member’s condition and whether expedited review is needed:
- Check “Yes” or “No” for expedited review.
- Indicate if the member resides in long-term care or is enrolled in hospice.
- Provide a disenrollment date if applicable.
- Clarify if the requested drug is treating a terminal illness or related conditions.
- Follow up with the rationale for the prior authorization or exception request by checking the relevant statements and providing supporting documentation.
- Sign and date the form at the end to complete the submission.
Once you have completed the form with all necessary details, submit it to the appropriate fax number for the patient's plan. Keep a copy for your records. You can follow up with the provider or Tufts if you have questions about the submission or the status of the authorization.
What You Should Know About This Form
What is the Tufts Prior Authorization form used for?
The Tufts Prior Authorization form is specifically designed for pharmacy requests that need prior review by Tufts Health Plan. This includes medications that require approval before they can be dispensed to members. It is crucial for ensuring that the prescribed medication meets coverage criteria set by the health plan.
Who should use this form?
This form is intended for healthcare providers who are prescribing medications for patients enrolled in plans such as Tufts Medicare Preferred HMO, Tufts Medicare Preferred PDP, or Tufts Health Plan Senior Care Options (HMO SNP). If you are a prescriber managing a patient's medication, this form will aid in the request for prior authorization.
How can I submit the form?
Submission depends on the patient's specific plan. For Commercial patients, the completed form should be faxed to 617-673-0988. For Tufts Medicare Preferred HMO or PDP, the fax number is 617-673-0956. The same fax number applies for Tufts Health Plan Senior Care Options (HMO SNP).
What information is required to complete the form?
Key information includes the patient's name, Member ID, date of birth, diagnosis, and details about the prescriber. You will need to provide information about the requested drug such as its name, strength, dosage form, and route of administration. Clinical justification for the request—including details on prior medications and adverse reactions—is also required.
What should I include in the clinical justification section?
In this section, you'll need to detail any adverse reactions or treatment failures related to previous medications attempted by the patient. Be as specific as possible about the outcomes of those treatments and explain why the requested medication is necessary. If you run out of space, you can attach a separate sheet.
What if the patient needs expedited review?
If a member's condition requires an expedited review, clearly indicate this on the form. This option should be checked only if waiting for the standard review could jeopardize the patient's health or ability to regain maximum function. Include a brief explanation for the urgency in the appropriate section.
What happens after I submit the form?
Once submitted, the request will undergo review by Tufts Health Plan. Depending on the outcome, the prescriber will receive notification regarding approval or any additional information required. If approved, the medication can be dispensed according to the prescription. Be sure to maintain communication with both your patient and the health plan throughout this process.
Common mistakes
Filling out the Tufts Prior Authorization form can often be a daunting task. Many people make common mistakes that can delay the approval process. Addressing these issues promptly is essential to ensure timely access to necessary medications.
One frequent error is omitting critical patient information. This includes the patient's Member ID, date of birth, or even their diagnosis. Without this information, the processing of the request can be stalled, leading to unnecessary delays in treatment.
Additionally, incomplete prescriber information is a problem. It's vital to provide thorough details such as the prescriber’s NPI and DEA numbers. Missing this information can hinder the review process, as the healthcare provider cannot be easily identified.
Another common mistake is the failure to specify the requested drug accurately. Ambiguity regarding the drug name, strength, or dosage form can result in confusion and further delays. Always ensure that these details are correct and clearly stated to avoid potential issues.
Many requestors do not adequately explain clinical justification for the drug request. This section is crucial for demonstrating the medical necessity of the medication. Providing a detailed account of prior medications, adverse reactions, and treatment failures can significantly strengthen the request.
Some people overlook the expedited review option, which can lead to delays in urgent situations. If a member requires rapid access to medication, it's vital to check the expedited review box and provide a compelling reason for the urgency.
Furthermore, not addressing the special conditions for members in long-term care or hospice can lead to oversight. It is important to accurately answer whether the drug is treating a terminal illness or related conditions, as this can impact the authorization decision.
When it comes to tier exceptions, incomplete rationale is often submitted. Clearly identify why the requested drug is necessary despite the existence of lower-tier alternatives, and provide supporting documentation to make a strong case.
Lastly, ensure that the prescriber’s signature is provided and dated. This step is frequently missed. Without the signature, the request will be considered invalid, resulting in further delays. Each section of the form is designed to ensure clarity and expedite the approval process; overlooking these details can have serious consequences.
Documents used along the form
The Tufts Prior Authorization form is a crucial document that facilitates the review and approval process necessary for specific healthcare services and medications. In addition to this form, several other documents are commonly required to support the authorization request and ensure all necessary information is provided. Below is a list of forms and documents that are often used alongside the Tufts Prior Authorization form.
- Patient Consent Form: This document confirms that the patient has granted permission for their medical information to be shared with the health plan. It ensures compliance with privacy laws.
- Medical History Records: These records provide detailed information about the patient’s past medical treatments, conditions, and medications. They can be essential for justifying the necessity of the requested approval.
- Prescription Documentation: This includes a copy of the original prescription written by the healthcare provider. It is important for verifying that the requested medication is appropriate for the patient's condition.
- Clinical Notes from Healthcare Provider: Notes that document the healthcare provider's evaluation, treatment plan, and rationale for the medication request. These notes support the need for the prior authorization.
- Formulary Exception Request: If a non-formulary medication is requested, this document outlines the reasons why a formulary drug is not suitable for the patient. It provides an in-depth justification for the requested drug.
- Adverse Reaction History: A record that specifies any prior adverse reactions the patient has experienced with alternative medications. This document can help reinforce the need for the requested treatment.
- Specialist Referral Form: If the medication or treatment involves a specialist, this form is used to refer the patient to the appropriate provider. It often includes relevant details about the patient's condition.
Collectively, these documents help ensure that the prior authorization process is thorough, transparent, and considers the individual needs of each patient. Having all necessary documentation assists providers and health plans in making informed decisions regarding patient care.
Similar forms
- Medicaid Prior Authorization Request Form: This document functions in a similar manner by requiring a healthcare provider to justify a request for medication coverage. Like the Tufts form, it collects patient and prescriber information and outlines the clinical justification for the request.
- Healthcare Insurance Authorization Request: This form is used by various health insurance plans to determine whether certain services or medications are medically necessary. It includes sections for patient information, treatments requested, and rationales for the requested services, akin to the Tufts form.
- Medicare Part D Coverage Determination Request: Similar to the Tufts form, this document is specifically used to request prior authorization for drugs covered under Medicare Part D. It also requires justification and relevant patient details.
- Pharmacy Benefit Manager (PBM) Prior Authorization Form: This form is issued by pharmacy benefit managers to manage controlled medications. It includes similar sections for patient demographics, prescribing information, and the need for specific medications.
- Workers' Compensation Medication Authorization Request: Used in cases involving workplace injuries, this form verifies the need for medications related to treatment. It requires justification and details related to both the patient and the prescriber, much like the Tufts form.
- Medically Necessary Drug Exception Form: This is utilized when a patient needs a medication that is not typically covered. It involves providing details and reasons for the exception, resembling the justification requirements of the Tufts form.
- Pharmaceutical Company Prior Authorization Form: Pharmaceutical companies often have their own forms for requesting coverage. They ask for similar patient and prescriber information and require detailed explanations for the medical necessity of the drug.
- Specialty Drug Request Form: This type of document addresses requests for specialty medications that usually require additional scrutiny. It includes patient and clinical information, focusing on justifying the specialty drug's necessity.
- Outpatient Clinical Prior Authorization Workflow Document: While more of a process outline, this document supports the same objectives as the Tufts form. It helps healthcare providers understand what needs to be submitted for outpatient services and medications.
Dos and Don'ts
Filling out the Tufts Prior Authorization form can be a straightforward process if approached correctly. Here are six essential dos and don’ts to keep in mind to ensure your submission is as smooth as possible.
- DO provide complete patient information, including the member ID and date of birth. Accuracy is crucial.
- DO check the prescribing physician’s information. Ensure the NPI and DEA/xDEA numbers are accurate.
- DO explain the clinical justification in detail. Describe any adverse reactions or treatment failures clearly to support the request.
- DO utilize the correct fax number based on the patient's plan to avoid delays.
- DON'T leave any sections blank. Every part of the form is important and missing information can lead to complications.
- DON'T forget to sign the form. An unsigned form cannot be processed and will create unnecessary delays.
By following these guidelines, you can help facilitate a quicker review process for prior authorizations and improve the chances of approval for your patient’s medication needs.
Misconceptions
Misconceptions about the Tufts Prior Authorization form can lead to confusion for both patients and healthcare providers. Here are six common misconceptions clarified:
- Prior Authorization is Only Necessary for Expensive Medications: Many believe that only high-cost drugs require prior authorization. In reality, any medication that falls under specific criteria outlined by Tufts Health Plan may require this process.
- Only New Prescriptions Require Prior Authorization: Another misconception is that prior authorization is only needed for brand new prescriptions. This is not accurate; changes in dosage, formulation, or a patient's condition may also necessitate a prior authorization.
- Submitting the Form Guarantees Approval: There is a belief that filling out the Tufts Prior Authorization form guarantees that the medication will be approved. However, approval depends on the clinical justification provided and compliance with Tufts' policies.
- The Process is the Same for All Plans: Some assume that prior authorization procedures are identical across different plans. In fact, requirements can vary significantly between commercial, Medicare, and other healthcare plans.
- Expedited Reviews are Rarely Granted: A common myth is that expedited reviews are seldom approved. In situations where a member’s health is at serious risk, expedited requests can and do get approved with proper justification.
- Once Approved, Prior Authorization is Permanent: Many think that once a medication is authorized, it remains authorized indefinitely. In truth, approvals often have time limits and may need to be renewed based on ongoing medical evaluations.
Understanding these misconceptions is crucial for ensuring that patients receive timely access to necessary medications.
Key takeaways
The Tufts Prior Authorization form is essential for obtaining approval for certain pharmacy requests that require prior review by Tufts Health Plan.
This form is specifically designed for requests related to members of Tufts Medicare Preferred HMO, Tufts Medicare Preferred PDP, and Tufts Health Plan Senior Care Options.
Ensure you correctly identify the patient’s plan and fax the request to the appropriate number based on their membership.
All required patient information must be filled out accurately, including name, member ID, date of birth, and diagnosis.
Prescriber information is crucial. Include details such as name, specialty, NPI, DEA/xDEA, phone number, and fax.
Detail the requested drug, including its name, strength, dosage form, route of administration, quantity, and duration.
The clinical justification section requires an explanation of the patient’s treatment history, including prior medications and any adverse reactions.
When applicable, check the expedited review box if the patient's condition requires a response in 24 hours, and provide relevant details.
Document any reasons for prescribing a medication outside of standard treatment, especially when treating terminal illnesses or chronic conditions.
Finally, ensure that the prescriber’s signature and date are included, as these are mandatory for processing the request.
Browse Other Templates
Single Party Listing - The form illustrates the adaptability of listing contracts in Wisconsin real estate.
Optum Rx Fax Form - Every fax submission should include the date to verify timeliness.
Rebounderz - Minor participants must also have their birthdays and names listed for clarity.