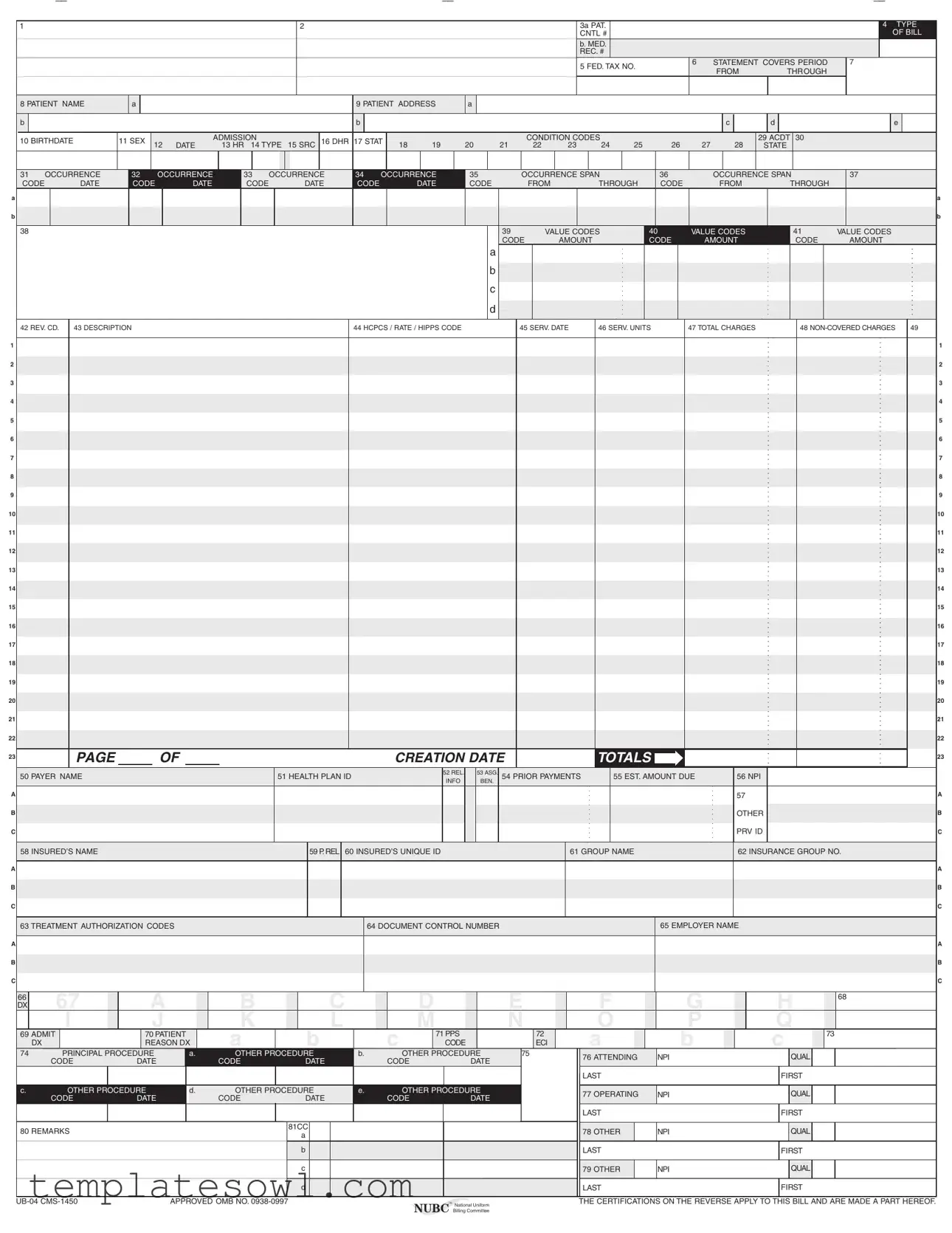
Fill Out Your Ub04 Form
The UB-04 form, also known as the CMS-1450, serves as a crucial component in the healthcare billing landscape. Used primarily by facilities such as hospitals, nursing homes, and rehabilitation centers, this standardized claim form assists with the submission of services rendered to patients for payment from Medicare, Medicaid, and private insurers. Within its structured layout, the UB-04 captures essential patient and provider information, including details such as patient name, identification numbers, and the specific services billed, along with designated codes that categorize diagnoses and procedures. It provides separate sections to itemize charges, outline payment responsibilities, and ensure that all necessary authorizations and certifications are duly noted. Additionally, compliance with federal and state regulations is highlighted through various certifications included in the form. This form not only acts as a means of financial transaction between healthcare providers and payers, but it also plays a significant role in maintaining the integrity of healthcare reimbursement practices.
Ub04 Example
A
B
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
A
B
C
A
B
C
A
B
C
1 |
2 |
3a PAT. |
|
|
|
|
|
4 TYPE |
|
|
CNTL # |
|
|
|
|
|
OF BILL |
|
|
b. MED. |
|
|
|
|
|
|
|
|
REC. # |
|
|
|
|
|
|
|
|
5 FED. TAX NO. |
6 |
STATEMENT COVERS PERIOD |
7 |
|
||
|
|
|
FROM |
THROUGH |
|
|
||
|
|
|
|
|
|
|
||
8 PATIENT NAME |
a |
|
|
|
|
9 PATIENT ADDRESS |
a |
|
|
|
|
|
|
|
|
|
|
||
b |
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
c |
d |
e |
10 BIRTHDATE |
11 SEX |
|
|
ADMISSION |
|
16 DHR 17 STAT |
|
|
|
|
CONDITION CODES |
|
|
|
|
|
29 ACDT 30 |
|
|
12 |
DATE |
13 HR 14 TYPE |
15 SRC |
18 |
19 |
20 |
21 |
22 |
23 |
24 |
25 |
26 |
27 |
28 |
STATE |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
31 OCCURRENCE |
32 |
|
OCCURRENCE |
33 |
OCCURRENCE |
34 |
OCCURRENCE |
35 |
|
|
|
OCCURRENCE SPAN |
|
36 |
|
|
|
OCCURRENCE SPAN |
|
37 |
|
|
|
||||||||||||||||||||||||||||||
CODE |
DATE |
CODE |
|
DATE |
CODE |
|
|
|
DATE |
CODE |
|
DATE |
CODE |
|
|
|
FROM |
THROUGH |
|
CODE |
|
|
FROM |
|
THROUGH |
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
38 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
39 |
|
|
VALUE CODES |
40 |
|
|
VALUE CODES |
|
41 |
|
VALUE CODES |
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CODE |
|
AMOUNT |
|
|
|
CODE |
|
|
AMOUNT |
|
CODE |
|
AMOUNT |
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
a |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
d |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
42 REV. CD. |
43 DESCRIPTION |
|
|
|
|
|
|
|
|
|
|
|
|
|
44 HCPCS / RATE / HIPPS CODE |
|
|
|
|
45 SERV. DATE |
46 SERV. UNITS |
47 TOTAL CHARGES |
|
|
48 |
49 |
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
7 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
8 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
9 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
11 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
12 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
13 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
15 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
17 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
18 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
19 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
20 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
21 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
22 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PAGE |
|
|
OF |
|
|
|
|
|
|
|
|
|
|
CREATION DATE |
|
|
|
|
|
|
|
TOTALS |
|
|
|
|
|
|
|
|
|
|
|
|
|
23 |
|||||||||||||||
50 PAYER NAME |
|
|
|
|
|
|
|
|
51 HEALTH PLAN ID |
|
|
|
|
52 REL. |
|
53 ASG. |
54 PRIOR PAYMENTS |
|
55 EST. AMOUNT DUE |
|
|
56 NPI |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
INFO |
|
BEN. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
57 |
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
OTHER |
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PRV ID |
|
|
|
|
|
|
|
|
C |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
58 INSURED’S NAME |
|
|
|
|
|
|
|
|
|
|
|
59 P. REL |
60 INSURED’S UNIQUE ID |
|
|
|
|
|
|
|
|
61 GROUP NAME |
|
|
|
|
|
|
|
62 INSURANCE GROUP NO. |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
63 TREATMENT AUTHORIZATION CODES |
|
|
|
|
|
|
|
|
64 DOCUMENT CONTROL NUMBER |
|
|
|
|
|
|
|
|
|
|
|
|
65 EMPLOYER NAME |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C
66 |
67 |
A |
|
B |
|
C |
|
D |
|
E |
F |
G |
H |
68 |
DX |
|
|
|
|
|
|||||||||
|
I |
J |
|
K |
|
L |
|
M |
|
N |
O |
P |
Q |
|
69 ADMIT |
70 PATIENT |
|
A |
B |
|
C |
71 PPS |
|
72 |
A |
B |
C |
73 |
|
|
DX |
REASON DX |
|
CODE |
|
ECI |
|
|||||||
74 |
PRINCIPAL PROCEDURE |
a. |
OTHER PROCEDURE |
b. |
|
OTHER PROCEDURE |
75 |
76 ATTENDING |
NPI |
QUAL |
|
|||
|
CODE |
DATE |
|
CODE |
DATE |
|
CODE |
DATE |
|
|
||||
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
LAST |
|
FIRST |
|
c. |
OTHER PROCEDURE |
d. |
OTHER PROCEDURE |
e. |
|
OTHER PROCEDURE |
|
77 OPERATING |
NPI |
QUAL |
|
|||
|
CODE |
DATE |
|
CODE |
DATE |
|
CODE |
DATE |
|
|
||||
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
LAST |
|
FIRST |
|
80 REMARKS |
|
|
|
81CC |
|
|
|
|
|
78 OTHER |
NPI |
QUAL |
|
|
|
|
|
a |
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
b |
|
|
|
|
|
LAST |
|
FIRST |
|
|
|
|
|
|
c |
|
|
|
|
|
79 OTHER |
NPI |
QUAL |
|
|
|
|
|
|
d |
|
|
|
|
|
LAST |
|
FIRST |
|
APPROVED OMB NO. |
™ National Uniform |
THE CERTIFICATIONS ON THE REVERSE APPLY TO THIS BILL AND ARE MADE A PART HEREOF. |
|
|
|
NUBC Billing Committee |
|

Submission of this claim constitutes certification that the billing information as shown on the face hereof is true, accurate and complete. That the submitter did not knowingly or recklessly disregard or misrepresent or conceal material facts. The following certifications or verifications apply where pertinent to this Bill:
1.If third party benefits are indicated, the appropriate assignments by the insured /beneficiary and signature of the patient or parent or a legal guardian covering authorization to release information are on file. Determinations as to the release of medical and financial information should be guided by the patient or the patient’s legal representative.
2.If patient occupied a private room or required private nursing for medical necessity, any required certifications are on file.
3.Physician’s certifications and
4.For Religious
5.Signature of patient or his representative on certifications, authorization to release information, and payment request, as required by Federal Law and Regulations (42 USC 1935f, 42 CFR 424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other applicable contract regulations, is on file.
6.The provider of care submitter acknowledges that the bill is in conformance with the Civil Rights Act of 1964 as amended. Records adequately describing services will be maintained and necessary information will be furnished to such governmental agencies as required by applicable law.
7.For Medicare Purposes: If the patient has indicated that other health insurance or a state medical assistance agency will pay part of his/her medical expenses and he/she wants information about his/her claim released to them upon request, necessary authorization is on file. The patient’s signature on the provider’s request to bill Medicare medical and
8.For Medicaid purposes: The submitter understands that because payment and satisfaction of this claim will be from Federal and State funds, any false statements, documents, or concealment of a material fact are subject to prosecution under applicable Federal or State Laws.
9.For TRICARE Purposes:
(a)The information on the face of this claim is true, accurate and complete to the best of the submitter’s knowledge and belief, and services were medically necessary and appropriate for the health of the patient;
(b)The patient has represented that by a reported residential address outside a military medical treatment facility catchment area he or she does not live within the catchment area of a U.S. military medical treatment facility, or if the patient resides within a catchment area of such a facility, a copy of
(c)The patient or the patient’s parent or guardian has responded directly to the provider’s request to identify all health insurance coverage, and that all such coverage is identified on the face of the claim except that coverage which is exclusively supplemental payments to
(d)The amount billed to TRICARE has been billed after all such coverage have been billed and paid excluding Medicaid, and the amount billed to TRICARE is that remaining claimed against TRICARE benefits;
(e)The beneficiary’s cost share has not been waived by consent or failure to exercise generally accepted billing and collection efforts; and,
(f)Any
(g)Based on 42 United States Code 1395cc(a)(1)(j) all providers participating in Medicare must also participate in TRICARE for inpatient hospital services provided pursuant to admissions to hospitals occurring on or after January 1, 1987; and
(h)If TRICARE benefits are to be paid in a participating status, the submitter of this claim agrees to submit this claim to the appropriate TRICARE claims processor. The provider of care submitter also agrees to accept the TRICARE determined reasonable charge as the total charge for the medical services or supplies listed on the claim form. The provider of care will accept the
SEE http://www. nubc . org/ FOR MORE INFORMATION ON
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Name | The UB-04 form, also known as the CMS-1450, is used for billing institutional services. |
| Purpose | This form serves as a request for payment from Medicare and other insurance payers for hospital and other medical facility services. |
| Standardization | The UB-04 is a standardized billing form adopted by the National Uniform Billing Committee (NUBC) to streamline the billing process. |
| Field Count | The form consists of 81 fields, each serving a specific purpose in detailing the billing information. |
| Submission | Healthcare providers must submit the UB-04 form electronically to comply with payer requirements for better processing. |
| State-Specific Forms | Certain states may require specific variations of the UB-04 form to comply with local laws. For instance, California has specific regulations under the California Code of Regulations. |
| Governing Laws | The use and submission of the UB-04 form are governed by various federal laws, including Medicare regulations and the Affordable Care Act. |
| Common Errors | Common errors include incorrect patient identifiers, missing information in required fields, and erroneous coding, which can cause delays in payment processing. |
| Patient Information | Essential patient information, such as name, date of birth, and medical record number, must be accurately reported on the form. |
| Submission Certification | Submitting the UB-04 certifies that the provided information is accurate and complete, ensuring legal accountability for any potential misrepresentation. |
Guidelines on Utilizing Ub04
Completing the UB-04 form accurately is crucial for proper billing and insurance reimbursement. Many healthcare providers use this form to submit claims for services provided to patients. Follow the steps outlined below to ensure all necessary information is correctly filled out.
- Begin with Patient Information: Enter the patient’s identification details such as the name, address, birthdate, and sex in the designated fields.
- Billing Information: Record the control number, medical record number, federal tax number, and the statement coverage period (from and through dates).
- Admission Details: Fill in the admission date, hour, type of service, and the source of admission.
- Condition and Diagnosis Codes: Indicate the condition codes in section 17 and fill in the diagnosis codes in sections I through K.
- Procedure Codes: In section 74, provide the principal and other procedure codes along with their corresponding dates if applicable.
- Charges: Enter total charges, non-covered charges, and revenue codes in sections 47 through 49.
- Payer Information: Complete the payer and health plan ID, including prior payments and the estimated amount due in sections 50 through 55.
- Insured’s Information: Fill out details about the insured party, including their name and relationship to the patient.
- Employer and Authorization Codes: If applicable, include the employer name and any treatment authorization codes in sections 65 and 63.
- Provider's NPI Numbers: Document the attending and operating provider’s National Provider Identifier (NPI) along with their qualifications.
- Review and Certify: After filling out all sections, review the form for accuracy and sign where required to certify the information is true.
Once the form is completed, provide the necessary supporting documentation required by payers. Submitting the UB-04 form promptly to the correct payer will aid in faster processing of claims. Ensure all details are accurate to minimize delays and potential rejections.
What You Should Know About This Form
What is a UB-04 form?
The UB-04 form, also known as the CMS-1450, is a standardized claim form used by healthcare providers to bill Medicare, Medicaid, and private health insurers for institutional services. It captures a wide range of information related to patient admissions, treatment, and charges, allowing providers to receive reimbursement for their services. The form includes details like patient information, billing codes, service dates, and total charges, facilitating an efficient claim submission process across multiple entities. Understanding this form is essential for both healthcare providers and patients alike.
Who uses the UB-04 form?
The UB-04 form is primarily utilized by hospitals, skilled nursing facilities, and other institutional healthcare providers. These entities use it to bill for services rendered to patients, including inpatient and outpatient care. Insurance companies, including Medicare and Medicaid, rely on this form to process claims and reimburse providers. Therefore, it acts as a vital communication tool that connects healthcare services with financial reimbursement.
What information is required on a UB-04 form?
Filling out a UB-04 form requires a range of information to ensure accurate billing. Essential details include the patient's name, address, and birthdate, as well as information about the healthcare provider, including identification numbers. The form also requires details related to the patient's treatment, such as admission and service dates, diagnosis and procedure codes, and total charges. Lastly, data about insurance coverage, including payer name and group number, is crucial for proper claim processing.
How is the UB-04 form different from the HCFA 1500 form?
The UB-04 and HCFA 1500 forms serve different purposes and are used by different types of healthcare providers. The UB-04 is designed for institutional providers, such as hospitals and skilled nursing facilities, focusing on billing for services provided during patient admissions. In contrast, the HCFA 1500 form is utilized by individual healthcare providers, such as physicians and outpatient clinics, to bill for services offered on an outpatient basis. This distinction is important for ensuring that claims are submitted correctly to the appropriate payers.
What are the consequences of incorrectly filling out a UB-04 form?
Filling out the UB-04 form incorrectly can lead to several issues, including delayed payments or denials from insurance companies. If inaccuracies occur, providers may face additional administrative burdens to correct and resubmit claims. Incorrect information may also trigger audits or investigations, potentially resulting in fines or penalties for fraud if misrepresentation is suspected. Therefore, accuracy and attention to detail while completing the form are essential for prompt reimbursement.
Where can I find more information about the UB-04 form?
For those seeking more information about the UB-04 form, various resources are available. The National Uniform Billing Committee (NUBC) offers comprehensive information regarding the data elements and printing specifications of the form on their website. Additionally, healthcare providers often have internal resources, such as billing departments or compliance officers, who can offer guidance on properly completing and submitting the UB-04 form. Keeping informed and up-to-date on any changes in regulations or billing practices is crucial for providers.
Common mistakes
When filling out the UB-04 form, accuracy is paramount. One common mistake is failing to complete all necessary fields. Every applicable section, including patient information and procedural codes, must be filled out. Omitting vital details can lead to claim denials or delays in processing.
Another frequent error occurs when providers enter incorrect patient identifiers. Inaccurate identification, such as misspelled names or incorrect medical record numbers, can cause significant issues in claim processing. A mismatch may result in rejections from insurance companies, prolonging the billing process.
Many individuals mistakenly omit the federal tax identification number. This number is crucial for identifying the billing entity and must be accurately included. Failure to provide this information might complicate the tax reporting process and could lead to compliance issues.
Additionally, not properly completing the sections related to the services provided is a significant oversight. This includes the service dates and units. When providers fail to detail the dates when services were rendered or the quantity of services provided, it may confuse insurance companies. Such confusion often results in lower reimbursement or denial of claims.
Moreover, many users neglect to confirm that all codes used—ICD, CPT, and HCPCS—are correct. These codes must accurately reflect the diagnosis and treatment. Using outdated or incorrect codes can lead to further complications, including audits and increased scrutiny from payers.
It is also common to see inaccuracies in the occurrence codes. These codes are essential for supporting the medical necessity of treatments rendered. Misrepresenting these can lead to potential allegations of fraudulent billing practices.
Neglecting to obtain the necessary signatures can also create a significant error. The UB-04 form requires verification from patients or guardians when applicable. Without these signatures, claims may be deemed invalid or improperly authorized, resulting in increased administrative work.
Another mistake involves failing to review the claim before submission. A lack of thoroughness can result in missing errors that could have easily been corrected prior to sending the claim. This oversight can complicate the reimbursement process and create unnecessary delays.
Lastly, many people mistakenly assume that once the form is submitted, their job is done. Continuous tracking of claims is essential. Providers should ensure that they follow up on submitted claims to confirm they have been processed correctly and any issues are promptly resolved.
Documents used along the form
The UB-04 form, also known as the CMS-1450, is a critical document in the healthcare billing process, specifically for institutional providers such as hospitals and nursing facilities. However, it often is accompanied by other forms and documents that streamline claims processing and communication with payers. Below is a list of commonly used forms that often complement the UB-04 in healthcare billing procedures.
- CMS 1500 Form: This form is primarily used by individual healthcare providers for outpatient services. It includes details about the patient, the provider, and the procedures performed, serving as a counterpart to the UB-04 for non-institutional claims.
- Advance Beneficiary Notice of Noncoverage (ABN): This document is used to inform Medicare beneficiaries that Medicare is unlikely to pay for a particular service or item. It serves as a safeguard for providers to ensure that patients understand their financial responsibility in case services are deemed non-covered by Medicare.
- Hospital Outpatient Prospective Payment System (OPPS) Notice: This notice is required for outpatient hospital services. It informs patients about their rights concerning billing and cost estimates for the services provided, giving them transparency before treatment begins.
- Patient Authorization Form: A vital document that grants healthcare providers permission to share a patient’s medical information with insurers or other third parties. This form ensures compliance with privacy regulations and facilitates claims processes that require sharing of sensitive information.
- Medicare Credit Balance Report: This report details any overpayments or credit balances owed back to Medicare. Monitoring and reporting these balances are crucial for compliance purposes and to avoid future billing errors that could attract penalties.
- Claim Adjustment Request (CAR): Also known as a claim reconsideration request, this document allows providers to formally contest claims that were denied or underpaid. By submitting a CAR, the provider seeks a review and adjustment of the original claim payment based on new information or corrections.
Alongside the UB-04 form, these documents facilitate accurate claims submission, ensure compliance with federal regulations, and enhance communication between healthcare providers and payers. Collectively, they foster a more streamlined and transparent billing process, which benefits all parties involved.
Similar forms
The UB-04 form, also known as CMS-1450, is a key document used in the healthcare billing process, specifically for institutional providers. Several other documents share similarities with the UB-04, functioning in a similar way by providing essential information for billing and claims purposes. Here are seven other documents that are similar to the UB-04 form:
- CMS-1500: Like the UB-04, the CMS-1500 is a billing form used to submit claims for medical services. However, while the UB-04 is primarily for institutional providers, the CMS-1500 is typically used by individual healthcare professionals and outpatient services.
- HCFA 1450: This document is another name for the UB-04 form, emphasizing its relevance to the Healthcare Financing Administration. It contains similar data elements and serves the same purpose in billing for healthcare services.
- Dental Claim Form: Dental providers use this form to detail various dental services provided. It collects patient information, treatment details, and billing amounts, similar to how the UB-04 captures information related to hospital stays and services.
- Electronic Claims Submission: Many providers submit claims electronically using standardized formats that replicate the information found on the UB-04. This practice streamlines the claims process, ensuring consistency and accuracy in patient data and billing details.
- Institutional Claims Attachment: This document complements the UB-04 by providing additional information that may not fit on the standard form. It supports detailed descriptions of services rendered, similar to the comprehensive data captured on the UB-04.
- Medicare Claims Form: Specifically for Medicare, this form contains data akin to the UB-04. It requires providers to submit patient and service information to receive reimbursement from Medicare, paralleling the UB-04's role in institutional billing.
- Disability Claim Form: When patients file for disability benefits, they often must complete a specific claim form that includes details about medical treatment and costs. This form functions similarly to the UB-04 by outlining necessary information for reimbursement purposes.
Understanding these various documents can aid healthcare providers and patients in navigating the complex landscape of medical billing, ensuring a smoother claims process.
Dos and Don'ts
When filling out the UB-04 form, attention to detail is essential for a smooth billing process. Here are key points to consider:
- Do: Ensure all patient information is accurate, including their name, address, and insurance details.
- Do: Use the correct codes for diagnoses and procedures as required by federal regulations.
- Do: Verify that all required signatures are present before submission.
- Do: Maintain copies of the submitted form for your records.
- Do: Check that the dates on the form align with the services provided.
- Don’t: Omit any information that the form specifically requests.
- Don’t: Forget to review the entire form for accuracy before sending it to the payer.
Following these guidelines can help ensure the UB-04 form is completed correctly. Accuracy helps to prevent delays in payment and protects against potential penalties for incorrect submissions.
Misconceptions
Many people misunderstand the purpose and use of the UB-04 form. This can lead to confusion and errors in billing. Here are some common misconceptions:
- The UB-04 is only for hospitals. Many believe the UB-04 form is exclusively used by hospitals. While it is primarily for institutional providers, other entities like skilled nursing facilities and home health agencies also use it to bill services.
- Filling out the UB-04 is straightforward and requires no training. Some think that since the form is a standard template, it can be completed easily by anyone. In reality, accurate completion requires understanding various codes and regulations. Improper completion can lead to claim denials.
- The UB-04 is the same as the CMS-1500 form. Many people incorrectly assume these are interchangeable. While both forms are used for billing healthcare services, they serve different providers and are designed for distinct purposes. The UB-04 is used for institutional claims, while the CMS-1500 is for professional claims.
- Once submitted, the UB-04 claim is final and cannot be changed. Some individuals believe that a submitted UB-04 cannot be amended. However, if mistakes are found after submission, facilities can often resubmit corrected claims, but know that this must be done promptly and according to specific procedures.
Key takeaways
The UB-04 form is essential for billing healthcare services. Here are several key takeaways for accurate completion and effective use of this form:
- Ensure Accuracy: Double-check all entries for completeness and correctness. Incorrect information can lead to claim denials.
- Understand Required Codes: Familiarize yourself with the codes needed on the form, such as diagnosis codes and revenue codes. Each code has a specific meaning that is crucial for processing.
- Use Appropriate Dates: Clearly indicate the dates of service and patient admission. This helps expedite the claims process.
- Include Patient Information: Ensure that patient details, such as name, birthdate, and address, are filled out accurately. Incomplete information may delay payment.
- Maintain Documentation: Keep all supporting documents related to billing and services provided. These can be referenced in case of audits or disputes.
Browse Other Templates
Codicil to Will in Florida - Specific phrasing is provided to ensure clarity in the changes being made.
High Yield Savings Account Navy Federal - Consider any potential impacts on your account services when updating personal information.