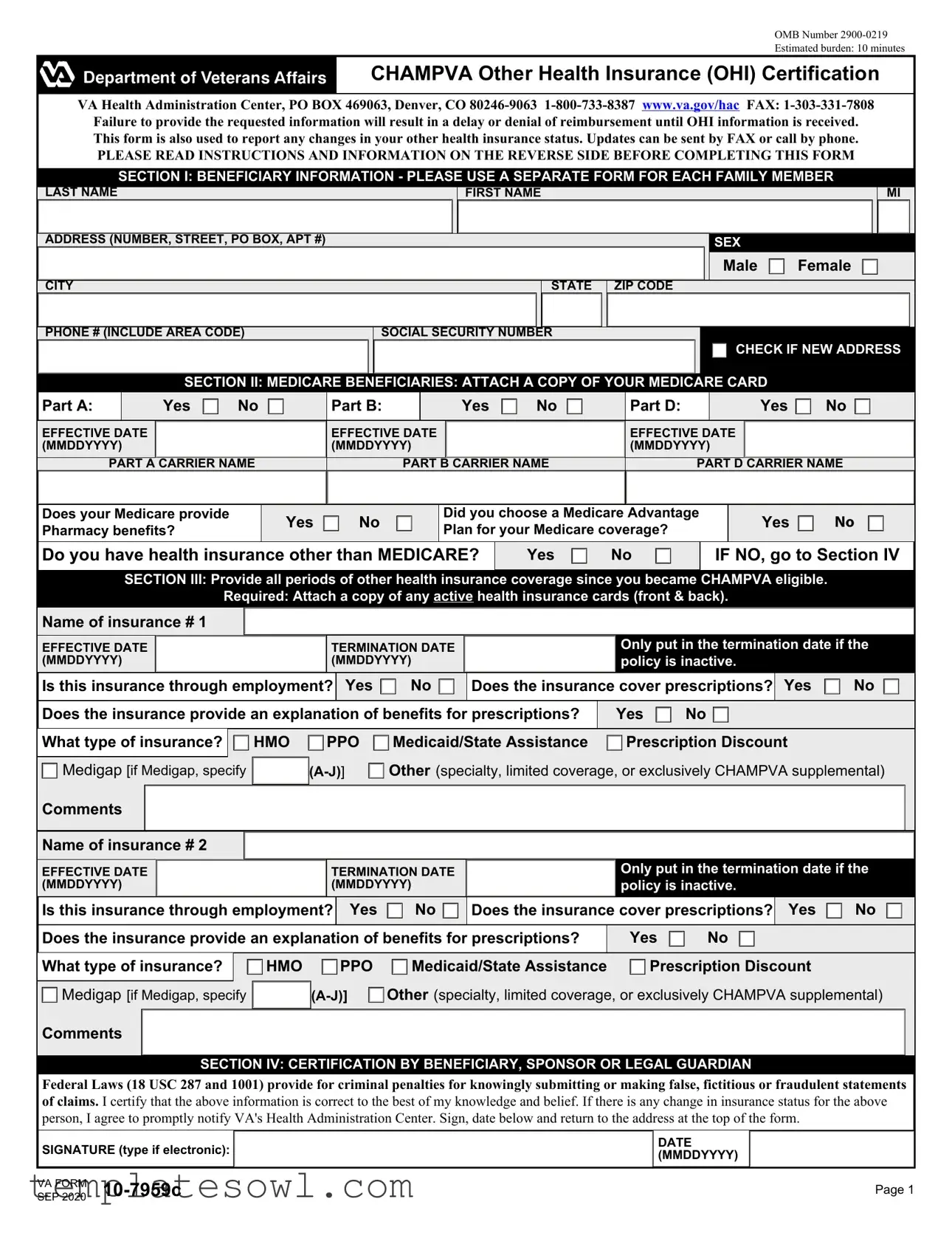
Fill Out Your Va 10 7959C Form
The VA Form 10-7959C is a critical document for veterans and their family members enrolled in the CHAMPVA program, ensuring that they can efficiently manage their health care benefits. This form is primarily designed to report the status of any Other Health Insurance (OHI) that a beneficiary may have. Proper completion of the form is essential, as it directly impacts reimbursement for medical expenses. Relying on this form, users can communicate any changes to their health insurance coverage, submit necessary information for re-certification, and ensure they provide comprehensive details about their Medicare coverage as well. To avoid potential delays or denials in benefits, beneficiaries must furnish complete and accurate information regarding their insurance status. This includes periods of coverage, carrier details, and prescription benefits. The form also emphasizes the importance of submitting supporting documentation, such as copies of insurance cards and explanation of benefits (EOB) statements, which are crucial for processing claims. Understanding the requirements and properly utilizing the form can significantly ease the navigation of CHAMPVA benefits, providing peace of mind to those who have served the country.
Va 10 7959C Example
OMB Number
Estimated burden: 10 minutes
CHAMPVA Other Health Insurance (OHI) Certification
VA Health Administration Center, PO BOX 469063, Denver, CO
PLEASE READ INSTRUCTIONS AND INFORMATION ON THE REVERSE SIDE BEFORE COMPLETING THIS FORM
SECTION I: BENEFICIARY INFORMATION - PLEASE USE A SEPARATE FORM FOR EACH FAMILY MEMBER
LAST NAME
FIRST NAME
MI
ADDRESS (NUMBER, STREET, PO BOX, APT #)
SEX
Male  Female
Female 
CITY |
STATE ZIP CODE |
PHONE # (INCLUDE AREA CODE) |
SOCIAL SECURITY NUMBER |
|
CHECK IF NEW ADDRESS |
SECTION II: MEDICARE BENEFICIARIES: ATTACH A COPY OF YOUR MEDICARE CARD
Part A: |
|
Yes |
|
No |
|
|
Part B: |
|
Yes |
|
No |
|
|
Part D: |
|
Yes |
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EFFECTIVE DATE |
|
|
|
|
|
EFFECTIVE DATE |
|
|
|
|
|
EFFECTIVE DATE |
|
|
|
|
|
|||
(MMDDYYYY) |
|
|
|
|
|
(MMDDYYYY) |
|
|
|
|
|
(MMDDYYYY) |
|
|
|
|
|
|||
|
|
|
|
|
|
|||||||||||||||
PART A CARRIER NAME |
PART B CARRIER NAME |
PART D CARRIER NAME |
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Does your Medicare provide Pharmacy benefits?
Yes  No
No
Did you choose a Medicare Advantage Plan for your Medicare coverage?
Yes  NO
NO
Do you have health insurance other than MEDICARE?
Yes  No
No
IF NO, go to Section IV
SECTION III: Provide all periods of other health insurance coverage since you became CHAMPVA eligible.
Required: Attach a copy of any active health insurance cards (front & back).
Name of insurance # 1
|
EFFECTIVE DATE |
|
|
|
TERMINATION DATE |
|
|
|
Only put in the termination date if the |
|
||||||||||||||||||||||||
|
(MMDDYYYY) |
|
|
|
(MMDDYYYY) |
|
|
|
policy is inactive. |
|
|
|
|
|
|
|||||||||||||||||||
|
Is this insurance through employment? |
Yes |
|
|
|
No |
|
|
Does the insurance cover prescriptions? |
Yes |
|
No |
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Does the insurance provide an explanation of benefits for prescriptions? |
|
|
Yes |
|
No |
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What type of insurance? |
|
|
HMO |
|
PPO |
|
|
|
Medicaid/State Assistance |
|
|
Prescription Discount |
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medigap [if Medigap, specify |
|
|
|
Other (specialty, limited coverage, or exclusively CHAMPVA supplemental) |
|
|||||||||||||||||||||||||||
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Comments |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Name of insurance # 2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EFFECTIVE DATE (MMDDYYYY)
TERMINATION DATE (MMDDYYYY)
Only put in the termination date if the policy is inactive.
|
Is this insurance through employment? |
Yes |
|
|
|
No |
|
|
Does the insurance cover prescriptions? |
Yes |
|
No |
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Does the insurance provide an explanation of benefits for prescriptions? |
|
Yes |
|
No |
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What type of insurance? |
|
|
|
HMO |
|
PPO |
|
|
|
Medicaid/State Assistance |
|
Prescription Discount |
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medigap [if Medigap, specify |
|
|
|
|
Other (specialty, limited coverage, or exclusively CHAMPVA supplemental) |
||||||||||||||||||||||
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Comments
SECTION IV: CERTIFICATION BY BENEFICIARY, SPONSOR OR LEGAL GUARDIAN
Federal Laws (18 USC 287 and 1001) provide for criminal penalties for knowingly submitting or making false, fictitious or fraudulent statements of claims. I certify that the above information is correct to the best of my knowledge and belief. If there is any change in insurance status for the above person, I agree to promptly notify VA's Health Administration Center. Sign, date below and return to the address at the top of the form.
SIGNATURE (type if electronic):
VA FORM
SEP 2020
DATE (MMDDYYYY)
Page 1
CHAMPVA OTHER HEALTH INSURANCE (OHI) CERTIFICATION
NOTES, DEFINITIONS, AND INSTRUCTIONS
INSTRUCTIONS
Failure to complete all applicable sections on the front can result in a delay or denial of benefits. Use this form to report any changes in your other health insurance.
•New beneficiaries - we need OHI information from the date your CHAMPVA eligibility became effective.
•
•To specify a medicare supplement plan A - J, refer to your policy cover sheet or your insurance membership card.
•If there are additional policies use plain bond paper and either type or legibly print your name, SSN, and the information for each item. Attach to this form. If submitting this form electronically add an attachment to the submission.
ITEMS TO RETURN WITH THIS COMPLETED OTHER HEALTH INSURANCE (OHI) CERTIFICATION
•A COPY of your Medicare card (do NOT send the original)
•A COPY of your other health insurance (OHI) member ID card (front and back).
•If your OHI does not issue EOBs, then attach a copy (card or document) of your schedule of benefits that lists your
DEFINITIONS
OHI: OHI refers to insurance or benefits you may have other than CHAMPVA called “Other Health Insurance”.
EOB: The abbreviation for an “explanation of benefits” form or letter that must accompany claims submitted to CHAMPVA. An EOB is a statement or “Remittance Advice” from an insurance carrier or benefit program that summarizes the action taken on a claim.
Note: If you have OHI primary to CHAMPVA you must submit EOB's for each primary insurance along with health care claims. If your OHI does not issue EOB's i.e. some HMO's and PPO's, you must submit a copy of your active
Carrier: Carrier is the insurance company that provides your medical benefits.
OHI primary to CHAMPVA: CHAMPVA by law is always supplemental or the secondary payer of health care benefits except for Medicaid, State Victims of Crimes Compensation Programs, and policies purchased exclusively to supplement CHAMPVA benefits.
Supplemental CHAMPVA policies: These are policies specifically purchased for the purpose of covering your cost share after CHAMPVA has completed adjudication of a claim.
Medicare supplemental policies: These are policies that are specifically for the purpose of covering your Medicare out of pocket expenses. These Medicare supplemental policies such as “Medigap” or Policies offered through employment are primary to CHAMPVA and must provide an EOB along with the Medicare EOB (two EOBs) for each claim submitted to CHAMPVA.
Indemnity: Plans that pay a flat fee or daily rate to supplement lost income while hospitalized are called Indemnity Plans.
Termination date: This is the date the policy ended or ceased to be active. The end date for a period shown on a card that will be reissued is not the termination date. Closing a policy will generate a true termination date.
Privacy Act Information: The authority for collection of the requested information on this form is 38 USC 501 and 1781. The purpose of collecting this information is to determine payer status when other health insurance coverage exists. The information you provide may be verified by a computer matching program at any time. You are requested to provide your Social Security number as your VA record is filed and retrieved by this number. You do not have to provide the requested information on this form but if any or all of the requested information is not provided, it may delay or result in denial of your request for CHAMPVA benefits. Failure to furnish the requested information will have no adverse impact on any other VA benefit to which you may be entitled. The responses you submit are considered confidential and may be disclosed outside VA only if the disclosure is authorized under the Privacy Act, including the routine uses identified in the VA system of records number 54VA16, titled "Health Administration Center Civilian Health and Medical Program Records
Paperwork Reduction Act: This information collection is in accordance with the clearance requirements of Section 3507 of the Paperwork Reduction Act of 1995. Public reporting burden for this collection of information is estimated to average 10 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. Comments regarding this burden estimate or any other aspect of this collection, including suggestions for reducing the burden, may be addressed by calling the CHAMPVA Help Line,
VA FORM |
Page 2 |
Form Characteristics
| Fact Name | Description |
|---|---|
| OMB Number | The OMB Number for this form is 2900-0219. |
| Estimated Burden | Completing the form generally takes about 10 minutes. |
| Purpose | This form certifies other health insurance (OHI) coverage for CHAMPVA beneficiaries. |
| Submission Address | Send completed forms to VA Health Administration Center, PO BOX 469063, Denver, CO 80246-9063. |
| Contact Method | You can contact the center via phone at 1-800-733-8387 or by fax at 1-303-331-7808. |
| Form Use | Use this form to report any changes in OHI status and provide updates as necessary. |
| Legal Consequences | Submitting false information may lead to criminal penalties under federal law (18 USC 287 and 1001). |
Guidelines on Utilizing Va 10 7959C
Filling out the VA Form 10-7959C is an important step for individuals eligible for CHAMPVA seeking reimbursement or reporting changes in their other health insurance (OHI) status. It's essential to provide accurate and complete information to avoid any delays or denials in benefits. Here are the steps to effectively fill out the form.
- Locate the VA Form 10-7959C, which can be found online or requested from the VA.
- In Section I, provide the beneficiary’s information:
- Write the last name, first name, and middle initial (if applicable).
- Fill in the complete address, including city, state, and ZIP code.
- Select the appropriate sex (Male or Female).
- Include a valid phone number with area code.
- Input the Social Security number of the beneficiary.
- If there is a new address, check the box.
- In Section II, for Medicare beneficiaries, provide the following:
- Attach a copy of your Medicare card (not the original).
- Indicate whether you have Medicare Part A, B, or D by circling Yes or No.
- Enter the effective dates for each Medicare part (MMDDYYYY).
- Provide the names of the carriers for each Medicare part.
- Indicate whether your Medicare provides pharmacy benefits.
- Specify if you chose a Medicare Advantage Plan.
- Next, in Section III, provide details about other health insurance:
- List each insurance policy you hold since becoming CHAMPVA eligible.
- Include the effective and termination dates of your policies in the specified format.
- Indicate if each policy is through employment.
- Answer whether the insurance covers prescriptions and if it provides explanations of benefits for prescriptions.
- Identify the type of insurance (HMO, PPO, etc.) and share comments as necessary.
- In Section IV, certify your information:
- Sign and date the form, confirming that the information provided is accurate.
- If submitting electronically, type your signature.
- Gather required attachments:
- A copy of your Medicare card.
- A copy of your other health insurance member ID card (front and back).
- If applicable, an explanation of benefits (EOB) or a schedule of benefits document from your other insurance.
- Submit the completed form and attachments to the VA Health Administration Center at the address provided at the top of the form.
After submission, monitor for any communication from the VA regarding your application. This helps ensure you adhere to any follow-up requirements, optimizing your benefits under the CHAMPVA program.
What You Should Know About This Form
What is the VA Form 10-7959C used for?
The VA Form 10-7959C, also known as the CHAMPVA Other Health Insurance (OHI) Certification, is primarily used to inform the Department of Veterans Affairs (VA) about your other health insurance coverage. Completing this form is essential if you are a beneficiary of the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA). It provides the necessary information to ensure that your claims are processed correctly and that you receive the appropriate reimbursements. Additionally, you are required to report any changes to your health insurance status using this form.
How long does it take to complete the VA Form 10-7959C?
On average, completing the VA Form 10-7959C takes approximately 10 minutes. Though this may vary depending on your familiarity with your other health insurance details, it's designed to be straightforward and efficient. To facilitate the process, gather your insurance information beforehand, such as policy numbers and effective dates.
What happens if I don't provide the required information on the form?
Failure to provide the necessary information can lead to significant consequences. Delays or denials in reimbursement may occur if the VA does not have accurate details regarding your other health insurance. The VA relies on this information to process your claims and determine how to coordinate benefits. Therefore, it's crucial to complete all sections of the form to avoid these issues.
Do I need to submit supporting documents along with the form?
Yes, submitting supporting documents is essential. When completing the VA Form 10-7959C, you must include copies of your Medicare card and your other health insurance member ID card (both front and back). If your other health insurance provider does not issue explanation of benefits (EOBs), include any documents that detail your copayment schedule. Providing these documents helps the VA verify your coverage and facilitates quicker processing of your claims.
Can I report changes to my other health insurance by phone or fax?
Absolutely! If there are any changes to your health insurance status, you can report these updates either by calling the VA's Health Administration Center at 1-800-733-8387 or by sending the updated information via fax at 1-303-331-7808. It is essential to keep your information current so that the VA maintains accurate records and can effectively coordinate your benefits.
What should I do if I become a new CHAMPVA beneficiary?
If you have recently become a new CHAMPVA beneficiary, you will need to complete the VA Form 10-7959C to provide information regarding your other health insurance from the date you became eligible for CHAMPVA benefits. Ensure you supply all requested details accurately, including attaching the necessary supporting documents. This step is vital in establishing your enrollment in the program and ensuring you receive the benefits you are entitled to.
Common mistakes
Filling out the VA Form 10-7959C can be straightforward, yet several common errors may impede the processing of benefits. Understanding these pitfalls can enable beneficiaries to navigate the application process more efficiently.
One frequent mistake occurs when individuals fail to complete all applicable sections of the form. The instructions explicitly state that incomplete submissions may lead to delays or outright denials of reimbursement. For instance, if a beneficiary skips providing their Social Security number, the Veterans Affairs (VA) may be unable to verify the individual’s identity, thus complicating the approval process.
Inaccurate dates often cause confusion as well. For example, when filling out effective or termination dates for insurance coverage, beneficiaries must follow the required format—MMDDYYYY. An incorrect format will not only lead to denial but may also require the individual to resubmit the form, fortifying an already prolonged timeline for benefits.
Another oversight involves omitting requisite documentation. Beneficiaries must attach copies of their health insurance cards and Medicare cards. Failing to provide these documents can lead to significant delays in processing claims. The VA’s requirement for both sides of the insurance card should not be overlooked, as it serves to authenticate the coverage claimed.
Some individuals neglect to specify whether their insurance is through employment or if it covers prescriptions. Each of these questions plays a crucial role in assessing the coverage provided by different policies. Misrepresentation or lack of clarity on these points can lead to misunderstandings regarding benefits eligibility.
Moreover, beneficiaries frequently disregard the necessity of reporting changes in their OHI status promptly. If there are adjustments in healthcare coverage, the VA should be informed immediately. Failure to report such changes could hinder claims processing and result in unintended payment gaps.
Finally, submitting the form with an electronic signature rather than a wet signature can be another stumbling block. While electronic submissions are permissible, specific instructions must be followed meticulously. If the process is not correctly adhered to, it may result in backtracking, thus wasting valuable time.
In conclusion, by carefully reviewing and adhering to the instructions while filling out the VA Form 10-7959C, beneficiaries can avoid common pitfalls. Ensuring that all necessary information is submitted accurately and completely is key to a smoother experience when seeking reimbursement through CHAMPVA.
Documents used along the form
When working with the VA Form 10-7959C, several other forms and documents may be required or beneficial for comprehensive health care management. Each document plays a role in ensuring smooth navigation of health insurance requirements and claims processes. Here's a list of these pertinent documents.
- VA Form 10-10EZ: This is the application for health benefits. It assesses eligibility for VA health care services and must be completed by new applicants or those reapplying.
- VA Form 21-526EZ: This is the application for disability compensation and related benefits. It provides necessary details regarding service-connected disabilities and allows veterans to seek additional support.
- Medicare Card: A copy of the Medicare card is crucial. It ensures that the patients' Medicare benefits are verified and properly processed in conjunction with CHAMPVA.
- Other Health Insurance Policy Documents: Copies of OHI member ID cards should include both front and back. They are needed to confirm coverage details and facilitate reimbursements.
- Claim for Compensation (VA Form 21-535): This form is used to claim burial benefits and is essential for beneficiaries who seek funding for funeral expenses.
- Explanation of Benefits (EOB): This document, received from OHI providers, provides details on claim outcomes and is required when submitting claims for reimbursement from CHAMPVA.
- VA Form 10-579: The Application for CHAMPVA Benefits form allows certain family members of disabled or deceased veterans to apply for eligibility under the CHAMPVA program.
- VA Form 10-0346: This form is necessary for requesting the review of CHAMPVA claims. It helps beneficiaries contest claim decisions or seek adjustments.
- Medicare Supplement Policy Information: Documentation outlining benefits and coverage provided by Medicare supplemental insurance plans. It is essential for understanding what additional costs may be available for CHAMPVA beneficiaries.
Each of these documents is vital for ensuring that benefits are administered correctly and efficiently. They help to clarify coverage options, streamline claims, and maintain essential health insurance relationships. If you are filing for benefits or responding to insurance requests, having all necessary forms completed and available will expedite the process significantly.
Similar forms
VA Form 10-10EZ: This application form is used for health benefits enrollment for veterans. Like the VA 10-7959C, it collects essential insurance and health information to determine eligibility and benefits.
VA Form 21-526EZ: This form is used to apply for disability compensation. Similar to the 10-7959C, it requires personal information and supports the administration of related benefits.
VA Form 21-4502: This is an application for veteran’s mortgage benefits. It, too, must provide detailed information about the veteran’s other insurance and financial situation, paralleling the OHI requirements of the 10-7959C.
VA Form 10-583: Used for claiming reimbursement for travel expenses, this form also requires detailed insurance and payment information, making it similar in function to the 10-7959C.
Medicare Form CMS-1500: This form is for billing Medicare for services provided. It requires insurance information like the 10-7959C to process claims effectively.
Medicaid Application Form: This form assesses eligibility for Medicaid benefits. Both it and the 10-7959C require detailed health insurance coverage information to determine eligibility.
CHAMPVA Application Form: This application is for enrolling in the CHAMPVA program for dependents of veterans. It is similar to the 10-7959C as it requires the same type of insurance information to qualify.
Long-Term Care Insurance Application: This form is necessary for enrolling in long-term care insurance plans, which also necessitate detailed personal and insurance information akin to that in the 10-7959C.
Insurance Claim Form (UB-04): Used to submit claims for hospital services, this form requires comprehensive insurance information for processing, akin to the requirements of the 10-7959C.
Life Insurance Application: This document collects information to assess risk and eligibility for life insurance policies, similar to the way the 10-7959C collects health insurance information.
Dos and Don'ts
When completing the VA Form 10-7959C, it's essential to ensure accuracy and completeness to avoid any delays or denials in reimbursement. Below are important guidelines to follow:
- DO read all instructions carefully before starting the form.
- DO provide accurate information for each family member on a separate form.
- DO attach copies of all relevant health insurance cards, both the front and back.
- DO report any changes in health insurance immediately to prevent reimbursement delays.
- DON'T leave any section blank if it applies to you; this can lead to processing issues.
- DON'T submit the original Medicare card; only provide a copy.
- DON'T forget to sign and date the form before submitting it.
- DON'T delay in providing the form; timely submission is critical for proper handling.
Following these guidelines will streamline your application process and ensure timely access to your benefits.
Misconceptions
Myths surrounding the VA Form 10-7959C can lead to confusion and mismanagement of health insurance reporting. Here are five common misconceptions:
- This form is only for new applicants. Many believe the 10-7959C is solely for new beneficiaries. In reality, it is also used for existing beneficiaries to report any changes in their other health insurance coverage.
- Filling out the form is optional. Some think that submitting this form is not necessary. However, failure to provide the requested information can delay or deny reimbursement. It is crucial to complete it whenever there are updates to your health insurance status.
- Medicare coverage is not relevant. There is a misconception that Medicare coverage does not affect CHAMPVA benefits. On the contrary, Medicare primary coverage significantly influences how claims are processed under CHAMPVA.
- Only the beneficiary needs to sign the form. A common misunderstanding is that only the beneficiary should sign the document. In fact, the form can also be signed by the sponsor or a legal guardian when applicable.
- All relevant information can be provided verbally. Some individuals believe they can relay their insurance information verbally instead of filling out the form. The VA requires written documentation to ensure accurate processing of claims.
Understanding these details can streamline the process and help avoid unnecessary delays in securing health benefits. Awareness of the requirements associated with the VA Form 10-7959C is essential for maintaining compliance and ensuring timely reimbursements.
Key takeaways
Understanding the VA Form 10-7959C is essential for beneficiaries using the CHAMPVA program. Here are key takeaways to consider:
- Purpose of the Form: This form certifies any other health insurance (OHI) you may have and is crucial for reimbursement from CHAMPVA.
- Information Required: Complete all sections fully. Missing information can result in delays or denials of claims.
- Submission Timing: Report changes in your health insurance as soon as they occur. Regular updates ensure that your records remain accurate.
- Medicare Information: If you are a Medicare beneficiary, you must include details about your Medicare coverage, including any relevant card copies.
- Document Attachments: Always attach copies of your health insurance cards, both front and back. This is necessary for processing your claims.
- Certification Statement: You must certify the accuracy of your information. Providing false statements can lead to serious legal consequences.
- Electronic Submission: If submitting online, you can attach necessary documents electronically, simplifying the process.
Completing the VA Form 10-7959C accurately helps ensure that you receive the full benefits for which you qualify. It is beneficial to keep records updated and ensure compliance with all requirements outlined in the form.
Browse Other Templates
I 131 Form - Expedited procedures require signed acknowledgment upon delivery of the card.
Employee Announcement Examples - Share the excitement of welcoming a new member to the team.
Icici Pay Direct Card Balance Check - Understand that fees and terms may change, and it’s your responsibility to stay updated.