Fill Out Your Us Script Prior Form
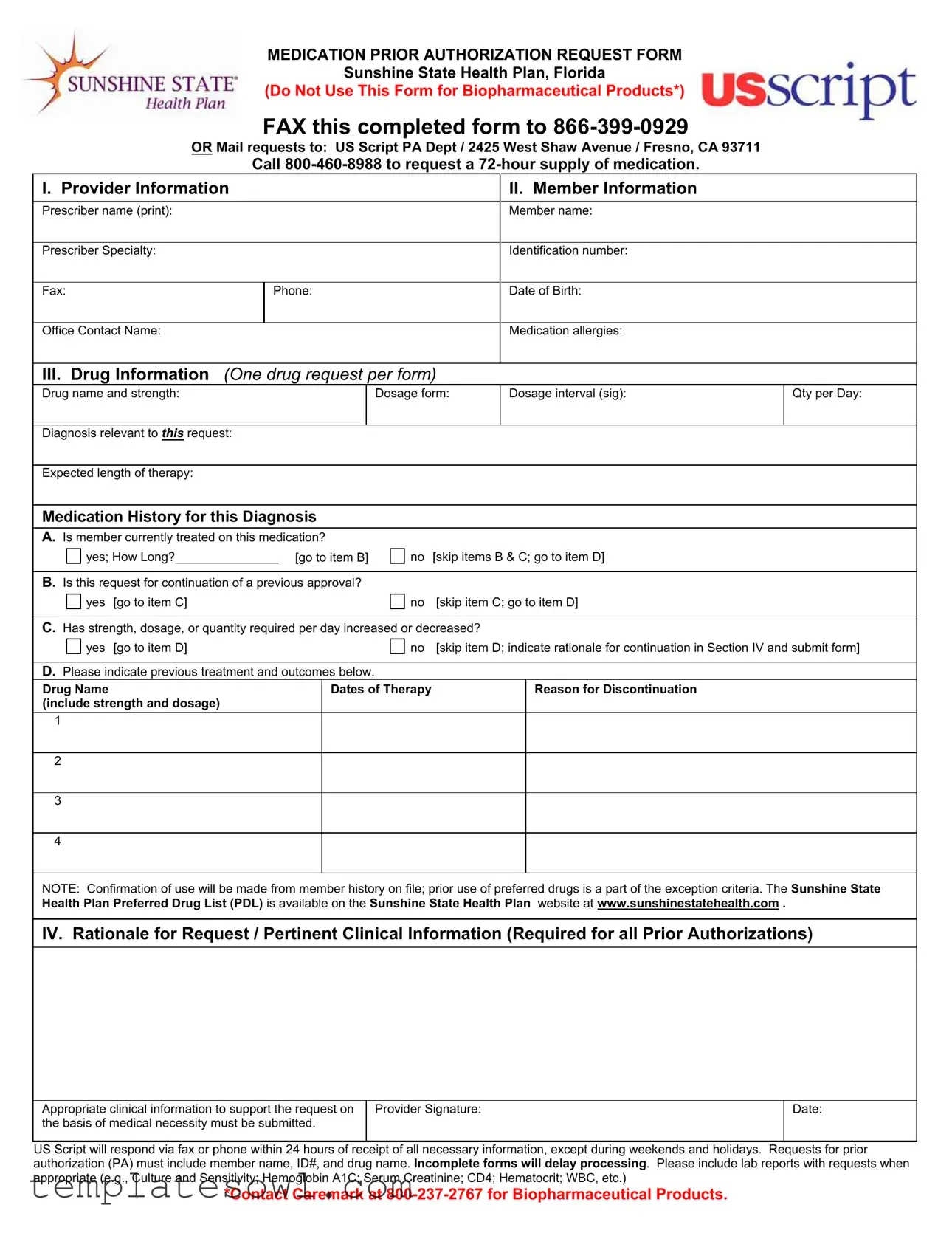
Navigating the healthcare landscape in the United States often involves understanding various forms and processes, one of which is the US Script Prior Authorization Request Form. This form is crucial for obtaining approval for certain medications under the Sunshine State Health Plan in Florida. Primarily, it serves as a structured means for healthcare providers to request authorization for prescription drugs that are not routinely covered. This form requires detailed information from both the provider and the member, including essential details such as the prescriber’s name, the member’s identification number, and specifics about the medication being requested. It also prompts the prescriber to elaborate on the patient’s medical history, including any previous treatments and their outcomes, ensuring that the request is well-supported by clinical information. When submitting the form, completeness is key; any missing information can lead to delays in processing. Healthcare providers must also provide a rationale for the request that clearly reflects the medical necessity of the medication, reinforcing the importance of thorough documentation. Not only does this form help streamline the approval process, but it also ensures that the patient's needs are carefully considered in alignment with the health plan's guidelines.
Us Script Prior Example
MEDICATION PRIOR AUTHORIZATION REQUEST FORM
Sunshine State Health Plan, Florida
(Do Not Use This Form for Biopharmaceutical Products*)
FAX this completed form to
OR Mail requests to: US Script PA Dept / 2425 West Shaw Avenue / Fresno, CA 93711
Call
I. Provider Information |
|
|
II. Member Information |
|
|||||
|
|
|
|
|
|
|
|
|
|
Prescriber name (print): |
|
|
Member name: |
|
|||||
|
|
|
|
|
|
|
|
|
|
Prescriber Specialty: |
|
|
Identification number: |
|
|||||
|
|
|
|
|
|
|
|
|
|
Fax: |
|
Phone: |
|
|
Date of Birth: |
|
|||
|
|
|
|
|
|
|
|
|
|
Office Contact Name: |
|
|
Medication allergies: |
|
|||||
|
|
|
|
|
|
||||
III. Drug Information (One drug request per form) |
|
|
|
||||||
Drug name and strength: |
|
Dosage form: |
Dosage interval (sig): |
Qty per Day: |
|||||
|
|
|
|
|
|
|
|
||
Diagnosis relevant to THIS request: |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|||
Expected length of therapy: |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|||
Medication History for this Diagnosis |
|
|
|
|
|
||||
A. Is member currently treated on this medication? |
|
|
|
|
|
||||
yes; How Long?_______________ [go to item B] |
no |
[skip items B & C; go to item D] |
|
||||||
|
|
|
|
|
|
|
|||
B. Is this request for continuation of a previous approval? |
|
|
|
|
|
||||
yes |
[go to item C] |
no |
[skip item C; go to item D] |
|
|||||
|
|
|
|
|
|||||
C. Has strength, dosage, or quantity required per day increased or decreased? |
|
|
|
||||||
yes |
[go to item D] |
no |
[skip item D; indicate rationale for continuation in Section IV and submit form] |
||||||
|
|
|
|
|
|
|
|||
D. Please indicate previous treatment and outcomes below. |
|
|
|
|
|
||||
Drug Name |
|
|
Dates of Therapy |
|
|
Reason for Discontinuation |
|
||
(include strength and dosage) |
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NOTE: Confirmation of use will be made from member history on file; prior use of preferred drugs is a part of the exception criteria. The Sunshine State Health Plan Preferred Drug List (PDL) is available on the Sunshine State Health Plan website at www.sunshinestatehealth.com .
IV. Rationale for Request / Pertinent Clinical Information (Required for all Prior Authorizations)
Appropriate clinical information to support the request on |
Provider Signature: |
Date: |
the basis of medical necessity must be submitted. |
|
|
|
|
|
US Script will respond via fax or phone within 24 hours of receipt of all necessary information, except during weekends and holidays. Requests for prior authorization (PA) must include member name, ID#, and drug name. Incomplete forms will delay processing. Please include lab reports with requests when appropriate (e.g., Culture and Sensitivity; Hemoglobin A1C; Serum Creatinine; CD4; Hematocrit; WBC, etc.)
*Contact Caremark at
Form Characteristics
| Fact Name | Description |
|---|---|
| Form Purpose | This form is used to request prior authorization for medications under the Sunshine State Health Plan in Florida, with specific instructions not to use it for biopharmaceutical products. |
| Submission Options | Completed forms can be faxed to 866-399-0929 or mailed to the US Script PA Department at 2425 West Shaw Avenue, Fresno, CA 93711. |
| Response Time | US Script aims to respond within 24 hours of receiving all necessary information, except during weekends and holidays. |
| Governing Laws | The use of this form is governed by Florida state laws related to healthcare and patient authorization. |
Guidelines on Utilizing Us Script Prior
Completing the US Script Prior Authorization Request Form is an important step in facilitating the approval process for a specific medication. The following steps outline how to accurately fill out the form to ensure prompt processing and response.
- Gather Required Information: Before beginning, ensure you have all necessary information regarding the prescriber, member, and medication.
- Provider Information: In the first section, clearly print the prescriber’s name, specialty, fax number, phone number, office contact name, and medication allergies.
- Member Information: Fill in the member's name and date of birth, along with their identification number.
- Drug Information: Specify the drug name and strength, dosage form, dosage interval, and quantity per day. Make sure to indicate the diagnosis related to this request and the expected length of therapy.
- Medication History: Answer questions A through D based on the member’s medical history. If the member is currently treated with the medication, provide the duration of treatment. If not, skip to item D. If this request is for continuation, confirm any changes in strength, dosage, or quantity for item C. In item D, list any previous treatments along with their outcomes including any reasons for discontinuation.
- Rationale for Request: In the final section, outline pertinent clinical information that supports the request. This should include necessary details that demonstrate medical necessity.
- Provider Signature: Sign and date the form to validate the request.
- Submit the Form: Send the completed form via fax to 866-399-0929 or mail it to US Script PA Dept, 2425 West Shaw Avenue, Fresno, CA 93711.
Once submitted, expect a response from US Script within 24 hours if all required information is provided. Be prepared to provide additional documentation, such as lab reports, if requested. Ensuring thoroughness and accuracy will help in expediting the review process.
What You Should Know About This Form
What is the purpose of the US Script Prior Authorization Request Form?
The US Script Prior Authorization Request Form is used to obtain approval for specific medications before they can be dispensed. This ensures that the requested drug is medically necessary for the member, and it helps manage costs and promote the use of preferred drugs.
Which medications require this form?
This form is required for medications that are not biopharmaceutical products. Biopharmaceutical products need to be handled through a different process. Always check with your healthcare provider if you are unsure.
How should I submit the completed form?
You can submit the completed form by faxing it to 866-399-0929. Alternatively, you can mail it to: US Script PA Dept / 2425 West Shaw Avenue / Fresno, CA 93711. Ensure that you submit it to the correct address to avoid delays.
What information is necessary for the form to be processed?
Important information includes the prescriber’s name, member’s name, medication details, diagnosis, and pertinent medical history. Missing details may delay the processing of your request. Include lab reports when relevant.
What happens if I submit an incomplete form?
Submitting an incomplete form will lead to delays in processing your authorization request. It is crucial to double-check all fields for accuracy before sending it in.
What if I need a medication urgently?
If you need a 72-hour supply of medication urgently, you can call 800-460-8988 for assistance. Make sure to explain your situation clearly for a prompt response.
How quickly will I receive a response after submitting my request?
You should receive a response from US Script within 24 hours of receipt of all necessary information. Please note that responses may be delayed during weekends and holidays.
What additional documentation should I provide with the request?
Alongside the completed form, it is highly recommended to provide supporting clinical information such as lab reports. This documents the medical necessity of the requested medication and may aid in swift processing.
Where can I find the Sunshine State Health Plan Preferred Drug List?
The Preferred Drug List (PDL) is available on the Sunshine State Health Plan website at www.sunshinestatehealth.com. Consult this resource to identify preferred medications that may streamline your approval process.
Common mistakes
Submitting the US Script Prior Authorization Request Form can be a straightforward process, but mistakes can easily lead to delays or complications. One common mistake is not providing complete provider information. This includes the prescriber’s name, specialty, fax number, and phone number. Omitting this crucial information can cause unnecessary back-and-forth communication, which might extend the approval process.
Another frequent error is failing to fill out the member information section accurately. Members must ensure that the identification number and date of birth are correct. Incorrect details can lead to confusion and potentially result in the denial of the request.
When it comes to the drug information section, many individuals mistakenly attempt to request more than one drug on a single form. It is essential to remember that each drug request requires a separate form. Consolidating requests leads to incomplete submissions and will only cause delay.
In the drug information section, being vague about dosage and quantity can also lead to issues. The form requires specific details such as drug name, strength, and dosage interval. Providing imprecise information can result in the request being deemed invalid, requiring another submission.
Some people forget to include a critical part of the form, known as the rationale for request. This section is mandatory, as it provides the clinical justification for the medication. Incomplete rationales can lead to immediate rejection, causing frustration for both providers and members.
Another frequent oversight involves the medication history for the diagnosis. Failing to answer all the relevant questions about previous treatment and current medication can hinder the assessment of the request. If a member has not previously been treated with the proposed medication, skipping sections can leave the reviewer without essential context.
Additionally, not submitting supporting documentation such as lab reports can be a significant error. For many requests, healthcare providers need to attach relevant medical records to strengthen the argument for medical necessity. Without these documents, the request may face prolonged scrutiny or outright denial.
People also often misinterpret the priority timeframe for response. Assuming that any delay signals the denial of the request can create unnecessary anxiety. The standard response time is typically 24 hours after receipt of all necessary details, excluding weekends and holidays.
Lastly, some forget to print and sign the form. A missing signature can halt the entire process. Double-checking all sections of the form before submission is a prudent step that helps ensure everything is complete.
Documents used along the form
In the realm of healthcare, various forms and documents work together to ensure that patients receive the medications they need. Among these, the US Script Prior Authorization Form is crucial for obtaining approval for certain medications before they can be dispensed. Below is a list of other commonly used forms that often accompany the Prior Authorization process. Each of these documents serves a specific purpose in facilitating communication between healthcare providers, insurance companies, and patients.
- Medication Prescription Form: This document is used by healthcare providers to formally prescribe medication to a patient. It includes details such as the medication name, dosage, and instructions for use.
- Patient Registration Form: New patients complete this form to provide their personal information, insurance details, and medical history, enabling healthcare providers to deliver personalized care.
- Medication Administration Record (MAR): A vital tool for healthcare professionals, this document tracks medication administration to a patient, documenting dosages, times, and any reactions the patient may have.
- Claim Submission Form: After services are rendered, this form is filed with insurance providers to seek reimbursement for healthcare expenses, ensuring providers are compensated for their services.
- Appeal Letter Template: In instances where prior authorization is denied, this template helps patients or providers formally request a review of the decision by the insurance company.
- Clinical Notes: Written by healthcare providers, these notes summarize a patient’s medical consultations, treatment plans, and progress, offering context for prior authorization requests.
- Authorization for Release of Information: This form gives healthcare providers the permission to share a patient’s medical information with insurers or other relevant parties, facilitating the approval process.
- Referral Form: When a patient needs to see a specialist, this form is completed by the referring provider, ensuring the specialist has the necessary information to provide appropriate care.
- Insurance Verification Form: Used by healthcare providers to confirm a patient’s insurance coverage, this form helps determine what services and medications will be covered, streamlining the prior authorization process.
Understanding these accompanying forms can enhance the experience of both healthcare providers and patients. Each document plays a pivotal role in ensuring that medication management is efficient, well-documented, and aligned with patients' healthcare needs. Navigating this paperwork can initially seem daunting, but it ultimately serves to protect and prioritize the well-being of patients.
Similar forms
The US Script Prior Authorization Request Form shares similarities with several other important documents used in healthcare and insurance contexts. These documents serve various functions, often related to the approval of medication or treatment plans. Below are nine documents that resemble the US Script form in their purpose and structure:
- Medicare Prior Authorization Form: This form is pivotal for Medicare beneficiaries seeking approval for certain medical services or medications. Like the US Script form, it requires detailed provider and patient information, including specific diagnoses and treatment history.
- Medicaid Prior Authorization Request: Similar to the Medicare form, the Medicaid prior authorization request is essential for Medicaid members. It too requires comprehensive clinical information and justification for requested treatments, paralleling the structured approach of the US Script form.
- Commercial Insurance Prior Authorization Form: Many private insurers require this document to manage coverage for specific drugs or procedures. It shares a format that includes sections for patient history, treatment rationale, and healthcare provider details, mirroring the US Script form’s organization.
- Medication Request Form: This internal document often used by healthcare facilities facilitates requests for medications. It typically captures similar patient and medication details, enabling efficient communication across pharmacy and medical departments.
- Case Management Request Form: Utilized by case managers to initiate service requests, this form integrates patient information, treatment history, and clinical justification. Its structured layout and focus on patient care align closely with the components found in the US Script form.
- Clinical Trial Enrollment Form: This form governs participation in clinical trials, requiring medical history and treatment rationale. Its comprehensive nature and emphasis on patient preparedness echo the thoroughness seen in the US Script prior authorization documentation.
- Drug Utilization Review Form: Often required for evaluating the appropriateness of prescribed medication, this form calls for patient-specific data and clinical details. The focus on drug therapy and patient outcomes resembles the information sought by the US Script form.
- Specialty Pharmacy Authorization Form: Used when patients need medications that require special handling, this form collects relevant medical information and justification. It also underscores medical necessity, paralleling the goals of the US Script prior authorization.
- Formulary Exception Request: This document requests an exception to a health plan's formulary, outlining why a certain drug is necessary. Similar to the US Script form, it demands detailed justifications and patient information to support the request.
Each of these documents has a unique focus and purpose but shares a common goal: ensuring patients receive the medically necessary treatments and medications while facilitating clear communication between healthcare providers and insurers.
Dos and Don'ts
When filling out the US Script Prior Authorization form, there are essential guidelines to follow. The following list outlines actions to take and avoid to ensure a smooth submission process.
- Do: Provide complete and accurate information.
- Do: Include the member's ID number and drug name.
- Do: Attach relevant lab reports when necessary.
- Do: Fax the completed form to 866-399-0929 or mail it to the designated address.
- Do: Check for medication allergies before submitting the form.
- Don't: Skip any required sections of the form.
- Don't: Use the form for biopharmaceutical products.
Following these guidelines can help facilitate the approval process and avoid delays in medication access.
Misconceptions
Many individuals have misconceptions regarding the US Script Prior Authorization Request Form. Understanding these misconceptions is essential for both healthcare providers and patients to navigate the process effectively. Below are some common misunderstandings along with clarifications.
- This form is used for all medications. The US Script Prior Authorization Request Form is specifically designed for medications that require prior authorization, excluding biopharmaceutical products. Using this form for other types of medications can result in delays.
- Submitting the form guarantees approval. While submitting the form is a necessary step, approval depends on various factors including medical necessity and the patient's history. There is no guarantee of approval upon submission.
- Any provider can submit the form. Only authorized prescribers, typically physicians or specialists, can complete and submit this form. This ensures that the request is valid and backed by the appropriate clinical rationale.
- All required information is optional. Providing complete and accurate information is crucial. Incomplete forms will delay processing and may lead to denial of the request.
- Prior authorization is only needed for new medications. This form is also applicable when requesting a continuation of previously approved medications. If there are changes in strength or dosage, it must be clearly noted.
- The response time is always within 24 hours. Although US Script aims to respond within 24 hours, response times can be longer during weekends, holidays, or if the submission is incomplete.
- Lab reports are never required. Although not always necessary, including relevant lab reports can significantly support the request and provide essential context for the medication's necessity.
- Faxing the form is the only option for submission. While faxing is one method, submitting the form via mail is also acceptable. Ensure the form is sent to the correct address for timely processing.
Clarifying these points may help streamline the prior authorization process and enhance patient care. It is vital for providers and patients alike to stay informed about the requirements and protocols associated with this form.
Key takeaways
Filling out and utilizing the US Script Prior Authorization Request Form requires attention to several key details. The following takeaways provide a comprehensive understanding of the process.
- Purpose of the Form: This form is specifically designed for requesting prior authorization for medications within the Sunshine State Health Plan.
- Submit via Fax or Mail: Completed forms can be faxed to 866-399-0929 or mailed to US Script PA Dept, 2425 West Shaw Avenue, Fresno, CA 93711.
- Emergency Supply: Call 800-460-8988 to request a 72-hour supply of medication if immediate access is necessary.
- Provider Information: Accurate information regarding the prescriber, including name, specialty, and contact details, is essential for effective processing.
- Member Information: Details about the member, such as name, date of birth, and identification number, must be clearly indicated.
- Use One Drug Per Form: Each form should request prior authorization for one drug only, ensuring focused information is provided.
- Medication History: The form inquires about the member's current treatment status and previous medication history. This information is crucial for evaluating the request.
- Rationale for Request: A clear explanation regarding the medical necessity of the requested medication must be documented in Section IV.
- Timely Response: US Script will respond within 24 hours of receiving all necessary information, excluding weekends and holidays.
- Preferred Drug List (PDL): The Sunshine State Health Plan's Preferred Drug List can be accessed online, which may affect the approval process.
Adhering to these guidelines will facilitate efficient processing of requests for medication prior authorizations.
Browse Other Templates
Judicial Council Forms - A judicial subpoena ensures that necessary evidence is available for the court to make informed decisions.
What Documents Are Needed for Citizenship - Applicants aged 75 and older are exempt from the biometric services fee.
Why Do Employers Ask About Disability - The form helps identify areas where additional outreach may be needed.