Fill Out Your Ubh Health Claim Inquiry Form
When dealing with health claims, especially in the realm of behavioral health, clarity and proper procedure are essential for both providers and members. The United Behavioral Health (UBH) Claim Inquiry/Adjustment Request Form serves as a crucial tool designed to facilitate adjustments and inquiries for claims associated with UBH members, including those under PacifiCare Behavioral Health. This form is intended solely for contracted clinicians and hospitals and differentiates between the initial inquiry stage and the more formal dispute process, making it easier for providers to navigate claim issues. Upon completion of the form, providers can seek resolutions for various reasons, such as claims that were denied due to timing issues or requests for additional information. It is vital that the appropriate information, including enrollee IDs and claim details, is included, ensuring a smoother adjustment process. Protecting the interests of providers and members alike, this form emphasizes the importance of timely communication with customer service, where issues can be escalated if necessary. Notably, California providers must be aware that this form is not applicable in their state and should follow alternative protocols outlined in their specific documentation. Understanding how to appropriately use this form can greatly impact the effectiveness of claims management and dispute resolution in behavioral health settings.
Ubh Health Claim Inquiry Example
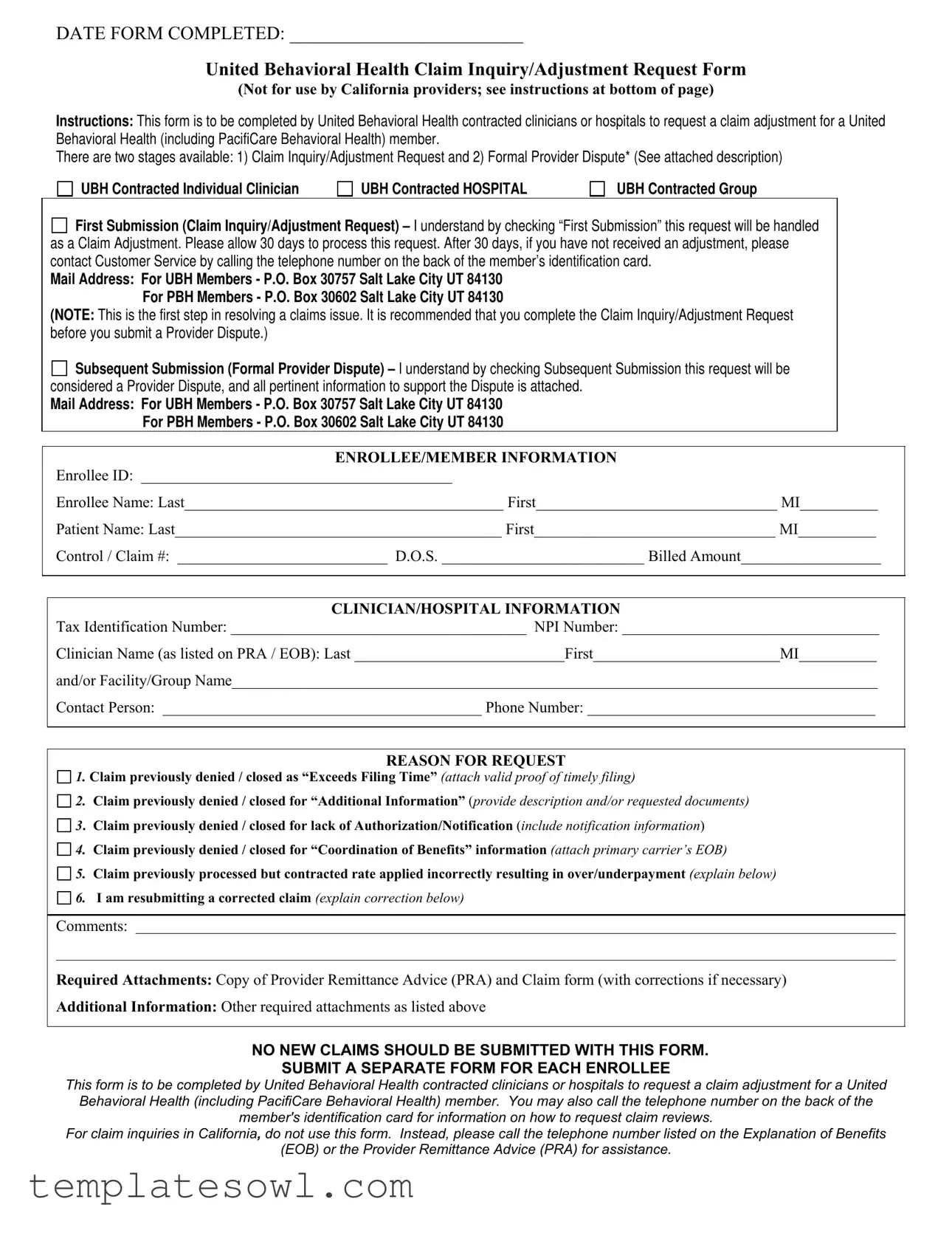
DATE FORM COMPLETED: _________________________
United Behavioral Health Claim Inquiry/Adjustment Request Form
(Not for use by California providers; see instructions at bottom of page)
Instructions: This form is to be completed by United Behavioral Health contracted clinicians or hospitals to request a claim adjustment for a United Behavioral Health (including PacifiCare Behavioral Health) member.
There are two stages available: 1) Claim Inquiry/Adjustment Request and 2) Formal Provider Dispute* (See attached description)
UBH Contracted Individual Clinician
UBH Contracted HOSPITAL
UBH Contracted Group

 First Submission (Claim Inquiry/Adjustment Request) – I understand by checking “First Submission” this request will be handled as a Claim Adjustment. Please allow 30 days to process this request. After 30 days, if you have not received an adjustment, please contact Customer Service by calling the telephone number on the back of the member’s identification card.
First Submission (Claim Inquiry/Adjustment Request) – I understand by checking “First Submission” this request will be handled as a Claim Adjustment. Please allow 30 days to process this request. After 30 days, if you have not received an adjustment, please contact Customer Service by calling the telephone number on the back of the member’s identification card.
Mail Address: For UBH Members - P.O. Box 30757 Salt Lake City UT 84130
For PBH Members - P.O. Box 30602 Salt Lake City UT 84130
(NOTE: This is the first step in resolving a claims issue. It is recommended that you complete the Claim Inquiry/Adjustment Request before you submit a Provider Dispute.)

 Subsequent Submission (Formal Provider Dispute) – I understand by checking Subsequent Submission this request will be considered a Provider Dispute, and all pertinent information to support the Dispute is attached.
Subsequent Submission (Formal Provider Dispute) – I understand by checking Subsequent Submission this request will be considered a Provider Dispute, and all pertinent information to support the Dispute is attached.
Mail Address: For UBH Members - P.O. Box 30757 Salt Lake City UT 84130
For PBH Members - P.O. Box 30602 Salt Lake City UT 84130
ENROLLEE/MEMBER INFORMATION
Enrollee ID: ________________________________________
Enrollee Name: Last_________________________________________ First_______________________________ MI__________
Patient Name: Last__________________________________________ First_______________________________ MI__________
Control / Claim #: ___________________________ D.O.S. __________________________ Billed Amount__________________
CLINICIAN/HOSPITAL INFORMATION
Tax Identification Number: ______________________________________ NPI Number: _________________________________
Clinician Name (as listed on PRA / EOB): Last ___________________________First________________________MI__________
and/or Facility/Group Name___________________________________________________________________________________
Contact Person: _________________________________________ Phone Number: _____________________________________
REASON FOR REQUEST
1. Claim previously denied / closed as “Exceeds Filing Time” (attach valid proof of timely filing)
2. Claim previously denied / closed for “Additional Information” (provide description and/or requested documents)
3. Claim previously denied / closed for lack of Authorization/Notification (include notification information)
4. Claim previously denied / closed for “Coordination of Benefits” information (attach primary carrier’s EOB)
5. Claim previously processed but contracted rate applied incorrectly resulting in over/underpayment (explain below)
6. I am resubmitting a corrected claim (explain correction below)
Comments:
Required Attachments: Copy of Provider Remittance Advice (PRA) and Claim form (with corrections if necessary)
Additional Information: Other required attachments as listed above
NO NEW CLAIMS SHOULD BE SUBMITTED WITH THIS FORM.
SUBMIT A SEPARATE FORM FOR EACH ENROLLEE
This form is to be completed by United Behavioral Health contracted clinicians or hospitals to request a claim adjustment for a United Behavioral Health (including PacifiCare Behavioral Health) member. You may also call the telephone number on the back of the member's identification card for information on how to request claim reviews.
For claim inquiries in California, do not use this form. Instead, please call the telephone number listed on the Explanation of Benefits
(EOB) or the Provider Remittance Advice (PRA) for assistance.
Formal Provider Dispute Process
Your Right to Dispute an Adverse Determination on Your Own Behalf
You or your authorized representative, on your own behalf, have the right to dispute the adverse determination made by United Behavioral Health (UBH). You may initiate this dispute in writing by completing the “UBH Claim Inquiry/Adjustment Request Form” and checking the “Subsequent Submission” checkbox. This will be considered a Formal Provider Dispute.
The First Level Provider Dispute Process
The Provider Dispute process can be initiated for post service requests only.
You must request a Provider Dispute review within one hundred eighty (180) calendar days of the date you received your adverse determination letter from UBH. Disputes received outside of this timeframe will not be processed.
UBH will notify you or your authorized representative of the dispute resolution (including any additional levels of the dispute process, as applicable) in writing within thirty (30) calendar days of the receipt of your request.
If UBH does not receive the minimum necessary information to process your dispute as described above, UBH will send written notice to you within thirty (30) calendar days of our receipt of your request that contains 1) a description of the information needed from you to process your dispute, and 2) a statement that failure to provide the requested information within thirty (30) calendar days of receipt will result in the closure of the request with no further review.
For Colorado Providers, UBH will provide you the opportunity to present your rationale for your dispute in person, or via an alternative method, such as a teleconference.
Form Characteristics
| Fact Name | Details |
|---|---|
| Form Purpose | This form is used by United Behavioral Health (UBH) contracted clinicians or hospitals to request a claim adjustment for a UBH member. |
| Submission Types | There are two submission types: Claim Inquiry/Adjustment Request and Formal Provider Dispute. |
| Mailing Addresses | For UBH Members: P.O. Box 30757, Salt Lake City, UT 84130. For PBH Members: P.O. Box 30602, Salt Lake City, UT 84130. |
| Initial Processing Time | Allow 30 days for processing a Claim Inquiry/Adjustment Request before following up with Customer Service. |
| California Providers | This form is not intended for use by providers in California. They should refer to the telephone number on the EOB or PRA. |
| Dispute Timeframe | A Provider Dispute must be requested within 180 calendar days from the date of the adverse determination letter. |
| Colorado Specifics | Providers in Colorado may present their dispute in person or via teleconference. |
Guidelines on Utilizing Ubh Health Claim Inquiry
Completing the Ubh Health Claim Inquiry form is an important step in addressing any claims-related concerns you may have. Upon submission, relevant teams will review the request and work towards a resolution. Please follow the steps carefully to ensure all necessary information is provided for a timely response.
- Enter the DATE FORM COMPLETED at the top of the form.
- Select the appropriate checkbox for First Submission or Subsequent Submission.
- Provide the ENROLLEE/MEMBER INFORMATION including:
- Enrollee ID
- Enrollee Name (Last, First, MI)
- Patient Name (Last, First, MI)
- Control / Claim Number
- Date of Service (D.O.S.)
- Billed Amount
- Fill in the CLINICIAN/HOSPITAL INFORMATION including:
- Tax Identification Number
- NPI Number
- Clinician Name (Last, First, MI)
- Facility/Group Name
- Contact Person
- Phone Number
- Indicate the REASON FOR REQUEST by checking the applicable box and providing any required details.
- Include specific COMMENTS related to the request.
- Attach any required documentation such as:
- Provider Remittance Advice (PRA)
- Claim form with corrections, if necessary
- Confirm that you are submitting a SEPARATE FORM for each enrollee, if necessary.
- Mail the completed form to the appropriate address based on the member type.
What You Should Know About This Form
What is the purpose of the UBH Health Claim Inquiry form?
This form is designed for United Behavioral Health (UBH) contracted clinicians or hospitals. It allows them to request a claim adjustment for a UBH member’s claim. The form can be used for various reasons, including previously denied claims and incorrect payment amounts.
Who should complete the form?
The form must be completed by clinicians or hospitals that are contracted with UBH. It is essential that those filling out the form are associated with a UBH member and have the necessary information for the claim.
What are the two submission types available on the form?
There are two submission types: First Submission and Subsequent Submission. The First Submission indicates that the request is a Claim Inquiry/Adjustment Request. The Subsequent Submission indicates that it is a Formal Provider Dispute. Each type has different processing routes and timelines.
How long will it take to process my claim inquiry request?
Please allow up to 30 days for your Claim Inquiry/Adjustment Request to be processed. If you do not receive an adjustment after this period, you should contact Customer Service using the number on the back of the member’s identification card.
What should I include when filling out the form?
When completing the UBH Claim Inquiry form, you should include details such as enrollee ID, patient name, the control/claim number, billed amount, and the reason for your request. Additionally, attach the necessary documents, like the Provider Remittance Advice and any supporting evidence for your request.
Can I submit a new claim with this form?
No, you should not submit a new claim using this form. It is specifically for requesting adjustments to existing claims. For new claims, a separate submission is required.
What if my claim was denied due to “Exceeds Filing Time”?
If your claim was denied for “Exceeds Filing Time,” you must attach valid proof of timely filing to your inquiry. This documentation is critical for processing your request successfully.
What happens if I submit my dispute after 180 days?
If you submit a provider dispute more than 180 days after receiving the adverse determination letter, UBH will not process your request. It is vital to adhere to this timeframe to ensure your dispute is considered.
Is there support available if I need help with the form?
Yes, you can contact Customer Service by calling the telephone number found on the back of the member's identification card for assistance. For claims inquiries in California, it is best to refer to the number on the Explanation of Benefits or the Provider Remittance Advice.
What will happen after I submit a formal provider dispute?
After submitting a formal provider dispute, UBH will notify you of the resolution within 30 days. If any additional information is needed, they will communicate that to you as well.
Common mistakes
Completing the United Behavioral Health Claim Inquiry form can seem straightforward, yet common mistakes often lead to delays in processing. Recognizing these pitfalls is essential for ensuring a smooth submission process.
One frequent error is failing to include the Enrollee ID.
This identification number is critical for establishing the member's account and processing the request efficiently. Without it, claims may be delayed or even denied entirely. Ensure the ID is accurately filled out to avoid unnecessary complications.
Another common mistake is not selecting the appropriate submission type: First Submission versus Subsequent Submission.
Choosing the wrong option can alter the nature of your request and the urgency with which it is handled. Understanding that the First Submission treats the request as a claim adjustment while the Subsequent Submission is a formal dispute is crucial. Misidentification here can lead to further misunderstandings.
Inadequate documentation is also a major issue.
Providers often neglect to attach required documents, such as the Provider Remittance Advice or the necessary records supporting the claim. Submitting a complete package is vital; if any necessary documents are missing, the request may be returned or disregarded altogether.
Finally, many individuals overlook the reason for the request.
Providing a clear, concise explanation of why the claim is being questioned helps expedite the review process. Without this context, claims may sit unresolved for longer periods, causing frustration for everyone involved. Make sure to provide detailed and accurate reasons for inquiries to facilitate swift resolution.
Avoiding these mistakes will not only help in the timely processing of claims but will also reduce the likelihood of disputes in the future.
Documents used along the form
When navigating the claims process with United Behavioral Health, several forms and documents may accompany the Ubh Health Claim Inquiry form. Each of these documents serves a specific purpose in ensuring a thorough review and resolution of your claims. Here is a summary of commonly used forms and documents:
- Claim Form: This document provides a detailed account of the services rendered and the charges incurred. It is essential for initiating claims with UBH.
- Provider Remittance Advice (PRA): This statement outlines the claims paid by UBH, including any adjustments or denials. It serves as a crucial reference for understanding payment breakdowns.
- Explanation of Benefits (EOB): An EOB is issued after the claim is processed, showing how the claim was adjudicated. It includes details on what was covered under the policy and outlines any outstanding patient obligations.
- Authorization Request Form: This form is used to obtain pre-approval for specific services before they are rendered. It ensures that the services are covered under the member’s plan.
- Appeal Form: If a claim is denied, the appeal form allows for a formal request to review the claim decision. This is typically used after the initial claim inquiry.
- Patient Information Release Form: This document grants permission for the release of the patient’s medical information to assist in processing the claim or appeal.
- Coordination of Benefits Form: This form is necessary when a member has multiple insurance coverages. It clarifies which insurance should be billed first.
- Dispute Resolution Form: This form initiates the formal process to dispute adverse determinations and allows for the submission of additional information or rationale.
- Additional Documentation Attachments: This includes any documents required to support the claim, such as medical records, notes, or previous correspondence related to the claim.
- Claim Adjustment Request Form: Separate from the initial claim inquiry, this form specifically requests changes or additional considerations for already submitted claims.
Using the appropriate forms and documentation can significantly impact the efficiency and effectiveness of the claims process. Attaching all necessary information helps ensure that your concerns are addressed promptly and accurately.
Similar forms
Insurance Claim Form: Much like the Ubh Health Claim Inquiry form, an insurance claim form is used to request benefits for covered services. Both require details about the patient, clinician or facility involved, and the nature of the services provided.
Claim Adjustment Request Form: This document is directly related to the Ubh form. It's submitted when there is a need to correct or adjust a previously submitted claim, focusing on issues such as billing errors or missing documentation.
Provider Dispute Form: Similar in purpose, this form allows providers to formally dispute a claim denial. While the Ubh form can initiate the inquiry, the Provider Dispute Form takes it a step further if the initial inquiry does not yield desired results.
Explanation of Benefits (EOB): The EOB outlines what services were covered, the amount billed, and any denied claims. Reviewing an EOB is crucial before completing the Ubh form, as it provides important details regarding the claim status.
Denial Letter: When a claim is denied, a denial letter is issued. This document provides reasons for the denial and essential information that can help guide the completion of the Ubh Claim Inquiry form.
Appeal Form: This document serves a similar purpose to the Ubh form, allowing an individual or provider to formally contest a decision regarding a claim. It usually requires a detailed account of the reasons for the appeal.
Patient Authorization Form: In cases where patient consent is necessary, this form provides the clinician permission to access or share medical records with the insurance company. This is integral for correctly processing claims.
Claim Review Request Form: Like the Ubh form, this document is utilized to request a review of a claim that is under dispute. It emphasizes gathering further details to ensure accurate claim processing.
Dos and Don'ts
When filling out the Ubh Health Claim Inquiry form, it's important to follow specific guidelines to ensure a smooth process. Here are some dos and don'ts to keep in mind:
- Do ensure that you indicate whether it is a First Submission or Subsequent Submission clearly.
- Do provide complete enrollee and patient information, including ID and names.
- Do attach all required documents, such as the Provider Remittance Advice.
- Do specify the reason for the claim inquiry accurately from the provided options.
- Do keep a copy of the submitted form and attachments for your records.
- Don't submit new claims using this form; a separate form is required for each enrollee.
- Don't leave any sections blank that are required, as this may delay processing.
- Don't forget to check that the contact information is current and accurate.
- Don't assume that a verbal request will suffice; written documentation is necessary.
- Don't wait longer than 180 calendar days to initiate a dispute if you're addressing an adverse determination.
Misconceptions
Misunderstandings about the Ubh Health Claim Inquiry form can lead to unnecessary complications. Here are ten common misconceptions, clarified for better understanding:
- Form Use Is Universal: Many believe this form is for all providers. However, it must not be used by California providers. They should refer to specific instructions instead.
- Only New Claims Can Be Filed: A frequent misconception is that this form can be used for new claims. In reality, it is strictly for requesting adjustments on existing claims.
- Processing Time Is Immediate: Extra caution is necessary. Though adjustments should be processed within 30 days, delays can occur, requiring follow-up with customer service.
- One Form Is Enough for Multiple Claims: Some providers think they can submit multiple inquiries on a single form. This is incorrect. A separate form is required for each enrollee.
- Any Reason Can Be Provided for Adjustments: Not every reason is valid for submission. The form outlines specific reasons that are accepted for claim adjustments.
- Automatic Acknowledgment of Submission: Providers often expect confirmation upon submission. However, it is advisable to contact customer service if no communication is received within the processing timeframe.
- Attachments Are Optional: Some assume that they can skip necessary documentation. This is misleading. Required attachments, like the Provider Remittance Advice and claim form, are essential for processing.
- Claim Inquiry Automatically Becomes a Dispute: Submitting a claim inquiry does not automatically escalate to a formal dispute. It must be clearly marked and submitted under the correct category.
- Disputes Can Be Filed Anytime: Providers often think they can dispute at their convenience. However, disputes must be initiated within 180 days of receiving an adverse determination letter.
- All Disputes Follow the Same Process: Not all disputes have the same resolution timeline or requirements. It's essential for providers to understand the specific process applicable to their situation for effective resolution.
Key takeaways
Filling out and using the Ubh Health Claim Inquiry form can be straightforward if you follow these key points.
- The form is specifically for United Behavioral Health contracted clinicians or hospitals to request a claim adjustment.
- There are two main submission options: the "First Submission" for claim adjustments and the "Subsequent Submission" for formal provider disputes.
- Be sure to provide all required details, including the enrollee's ID, control/claim number, and billed amount, to avoid processing delays.
- Submit a separate form for each enrollee; do not include new claims on this form.
Browse Other Templates
How to Fill Out Affidavit for Collection of Personal Property California - This form allows heirs to receive property directly if certain criteria are met within the California Probate Code.
Desjardins Insurance Health - Completing the DFS-12 accurately helps forensic scientists focus on the analysis of the evidence.