Fill Out Your Upmc Auth Form
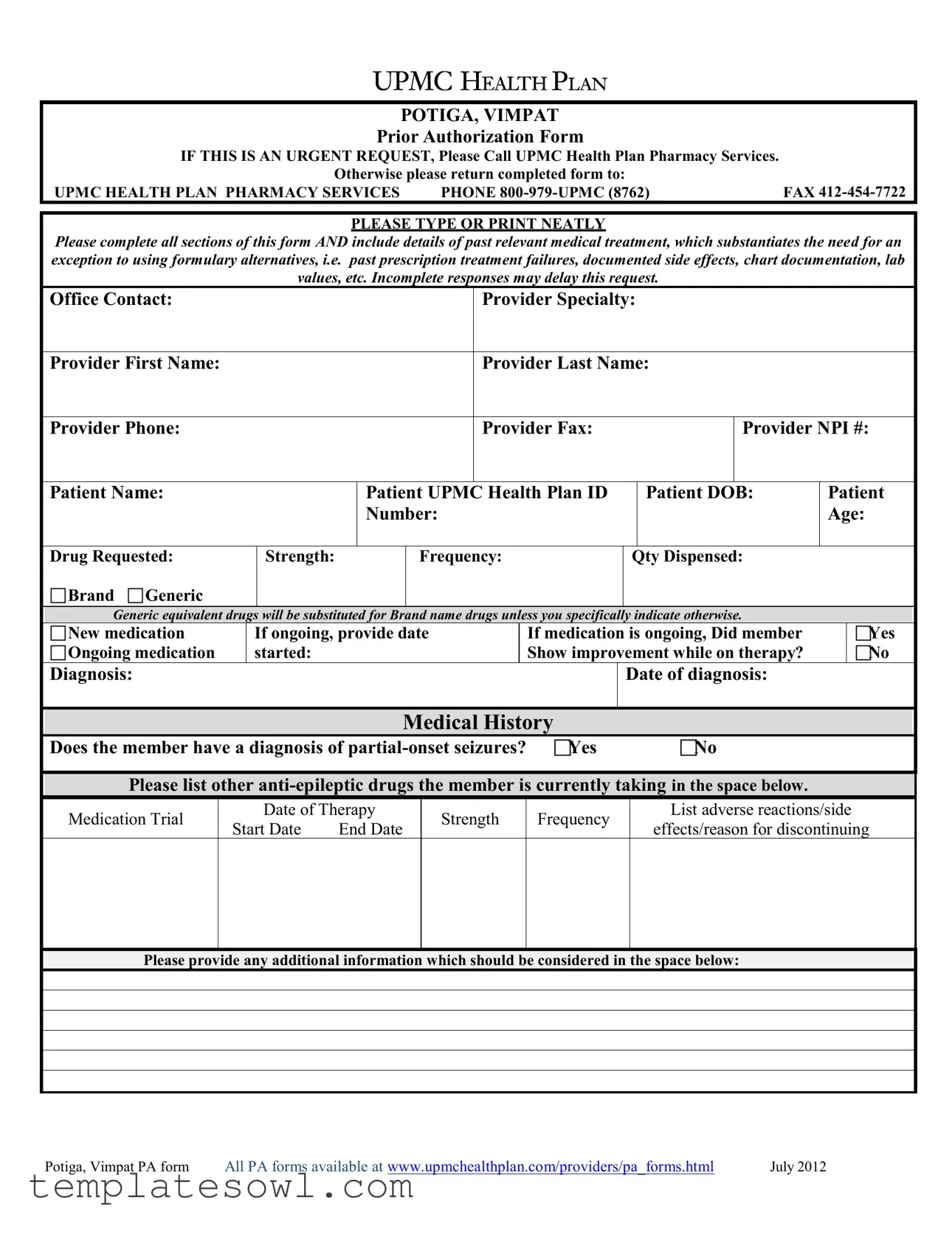
The UPMC Auth form for Potiga and Vimpat is an essential document for healthcare providers seeking prior authorization for these medications. It serves as a formal request to obtain coverage for specific treatment options that may not be included in the standard formulary. To ensure a smooth authorization process, the form requires a thorough completion of all sections. Practitioners must provide detailed information regarding the patient's medical history, including any past treatments attempted, documented side effects, and lab values that justify the need for these particular drugs. Additionally, essential patient information—such as their name, date of birth, and UPMC Health Plan ID—must be accurately recorded. The form also includes a section to describe the requested drug, specifying whether it is a new or ongoing medication and detailing its frequency and dosage. Should the medication be ongoing, the provider must indicate the start date and whether the patient has shown any improvement while on therapy. Furthermore, it is critical to note any other anti-epileptic drugs the patient is taking, along with reasons for discontinuation if applicable. Failure to provide complete information may result in delays, making accuracy and clarity paramount in this process. For urgent requests, providers are encouraged to contact UPMC Health Plan Pharmacy Services directly, ensuring timely attention to patient needs.
Upmc Auth Example
POTIGA, VIMPAT
Prior Authorization Form
IF THIS IS AN URGENT REQUEST, Please Call UPMC Health Plan Pharmacy Services. |
|
|
Otherwise please return completed form to: |
|
|
UPMC HEALTH PLAN PHARMACY SERVICES |
PHONE |
FAX |
PLEASE TYPE OR PRINT NEATLY
Please complete all sections of this form AND include details of past relevant medical treatment, which substantiates the need for an exception to using formulary alternatives, i.e. past prescription treatment failures, documented side effects, chart documentation, lab values, etc. Incomplete responses may delay this request.
Office Contact:
Provider Specialty:
Provider First Name:
Provider Last Name:
Provider Phone:
Provider Fax:
Provider NPI #:
Patient Name:
Patient UPMC Health Plan ID Number:
Patient DOB:
Patient
Age:
Drug Requested:
Brand Generic
Strength:
Frequency:
Qty Dispensed:
Generic equivalent drugs will be substituted for Brand name drugs unless you specifically indicate otherwise.
New medication
Ongoing medication
If ongoing, provide date started:
If medication is ongoing, Did member Show improvement while on therapy?
Yes No
Diagnosis:
Date of diagnosis:
Medical History
Does the member have a diagnosis of
Please list other
Medication Trial
Date of Therapy
Start Date |
End Date |
Strength
Frequency
List adverse reactions/side
effects/reason for discontinuing
Please provide any additional information which should be considered in the space below:
Potiga, Vimpat PA form |
All PA forms available at www.upmchealthplan.com/providers/pa_forms.html |
July 2012 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Urgent Requests | If a request is urgent, it's essential to call UPMC Health Plan Pharmacy Services directly for prompt assistance instead of submitting the form. |
| Required Information | Completion of all sections is crucial. Details about past relevant medical treatments, such as previous prescription failures or documented side effects, must be included to avoid delays. |
| Medication Type | The form allows for the request of either brand or generic medication, with a reminder that generic alternatives will be substituted unless otherwise specified. |
| Patient Information | Key patient details, such as name, UPMC Health Plan ID, date of birth, and age, must be clearly provided to facilitate the authorization process. |
| Other Medications | Information on other anti-epileptic drugs currently being taken by the patient must be detailed, including the medication's trial dates, strengths, and any adverse reactions experienced. |
Guidelines on Utilizing Upmc Auth
Filling out the UPMC Authorization Form correctly is crucial for ensuring timely processing. Gather all necessary patient and provider information before beginning. Accuracy is key to avoid delays in approval, so please double-check each section.
- Begin by indicating whether this is an urgent request. If so, call UPMC Health Plan Pharmacy Services.
- Print or type neatly throughout the form.
- Fill in the Office Contact details.
- Enter the Provider Specialty.
- Provide the Provider’s First and Last Name.
- List the Provider’s Phone Number and Fax Number.
- Include the Provider NPI Number.
- Complete the patient section with the Patient Name, UPMC Health Plan ID Number, and Patient Date of Birth (DOB).
- Fill in the Patient Age.
- Specify the Drug Requested and indicate whether it is Brand or Generic.
- Note the Strength of the medication required.
- Indicate the Frequency of the medication.
- State the Quantity Dispensed.
- Select whether this is a New medication or Ongoing medication.
- If the medication is ongoing, provide the Date Started.
- If medication is ongoing, answer whether the member showed improvement while on therapy by selecting Yes or No.
- Provide the Diagnosis and the corresponding Date of Diagnosis.
- Indicate whether the member has a diagnosis of partial-onset seizures by selecting Yes or No.
- List other anti-epileptic drugs the member is currently taking in the provided space.
- For each medication, include the Trial Date, Start Date, End Date, Strength, and Frequency.
- Document any adverse reactions or side effects, as well as reasons for discontinuation.
- Provide any additional information that should be considered in the designated space.
- Check to confirm that all sections of the form are completed.
- Return the completed form via FAX to 412-454-7722 or call if it is an urgent request.
What You Should Know About This Form
What is the purpose of the UPMC Auth form for Potiga and Vimpat?
The UPMC Auth form is a prior authorization request needed to obtain approval for prescribing Potiga or Vimpat. These medications may not be covered under the standard formulary, and the form helps demonstrate the medical necessity for using these specific drugs, especially if other treatments have failed or caused adverse effects.
How do I submit the UPMC Auth form?
You can submit the completed UPMC Auth form by fax or directly contacting the UPMC Health Plan Pharmacy Services. For fax submissions, use the number 412-454-7722. If your request is urgent, it’s best to call the pharmacy services number at 800-979-UPMC (8762) for immediate assistance.
What information is required to complete the form?
In order to complete the UPMC Auth form, you'll need to provide detailed information about the provider and patient, including the provider's specialty, name, contact numbers, and NPI number. You also need to document the patient's medical history, including any prior treatments for seizures and the reasons for any discontinuation of medications, as well as details about the current request.
What happens if I leave sections of the form incomplete?
If any sections of the form are left incomplete, it may lead to delays in the processing of your request. It’s crucial to provide comprehensive details and to explain the necessities, such as past prescription failures or side effects that justify the need for the requested drug.
Can I request a brand name drug instead of a generic?
Yes, you can specifically indicate your preference for a brand name drug on the form. However, if you do not specify, the pharmacy will typically substitute a generic equivalent for the brand name medication. Clearly specifying your preference helps ensure that your request is aligned with your patient's needs.
What additional information should I include if the medication is ongoing?
If the medication is ongoing, it’s important to provide the date the treatment started. Additionally, indicating whether the member has shown improvement while on therapy helps support the case for continued coverage of the medication.
Where can I find more prior authorization forms?
All prior authorization forms, including the Potiga and Vimpat forms, are available on the UPMC Health Plan website. You can access these forms by visiting www.upmchealthplan.com/providers/pa_forms.html for a comprehensive list of options.
Common mistakes
When filling out the UPMC Authorization Form for Potiga or Vimpat, individuals often encounter various pitfalls that can lead to delays or denials in their medication requests. Understanding these common mistakes can help streamline the submission process and ensure timely access to necessary treatments.
Failure to Complete All Sections is a frequent error. Each section of the form is designed to gather essential information. Omitting details such as the patient's name or provider contact information creates gaps that can hinder the authorization process. By ensuring every field is filled out, applicants reduce the likelihood of delays.
Another mistake is not including relevant medical history. The form explicitly requests details about past treatments and experiences related to the medication. Failing to provide specific information about prior treatment failures, side effects, or lab results may lead the reviewer to question the necessity of the requested medication.
Some applicants often neglect to specify whether the medication is new or ongoing. This distinction is crucial, as ongoing medications typically require documentation of improvement during therapy. If the request pertains to ongoing treatment, indicating the date started and responses to therapy becomes vital to justifying the authorization.
A common oversight involves not listing all current medications. Clearly documenting other anti-epileptic drugs the member is taking helps healthcare providers assess the appropriateness of the requested medication. Incomplete medication lists may result in conflicts with existing treatments or unnecessary delays in the authorization process.
Many individuals also fail to detail adverse reactions or side effects. This information supports the justification for the requested medication, especially if a member has previously tried alternative treatments. Including this data emphasizes the medical necessity of the request and demonstrates a well-considered approach to patient care.
Inadequately completing the diagnosis section is another issue. Providing a clear diagnosis and the date it was confirmed is vital. This information helps the reviewing authority understand the member’s condition and assess whether the prescribed medication aligns with the diagnosis.
Some applicants may not provide additional information as requested in the form. This space allows for contextual data that can support the necessity of the medication, including special circumstances or further justification for using a non-formulary drug. Utilizing this opportunity can strengthen the request significantly.
Lastly, forgetting to include contact information for the provider can impede communication during the review process. Having accurate and accessible contact details ensures that any questions or clarifications can be addressed quickly, effectively minimizing delays.
By avoiding these common mistakes, individuals can enhance the efficiency of the UPMC Authorization Form submission process and facilitate better healthcare outcomes.
Documents used along the form
When submitting the UPMC Auth form for prior authorization of medication, several other forms and documents may be required to ensure a smooth approval process. Each of these documents plays a crucial role in providing necessary information and facilitating timely decisions by the health plan. Below is a list of commonly used forms that accompany the UPMC Auth form.
- Patient Consent Form: This document secures the patient's permission to share their medical information with the health plan. It ensures compliance with privacy regulations and is essential for processing claims or requests.
- Clinical Information Form: This detailed form collects comprehensive medical history and treatment information relevant to the authorization request. It may include past treatments, services provided, and diagnostic codes that pertain to the patient's condition.
- Prescription Drug Formulary: This resource outlines the medications covered under the patient's insurance plan, including preferred alternatives. It assists providers in proposing the most cost-effective options when submitting authorization requests.
- Medical Necessity Documentation: Additional notes or letters from the provider explaining why the requested medication is necessary can support the authorization request. This document often includes details about the patient's specific health needs.
- Treatment Plan: A structured outline detailing the patient's ongoing treatment course can be beneficial. This plan typically incorporates medication regimens, frequencies, and anticipated outcomes to clarify the need for the progression of therapy.
- Previous Drug Trials Documentation: This form captures information about any prior medications that have been tried, including dates, dosages, and effectiveness. It helps to substantiate the claim for the requested medication by showing the need for alternatives.
Having these documents prepared will help expedite the authorization process, minimizing delays and ensuring that patients receive the necessary medications in a timely manner. Each document adds value by providing pertinent information that supports the request, ultimately benefiting patient care.
Similar forms
The UPMC Auth form, primarily used for requesting prior authorization for specific medications, shares similarities with various other documents commonly used in healthcare settings. Each of these forms serves a unique purpose but reflects a focus on gathering essential patient information for approved treatment plans. Here is a list of six documents similar to the UPMC Auth form:
- Prior Authorization Forms: Like the UPMC Auth form, other prior authorization forms are used by insurers to determine if a prescribed treatment or medication requires additional approval. Examples include forms from Blue Cross Blue Shield and Aetna, which also ask for patient specifics and medical history related to the requested treatment.
- Medication Reconciliation Forms: These forms compile lists of all medications a patient is taking, similar to how the UPMC Auth form inquires about current and past medications. Accurate medication reconciliation is vital for ensuring patient safety and avoiding harmful drug interactions.
- Referral Forms: Referral forms request permission from a primary care physician to see a specialist. Much like the UPMC form, they require specific patient information and details related to the medical necessity for the referral.
- Prescription Drug Claim Forms: These forms are submitted to insurance companies to claim coverage for medications. They often require similar information, including patient details and medication specifics, paralleling the data collection seen in the UPMC Auth form.
- Patient Intake Forms: When new patients register at a healthcare facility, they complete intake forms that collect personal, medical, and insurance information. This is akin to the UPMC Auth form's focus on gathering detailed patient history for treatment evaluation.
- Appeal Forms for Denied Claims: These documents are used by patients or providers to contest denied medication claims. The appeal process often necessitates providing comprehensive medical history and treatment rationale, mirroring the documentation process outlined in the UPMC Auth form.
Each of these forms emphasizes the importance of detailed patient information and medical history, ensuring that healthcare providers can make informed decisions regarding treatment options and insurance coverage.
Dos and Don'ts
When filling out the UPMC Authorization form, there are several key actions to consider that can help streamline the process. Below is a list outlining what you should and should not do.
- Do: Complete all sections of the form. Ensure every part is filled out to avoid delays.
- Do: Include details of past medical treatments. Specific information about prior prescription treatments or side effects can support your request.
- Do: Verify the contact information for the provider. Accurate details will facilitate communication regarding the authorization process.
- Do: Indicate if the medication is ongoing or new. This distinction helps in processing and determining the necessary steps.
- Do: Review the form for completeness before submission. A thorough review can prevent issues later on.
- Don't: Leave any sections blank. Incomplete responses may lead to unnecessary delays.
- Don't: Forget to provide relevant medical history. Omitting this information can hinder your request's success.
- Don't: Use illegible handwriting. It's essential to type or print neatly to ensure clarity.
- Don't: Submit the form without obtaining necessary signatures. Ensure all required approvals are in place before sending.
- Don't: Assume generic substitutions are acceptable. Clearly indicate preference for brand or generic medications.
Misconceptions
Understanding the UPMC Auth Form can sometimes be challenging. Here are five common misconceptions and clarifications about this form:
- Form Completion Is Optional. Many believe that filling out the form completely is not necessary. In reality, incomplete responses may lead to delays in the authorization request process. It's essential to provide all requested information.
- Only New Medications Require Authorization. Some individuals think that prior authorization is only needed for new prescriptions. However, ongoing medications also require this process if specific criteria are met, or if there are changes in the patient's treatment plan.
- Submitting the Form Is Enough. Another misconception is that submitting the completed form guarantees approval. The UPMC team carefully reviews each request, and the necessity for using formulary alternatives must be clearly justified. Supporting documentation is crucial.
- Only Doctors Can Submit the Form. It's often assumed that only physicians are allowed to submit the form. While healthcare providers typically complete and submit the form, patients or their authorized representatives can also assist in this process.
- Talking to UPMC Is Not Necessary. Some think that if they submit the form, no further communication with UPMC is needed. In urgent situations, reaching out directly to UPMC Health Plan Pharmacy Services can expedite the process and provide clarity.
Recognizing these misconceptions can help streamline the prior authorization process and ensure that patients receive the medications they need in a timely manner.
Key takeaways
Urgent requests demand immediate action. If your request is urgent, reach out directly to UPMC Health Plan Pharmacy Services by phone instead of completing the form.
Accuracy matters. Fill out the form clearly and completely to avoid delays. Provide detailed information about past medical treatments.
Include essential medical history. Clearly list all previous medications and any side effects experienced. This helps substantiate your request for an exception.
Generic substitutions are standard. List your preference for brand versus generic drugs. If you want a specific brand, indicate that preference on the form.
Missing information can stall your process. Ensure all fields are filled out, especially regarding provider and patient details to facilitate approval.
Browse Other Templates
Michigan Liquor License Application - Responses on the form impact the regulatory status of the business being inspected.
Fairfax Water Tenant Authorization Form - Asking for assistance may be required if issues arise during submission.