Fill Out Your Umr Ez Claim Form
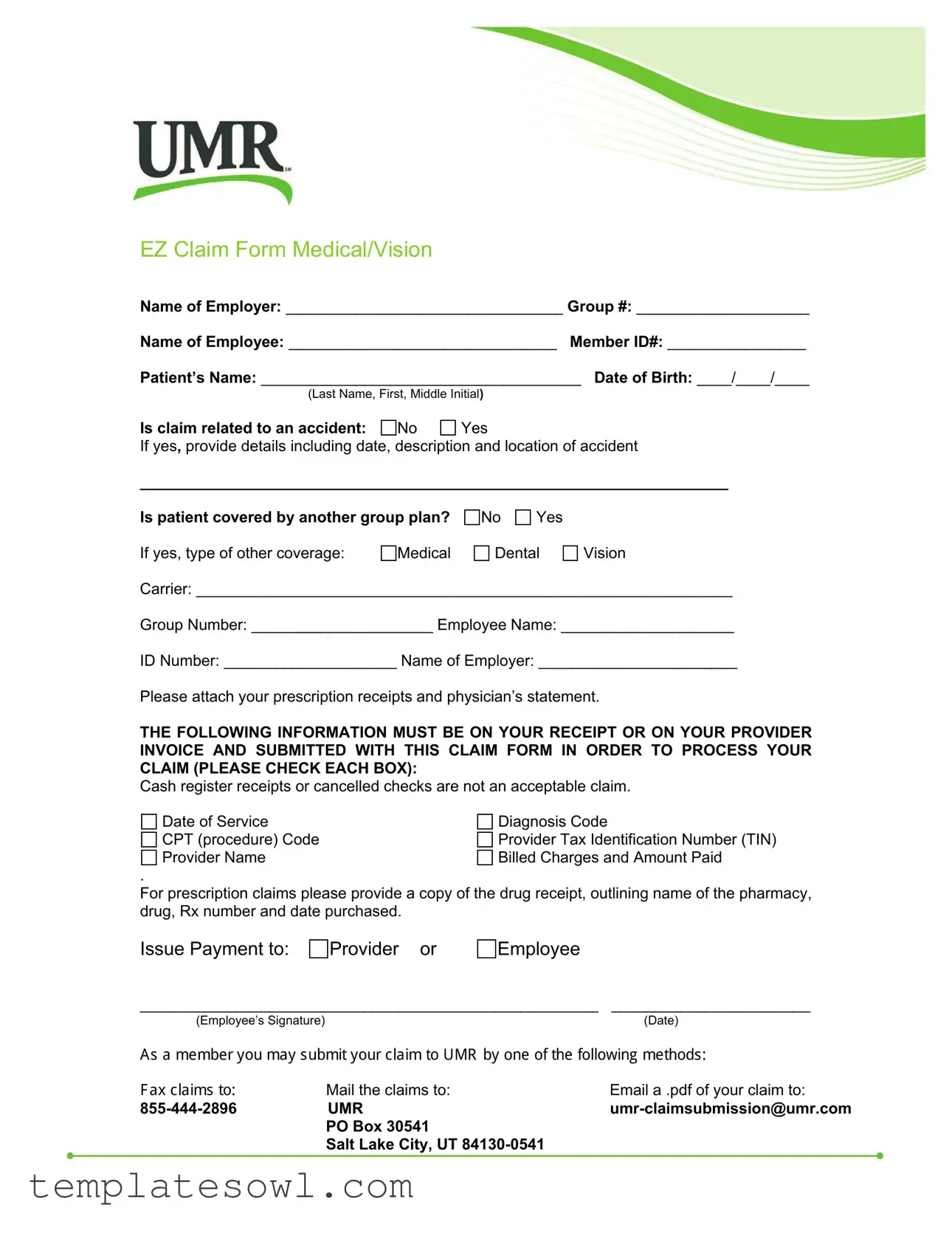
The UMR EZ Claim form plays a pivotal role in simplifying the claims process for medical and vision expenses. Designed to efficiently gather essential information, this form includes fields for the name of the employer, group number, and employee details, such as member ID and patient information. It prompts users to clarify whether the claim is related to an accident and requires details if applicable. Coverage under another group plan is also addressed, ensuring all pertinent information is available for processing. To expedite the claims procedure, individuals must attach prescription receipts and a physician's statement, highlighting the need for specific documentation. The necessary items must be verified for compliance, including diagnosis codes, procedure codes, and the provider's tax identification number. This structured approach aims to deliver a clear pathway for claims submission, with options available for payment to either the provider or the employee. Accessible methods for submission include mailing the completed form or emailing a PDF, reinforcing UMR's commitment to customer convenience in navigating healthcare claims.
Umr Ez Claim Example
EZ Claim Form Medical/Vision
Name of Employer: ________________________________ Group #: ____________________
Name of Employee: _______________________________ Member ID#: ________________
Patient’s Name: _____________________________________ Date of Birth: ____/____/____
(Last Name, First, Middle Initial)
Is claim related to an accident: |
No |
Yes |
If yes, provide details including date, description and location of accident
____________________________________________________________________
Is patient covered by another group plan?
No
Yes
If yes, type of other coverage: |
Medical |
Dental |
Vision |
Carrier: ______________________________________________________________
Group Number: _____________________ Employee Name: ____________________
ID Number: ____________________ Name of Employer: _______________________
Please attach your prescription receipts and physician’s statement.
THE FOLLOWING INFORMATION MUST BE ON YOUR RECEIPT OR ON YOUR PROVIDER INVOICE AND SUBMITTED WITH THIS CLAIM FORM IN ORDER TO PROCESS YOUR CLAIM (PLEASE CHECK EACH BOX):
Cash register receipts or cancelled checks are not an acceptable claim.
Date of Service |
Diagnosis Code |
CPT (procedure) Code |
Provider Tax Identification Number (TIN) |
Provider Name |
Billed Charges and Amount Paid |
.
For prescription claims please provide a copy of the drug receipt, outlining name of the pharmacy, drug, Rx number and date purchased.
Issue Payment to:
Provider or
Employee
_____________________________________________________ |
_______________________ |
|
(Employee’s Signature) |
|
(Date) |
$VDPHPEHU\RXPD\VXEPLW\RXUFODLPWR80 E\RQHRIWKHIROORZLQJPHWKRGV |
||
)D[FODLPVWRMail the claims to: |
Email a .pdf of your claim to: |
|
UMR |
||
|
PO Box 30541 |
|
|
Salt Lake City, UT |
|
Form Characteristics
| Fact Name | Details |
|---|---|
| Name of the Form | The form is called the EZ Claim Form for Medical and Vision claims. |
| Employer Information | Employees must provide the name of their employer and the corresponding group number on the form. |
| Accident Information | Claimants must indicate if the claim is related to an accident, providing specific details if applicable. |
| Other Coverage | If the patient is covered by another group plan, additional information regarding that coverage must be included. |
| Required Documentation | A valid claim requires supporting documents, including diagnosis codes and the provider’s tax identification number. |
| Submission Methods | Claims can be submitted via mail or email as a .pdf file to UMR, and a fax option is also available. |
Guidelines on Utilizing Umr Ez Claim
Completing the UMU Ez Claim form involves providing specific information about the patient, employer, and details related to the claim. You will need to gather receipts and documentation to accompany the form. Follow these steps carefully to ensure a successful submission.
- Begin by filling out the Name of Employer field at the top of the form.
- Next, enter the Group # assigned to the employer.
- Input the Name of Employee and their Member ID#.
- In the Patient’s Name section, provide the last name, first name, and middle initial of the patient.
- Record the patient’s Date of Birth in the format of day/month/year.
- Indicate whether the claim is related to an accident by checking the corresponding Yes or No box.
- If applicable, provide details about the accident, including the date, description, and location.
- Answer whether the patient is covered by another group plan by checking Yes or No.
- If the patient has other coverage, specify the type (Medical, Dental, Vision) and fill in the Carrier and Group Number.
- List the Employee Name and their ID Number associated with the other coverage.
- Document the Name of Employer for the other coverage, if any.
- Remember to attach prescription receipts and a physician’s statement to your submission.
- Check the boxes to ensure the following details are included on your receipt: Date of Service, Diagnosis Code, CPT (procedure) Code, Provider Tax Identification Number (TIN), Provider Name, Billed Charges and Amount Paid.
- For prescriptions, include a copy of the drug receipt containing the pharmacy name, drug, Rx number, and date purchased.
- Decide who to issue payment to: the Provider or Employee, and fill in that information on the form.
- Have the Employee sign the form and date it as required.
- Choose the method of submission: mail, email, or fax, and follow the instructions provided to send it to UMR.
What You Should Know About This Form
What is the purpose of the UMR EZ Claim form?
The UMR EZ Claim form serves as a means for employees to submit medical or vision claims for reimbursement. This form captures necessary details, including the patient's information, dates of service, and amounts paid. A well-completed form ensures that claims are processed promptly and accurately, facilitating timely reimbursements for health-related expenses.
What information must be included when submitting the claim?
To successfully process your claim, specific information must be included on the form and supporting documents. This includes the patient's name, date of birth, diagnosis code, procedure code, provider's name and Tax Identification Number (TIN), and details of the billed charges. Additionally, receipts from prescriptions and a physician's statement must accompany the claim. Receipts from cash registers or canceled checks are not accepted, so make sure that you include valid documents to avoid delays.
How should I submit the completed UMR EZ Claim form?
Once you have completed the UMR EZ Claim form and gathered all required documents, you have several options for submission. You can mail the claims to UMR at their dedicated address: PO Box 30541, Salt Lake City, UT 84130-0541. Alternatively, if you prefer a quicker method, you may email a PDF copy of your claim to umr-claimsubmission@umr.com or fax it to 855-444-2896. It is essential to keep a copy for your records and ensure all documents are legible and complete.
What happens if my claim is denied or requires additional information?
If your claim is denied or additional information is needed, you will receive a notification outlining the reasons for denial or what further details are necessary. It is crucial to review this communication carefully and respond promptly to any requests. If you believe the denial was an error, you can appeal the decision, providing any further information or documentation as needed. Engaging with the claims department can often clarify misunderstandings and assist in resolving issues to secure the benefits you deserve.
Common mistakes
Completing the UMR EZ Claim form can sometimes be challenging. There are several common mistakes that individuals may encounter.
One error is failing to provide all requisite information. It is essential to fill in every blank accurately, including the name of the employer, group number, member ID, and patient details. Incomplete fields can lead to delays in processing the claim.
Another frequent mistake is not attaching the necessary documentation. Receipts and physician statements are required for processing a claim. Without them, claims may be denied. It is important to remember that cash register receipts and canceled checks are not accepted.
Some individuals overlook the importance of including the correct diagnosis code and CPT procedure code. These items are critical for determining the nature of the claim. Missing or incorrect codes can result in claim rejection.
Additionally, failing to indicate whether the claim is related to an accident can cause complications. If the answer is "Yes," providing detailed information about the accident, including date, description, and location, is crucial.
Another common mistake is not selecting a payment method. Claimants need to specify whether the payment should be directed to the provider or themselves. This choice must be clearly indicated on the form to ensure proper payment processing.
Lastly, individuals might neglect to double-check their provided contact information. Errors in contact details can mean that claims are delayed as follow-up may be necessary. Verifying that all information is accurate before submission will help streamline the process.
Documents used along the form
The UMR EZ Claim form is a crucial document for submitting claims related to medical or vision services. To effectively process these claims, various other forms and documents may be required. Each document plays a specific role in the claims process, ensuring that all necessary information is available for a timely review and approval.
- Patient Authorization Form: This document grants permission for the insurance company to access the patient’s medical records. It ensures compliance with privacy regulations and is essential for processing claims involving sensitive health information.
- Physician’s Statement: Often required to validate the medical necessity of the treatment provided, this statement is completed by the healthcare provider. It includes the diagnosis and the rationale for the services rendered.
- Prescription Receipts: For claims related to medications, receipts indicate the details of the purchased drugs, including the pharmacy name and Rx numbers. This documentation is necessary to support claims for prescription coverage.
- Secondary Insurance Claim Form: If the patient is covered by another insurance plan, this form is used to file for additional coverage. It captures relevant details about the secondary insurance provider and any payments made.
- Explanation of Benefits (EOB): Issued by the insurance company, the EOB outlines the services covered, the amount billed, and the patient’s financial responsibility. It is helpful in clarifying what portions of the claim have been processed.
- Personal Injury Information Form: If a claim is related to an accident or injury, this form details the circumstances surrounding the event. It may include specific information about the accident and any involved parties.
- Claim Checklist: This document serves as a summary guide to ensure that all required pieces of information are submitted with the claim. It helps prevent delays by ensuring that all necessary forms are included.
Each of these documents is integral to the claims submission process, aiding in proper communication between patients, providers, and insurance companies. Ensuring their accuracy and completeness can significantly influence the outcome of a claim.
Similar forms
-
Insurance Claim Form: Much like the Umr Ez Claim form, an insurance claim form is used to submit claims for coverage reimbursement. It requires basic information such as the patient's details, the nature of the service, and any relevant diagnosis codes. Both forms emphasize the necessity of receipts and provider details to ensure proper processing of claims.
-
Medical Reimbursement Request Form: This document serves a similar function as the Umr Ez Claim form in requesting reimbursement for medical expenses. It typically includes sections for patient information and details about the medical services provided, along with a need for supporting documentation, like receipts and treatment descriptions.
-
Vision Care Claim Form: A vision care claim form is akin to the Umr Ez Claim form but specifically for eye care claims. It necessitates the same type of information about the patient and provider, and often requires evidence of the expenses incurred, such as receipts from the optometrist or ophthalmologist.
-
Pharmacy Claim Form: Similar to the Umr Ez Claim form, the pharmacy claim form is specifically designed for prescription claims. It captures necessary information such as the name of the medication, pharmacy details, and the date of the prescription, stressing the importance of receipts or invoices for verification.
Dos and Don'ts
Filling out the UMR EZ Claim form may seem straightforward, but attention to detail is crucial. Here are seven important dos and don'ts to keep in mind.
- Do ensure all sections of the form are completed accurately.
- Do provide your employer’s name and group number correctly.
- Do include all relevant patient information, including date of birth.
- Do attach all necessary documents, like prescription receipts and the physician's statement.
- Do verify that all required information is printed clearly on your receipts.
- Don't submit cash register receipts or canceled checks as your proof of payment.
- Don't forget to sign and date the form before submitting.
By following these guidelines, you can help ensure your claim is processed without delay. Ensure all documentation is complete and legible to avoid complications. Start the process promptly to meet claim submission deadlines. Each detail matters when it comes to securing your benefits. Stay organized and diligent.
Misconceptions
Misconceptions about the UMR EZ Claim form can lead to errors and delays in processing claims. Here are seven common misunderstandings and clarifications to help navigate the process.
- All types of receipts are acceptable. Many believe that any receipt is valid. In reality, only specific documents, such as prescription receipts or provider invoices, can be accepted for processing a claim.
- The form does not require detailed information about accidents. Some think they only need to note if an accident occurred. If the claim is accident-related, they must provide details about the event.
- Claims can be submitted without required information. There is an assumption that incomplete submissions will still be considered. However, all requested information must be included, or the claim may be rejected.
- Cash register receipts are sufficient evidence. It's a common misconception that cash register receipts or cancelled checks suffice. These types of documents cannot be used to support a claim; proper invoices must be submitted.
- There is no time limit for submission. Some individuals think they can submit claims at any time. Each claim must be submitted within a specified time frame; failing to do so could result in denial.
- Only the employee can submit the claim. Many believe that only the employee is allowed to submit claims. In actuality, providers can also submit on behalf of the employee, simplifying the process.
- The claim submission process is the same for all types of coverage. Some assume that the process is uniform. Different types of claims, such as medical or vision, may have distinct requirements during submission.
Understanding these misconceptions is crucial in ensuring a smooth claim process and timely reimbursements. Always refer to the guidelines provided with the UMR EZ Claim form for the most accurate information.
Key takeaways
When using the UMR EZ Claim form, be aware of the following important points:
- Employer Information: Clearly fill in the name of your employer and the group number at the top of the form.
- Patient Details: Provide accurate information about the patient, including the full name and date of birth.
- Accident Inquiry: Indicate if the claim is related to an accident. If yes, give detailed information regarding the date, description, and location of the accident.
- Other Insurance Coverage: Disclose if the patient has coverage from another group plan. This is critical for processing the claim correctly.
- Receipt Requirements: Ensure all receipt and invoice information is complete. Claims will not be processed without key details, including the date of service and provider information.
- Prescription Claims: For prescription reimbursements, attach a copy of the drug receipt, which must include the pharmacy’s name, drug, Rx number, and purchase date.
- Payment Instructions: Specify to whom the payment should be directed—either to the provider or to the employee.
- Submission Methods: Choose your submission method wisely; claims can be mailed or emailed as a PDF to expedite processing.
- Timely Submission: Submit your claim promptly to ensure that it is processed without unnecessary delays.
Browse Other Templates
Uva Financial Aid - Remember to attach all required documentation, as incomplete forms may delay assistance.
How to Get Va Disability - Applicants should also provide multiple phone numbers for effective communication.
Ud100 - The plaintiff must specify whether the claim is a limited or unlimited civil case based on the amount demanded.