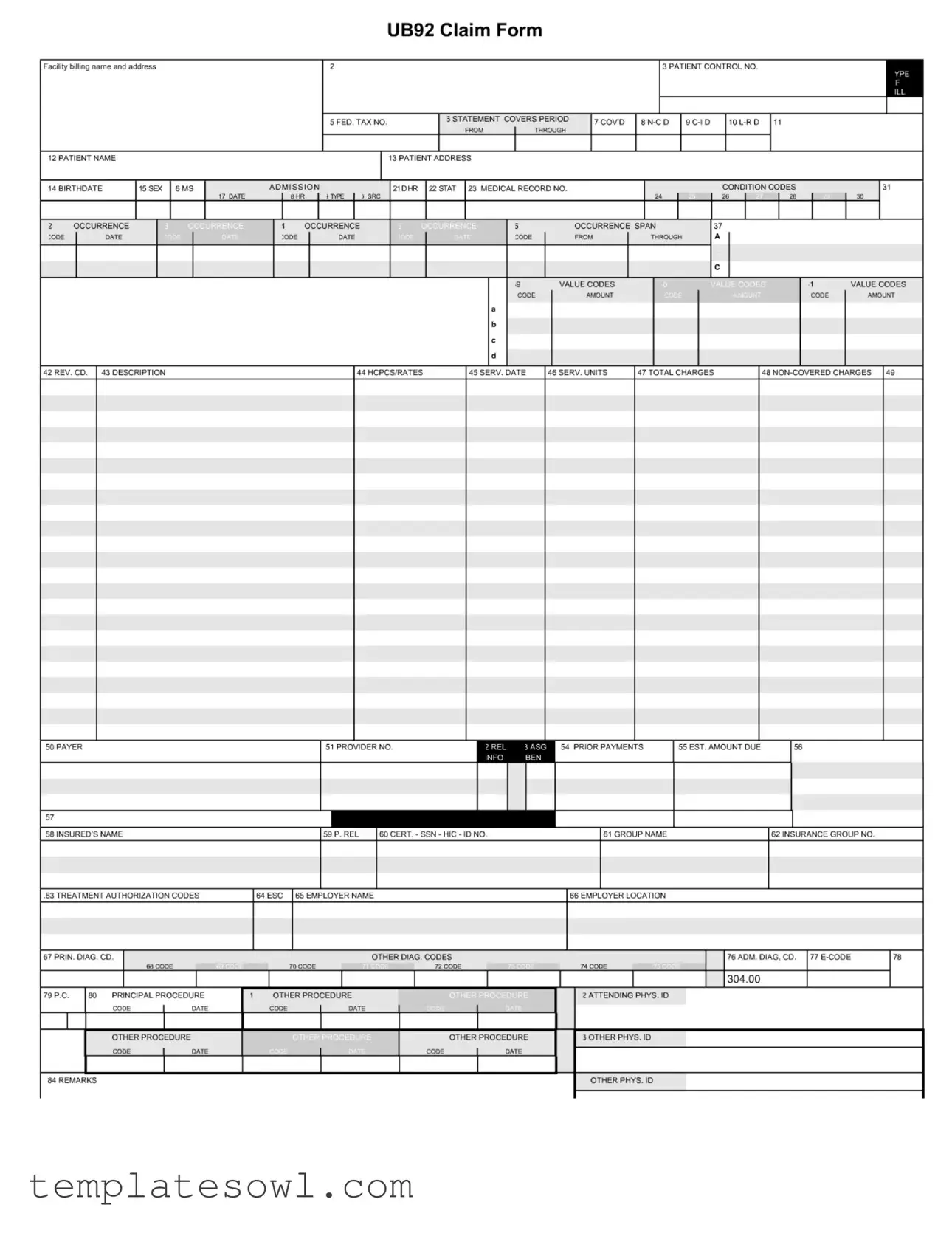
Fill Out Your Ub92 Claim Form
Navigating the complexities of healthcare billing requires understanding several key documents, with the UB92 Claim Form standing out as a critical component in the process. This form facilitates the billing of institutional healthcare services and collects essential data points relevant to patient care and insurance coverage. Among its various fields, you will find the Facility billing name and address, the Patient Control Number, and vital details like the patient's name, birthdate, and address. Notably, it also requires the Medical Record Number and indicators of the admissions condition. In addition, the form captures procedural data through diagnosis and procedure codes, detailing the services rendered during a specific treatment period. This includes codes for principal and additional diagnoses, along with codes that specify the type and source of care provided. Financial aspects such as total charges and prior payments are equally important, ensuring clarity in billing and reimbursement processes. Finally, the UB92 accommodates various insurance details, including the payer's information and authorization codes, making it an indispensable tool for healthcare providers and insurers alike.
Ub92 Claim Example
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The UB92 Claim Form is used for billing institutional healthcare services provided to patients. |
| Structure | This form includes numerous fields for patient and provider information, services rendered, and billing details. |
| Patient Information | Key patient details such as name, birthdate, and address must be clearly displayed on the form. |
| Facility Details | Providers must include the facility’s billing name and address at the top of the form. |
| Claims Processing | The form is processed by insurance companies to determine payment and coverage for services rendered. |
| Governing Law | The UB92 format is governed by federal laws such as the Health Insurance Portability and Accountability Act (HIPAA). |
| Submission Method | Claim submissions can be made electronically or by mailing a physical copy, depending on the payer's requirements. |
| Common Fields | Important fields include patient control number, service dates, procedure codes, and total charges. |
| Additional Codes | The form allows for various codes, including diagnosis codes and procedure codes, to specify services provided. |
| Updates and Revisions | Always check for the latest version of the form as updates may come out to reflect changes in billing practices. |
Guidelines on Utilizing Ub92 Claim
Filling out the UB92 Claim Form requires attention to detail and accurate information about the patient and services rendered. Ensure you have all necessary documents and information on hand before starting. Below are the steps to complete the form correctly:
- Facility Billing Information: Enter the facility’s billing name and address in the designated area.
- Patient Control Number: Fill in the unique control number assigned to the patient.
- Federal Tax Number: Input the facility's federal tax identification number.
- Statement Covers Period: Specify the period covered by the billing statement.
- Patient Information: Fill in the patient's name, birthdate, and address fields accurately.
- Sex: Mark the patient's sex on the form.
- Admission Condition Codes: Provide any relevant admission condition codes.
- Occurrence Codes: List any occurrence codes along with the dates they pertain to.
- Value Codes: Enter value codes and the corresponding amounts as necessary.
- Description and Service Details: State the description of services provided, the service date, service units, total charges, and any non-covered charges.
- Payer Information: Fill in payer details, including payer name, provider number, prior payments received, and insured name.
- Insurance Information: Enter group name, insurance group number, and treatment authorization codes.
- Employer Information: Include the employer's name and location if applicable.
- Diagnosis Codes: Enter the principal diagnosis code and any additional codes required.
- Principal and Other Procedures: Fill in the principal procedure code and any other procedure codes as needed.
- Attending Physicians: Include attending physician ID codes and dates.
- Remarks: Use the remarks section for any additional comments or information relevant to the claim.
Keep the completed form safe until submission. Double-check for accuracy to avoid delays in processing your claim.
What You Should Know About This Form
What is the UB92 Claim Form used for?
The UB92 Claim Form, also known as the UB-92 or CMS-1450, is used by healthcare facilities to bill for services provided to patients. It is primarily utilized for inpatient hospital services, outpatient services, and skilled nursing facilities. The form consolidates essential patient and service information, allowing for standardized billing across various healthcare providers and insurance companies.
What information is required on the UB92 Claim Form?
Several key pieces of information must be filled out on the UB92 Claim Form. This includes the facility's billing name and address, patient demographics (such as name, birthdate, and address), admission details, medical record numbers, service dates, total charges, and diagnosis codes. Additionally, information on the insurance payer, prior payments, and any treatment authorization codes may also be necessary. It's crucial to ensure that all information is accurate to avoid delays in payment.
How does the UB92 claim process work?
The claim process begins when a healthcare provider completes the UB92 Claim Form after providing services to a patient. This form is then submitted to the appropriate insurance company for reimbursement. The insurance provider reviews the claim for accuracy and checks whether the services are covered under the patient's plan. Upon approval, the insurance company processes the payment, which is sent to the provider. If there are any discrepancies or denials, the provider may need to address issues and resubmit the claim.
What are the common reasons for UB92 claim denials?
Claim denials can occur for various reasons. Some common issues include incomplete or incorrect information on the form, services provided not being covered by the insurance plan, or prior authorization not being obtained when required. Additionally, coding errors or missing documentation can lead to denials. It's essential for providers to review the completed UB92 form thoroughly before submission to minimize the chances of denial.
How can I correct errors on a submitted UB92 form?
If errors are discovered after submission, providers can address this through a few methods. Depending on the insurer's guidelines, they may allow claims to be corrected electronically or via a paper process. If a claim is denied due to errors, providers can submit a corrected claim, noting the changes made. It's important to act promptly, as there are time limits for correcting claims and resubmitting them for payment.
Common mistakes
The UB92 Claim form, also known as the Uniform Bill-92, is essential for healthcare facilities to seek reimbursement from insurers. However, errors often occur when filling it out. One common mistake involves incorrect patient information. Omitting or inaccurately entering the patient’s name, birth date, or address can lead to delays or denials of claims.
Another common error is related to the Patient Control Number. This reference number should be unique for each patient visit. Failing to provide this number or duplicating it among different claims can complicate processing and tracking.
Understanding the statement covers period is important, as it identifies the dates of service. Errors in this area can create confusion for payers regarding the timeframe being billed, resulting in payment issues.
Also problematic is the accurate entry of diagnosis codes. The UB92 form requires precise diagnostic data to justify the treatments and services rendered. Incorrect or vague codes may lead to audits or fraudulent claims allegations.
A further mistake pertains to the total charges section. Inaccurate calculations or failure to include all associated service charges can misrepresent the bill. Such discrepancies can result in either overpayment or underpayment issues.
Additionally, some claimants overlook the need to provide payer information. This includes the insurance provider’s details, which must be accurate and current. Errors can prevent the claim from reaching the right destination.
Another frequent mistake occurs with the entry of prior payments. Not reporting any prior payments made on behalf of the patient can mislead the insurance company regarding the amount owed, impacting reimbursement rates.
The employment information section is sometimes incomplete or inaccurate. Providing the employer’s name and location is crucial, especially for claims related to workplace injuries. Misrepresentation in this regard can lead to claim denial.
Finally, errors often occur in the service date and units fields. If these details do not correlate with the supporting documentation, it may trigger audits or rejections. Always ensure that service dates match the actual treatment dates to foster clear communication with payers.
In summary, filling out the UB92 Claim form requires careful attention to detail. Common mistakes include inaccuracies in patient information, diagnosis codes, total charges, payer information, and service dates. Avoiding these pitfalls can streamline the reimbursement process and minimize delays.
Documents used along the form
The UB92 claim form is a crucial document used in healthcare billing for inpatient services. Along with the UB92 form, various other documents are often required to ensure accurate processing and payment. Below is a list of these documents, each briefly described for clarity.
- CMS-1500 Form: This form is used primarily for outpatient services and is completed by healthcare providers for billing purposes. It contains patient information, service details, and coding relevant to the treatment provided.
- Patient Encounter Form: Also known as a superbill, this document summarizes the services rendered during a visit. It includes diagnostic codes, procedure codes, and charges, aiding in documentation and claim submission.
- Medical Records Documentation: Comprehensive documentation of patient encounters, diagnoses, treatments, and outcomes. This information supports the services billed on the UB92 and helps to justify insurance claims.
- Insurance Verification Form: This form is used to confirm a patient’s insurance coverage prior to service delivery. It helps identify benefits and out-of-pocket costs, streamlining the billing process.
- Authorization Request Form: This document is submitted to insurance companies to obtain pre-approval for certain medical services. It is essential for procedures that require prior authorization before being billed.
- Payment Posting Report: This report details payments received for services rendered and is essential for reconciling accounts. It includes information on payments, adjustments, and denials.
- Claim Denial Letter: This letter is issued by the insurance company when a claim is rejected. It specifies the reasons for denial and typically includes instructions for appealing the decision.
- Appeal Letter: When a claim is denied, a provider may respond with an appeal letter disputing the decision. This document must address the reasons for denial and provide supporting evidence.
- Billing Statement: A statement generated for patients detailing charges for services received, payments made, and any outstanding balances. This document assists patients in understanding their financial responsibilities.
Each of these documents plays a significant role in the healthcare billing process alongside the UB92 claim form. Proper use and completion of these forms ensure timely and accurate reimbursement from insurance providers.
Similar forms
-
CMS-1500 Claim Form: This form is primarily used by healthcare professionals to bill for services provided to patients. Both forms require patient and provider information, diagnosis codes, procedure codes, and payment details. They facilitate the claims submission process for reimbursement from insurance companies.
-
UB-04 Claim Form: The UB-04 is a newer format used for billing similar to the UB92 form. It is designed for institutional providers, such as hospitals. Both forms capture essential information like patient details, service dates, and charges, but the UB-04 includes more fields for additional data collection.
-
Superbill: A superbill is an internal document used by healthcare providers to summarize the services rendered to a patient. While the UB92 is submitted to insurers for claims, a superbill contains similar components, such as service codes and patient information, but is used for billing in a more efficient way internally before claims submission.
-
Medicare Annuity Claim Form: This claim form serves to bill Medicare for provided services. Similar to the UB92, it includes required patient data, provider information, and documentation of services rendered. Both documents aim to secure reimbursement from federal healthcare programs.
-
Workers' Compensation Claim Form: Workers' compensation forms collect detailed information about workplace injury claims. Like the UB92, they require patient identification, reason for the visit, treatment details, and billing amounts. Both forms ensure that medical services related to injury claims are adequately documented and compensated.
Dos and Don'ts
- Do provide accurate patient information, including name, address, and birthdate.
- Don't leave any required fields blank. All necessary information must be filled out.
- Do double-check the Federal Tax Number and patient control number for accuracy.
- Don't use abbreviations unless they are standard and widely accepted.
- Do specify the dates for the coverage period clearly.
- Don't forget to include service dates and units accurately.
- Do ensure the billing name and address match the facility's legal name.
- Don't submit the claim without verifying the insurance group number and other related information.
- Do include all applicable diagnosis and procedure codes.
- Don't overlook the sections for prior payments and remarks if necessary.
Misconceptions
The UB92 Claim Form, also known as the UB-92 or UB-04, plays a crucial role in health care billing, yet several misconceptions surround its usage. Understanding these misunderstandings can improve billing accuracy and enhance the overall reimbursement process.
- Misconception 1: The UB92 form is only for hospitals.
- Misconception 2: Every field on the UB92 must be filled out.
- Misconception 3: The UB92 form is universally accepted by all payers.
- Misconception 4: This form can only be submitted in paper format.
- Misconception 5: Detailed descriptions are not necessary on the UB92.
- Misconception 6: The UB92 is the same as the CMS-1500 form.
- Misconception 7: Coding errors have no significant impact on claims.
- Misconception 8: The form does not require signatures.
- Misconception 9: The UB92 form is outdated and will be replaced soon.
- Misconception 10: Submission of the UB92 guarantees payment.
This form is utilized by a variety of health care facilities, including nursing homes and outpatient care centers. It is not exclusive to inpatient hospital claims.
While many fields are essential, not all sections require completion. Each blank space should be considered based on the specific services rendered and the payer's requirements.
Different insurance companies and government programs may have specific requirements and variations. It is crucial to confirm acceptance prior to submission.
Though traditionally a paper form, the UB92 can be submitted electronically, aligning with modern electronic claims processing standards.
Providing concise and accurate descriptions of services can promote better understanding and timely payment from insurance companies.
The UB92 and CMS-1500 serve different purposes and audiences. The CMS-1500 is generally used for outpatient services provided by physicians, while the UB92 caters to institutional claims.
Accuracy in coding is critical. Errors can lead to claim denials or delays in payment, impacting the cash flow of health care facilities.
A signature from an authorized individual is typically necessary to validate the claim, confirming that the information provided is true and accurate.
While updates may occur, the UB92 continues to be a standard for institutional claims. Ongoing training and familiarity with the form remain essential.
Submitting a claim does not guarantee reimbursement. Several factors, including the validity of services rendered and adherence to payer policies, influence the ultimate payment decision.
Key takeaways
The UB92 claim form is a vital document used in healthcare billing processes. Here are some key takeaways to ensure effective and accurate completion:
- Accurate Information is Essential: Always provide precise details, like the facility’s billing name, patient identification numbers, and service dates. Errors can lead to delays in processing claims.
- Understanding Codes is Crucial: Familiarize yourself with various codes listed on the form, including diagnosis and procedure codes. These codes help convey the nature of services provided.
- Check for Completeness: Ensure all required sections are filled out completely. Missing information can result in denied claims or requests for additional information.
- Stay Up-to-Date: Regulations and requirements for UB92 claims can change. Regularly update your knowledge to remain compliant with current billing practices.
By adhering to these guidelines, you can streamline the claims process and improve the likelihood of successful reimbursements.
Browse Other Templates
Michigan Probate Court Forms - Service fees and miles traveled can be included on the form for reimbursement calculations.
Player Evaluation Form - Examines the skill of finishing in various styles of goal scoring.
Sinai Hospital Medical Records Phone Number - Memorial Hermann staff is authorized to disclose the necessary information per this form.