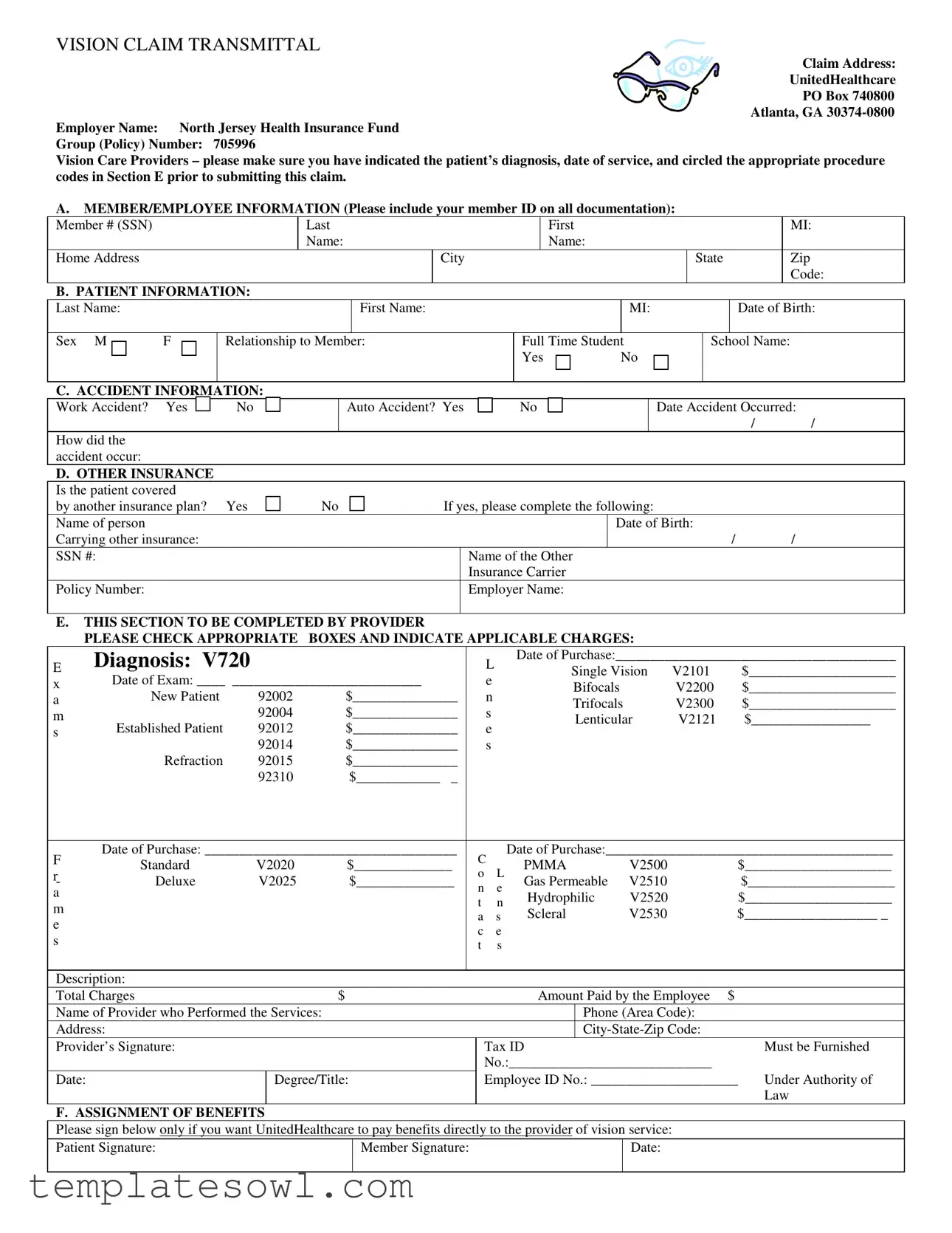
Fill Out Your Vision Claim Transmittal Form
The Vision Claim Transmittal form serves as a crucial document for the submission of vision care claims to UnitedHealthcare. It streamlines the reimbursement process, ensuring that all necessary information is captured accurately and efficiently. Key components of the form include sections for member and patient information, where important identifiers such as the member ID and personal details, including date of birth and relationship to the member, must be provided. Additionally, the form requires specific information related to any accidents that may have occurred, as well as inquiries about coverage from other insurance plans. Vital for the serving provider, Section E outlines the procedures performed, allowing providers to indicate applicable diagnosis codes and charges for the services rendered. Furthermore, there is a space designated for the assignment of benefits, enabling participants to authorize payment directly to the provider, facilitating quicker reimbursement. It is essential that providers complete the form thoroughly and avoid attaching receipts or bills to prevent processing delays, as the claims should be submitted directly to UnitedHealthcare's specified address, ensuring timely attention to vision care needs.
Vision Claim Transmittal Example
VISION CLAIM TRANSMITTAL
Claim Address:
UnitedHealthcare
PO Box 740800 Atlanta, GA
Employer Name: North Jersey Health Insurance Fund
Group (Policy) Number: 705996
Vision Care Providers – please make sure you have indicated the patient’s diagnosis, date of service, and circled the appropriate procedure codes in Section E prior to submitting this claim.
A.MEMBER/EMPLOYEE INFORMATION (Please include your member ID on all documentation):
|
Member # (SSN) |
|
|
Last |
|
|
|
|
|
Name: |
|
|
Home Address |
|
|
|
|
|
B. PATIENT INFORMATION: |
||||
|
|||||
|
Last Name: |
|
|
|
First Name: |
|
|
|
|
|
|
|
Sex M |
F |
Relationship to Member: |
||
|
|
|
|
|
|
City
|
|
First |
|
|
|
MI: |
|
|
|
Name: |
|
|
|
|
|
|
|
|
|
State |
|
Zip |
|
|
|
|
|
|
|
|
Code: |
|
|
|
MI: |
|
|
Date of Birth: |
|
|
|
|
|
|
|||
|
|
|
|
|
|||
Full Time Student |
|
School Name: |
|||||
Yes |
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
C. ACCIDENT INFORMATION:
Work Accident? Yes |
|
|
|
No |
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
How did the accident occur:
Auto Accident? Yes
No
Date Accident Occurred:
//
D.OTHER INSURANCE Is the patient covered
by another insurance plan? Yes
No
If yes, please complete the following:
Name of person |
|
Date of Birth: |
|
Carrying other insurance: |
|
/ |
/ |
SSN #: |
Name of the Other |
|
|
|
Insurance Carrier |
|
|
Policy Number: |
Employer Name: |
|
|
|
|
|
|
E. THIS SECTION TO BE COMPLETED BY PROVIDER |
|
|
|
|
|
|
|
|
|
||||
|
PLEASE CHECK APPROPRIATE |
BOXES AND INDICATE APPLICABLE CHARGES: |
|
|
|
||||||||
E |
Diagnosis: V720 |
|
|
|
|
|
L |
Date of Purchase:________________________________________ |
|||||
|
|
|
|
|
Single Vision |
V2101 |
|
$_____________________ |
|||||
x |
Date of Exam: ____ ___________________________ |
|
|
e |
|
||||||||
|
|
Bifocals |
|
V2200 |
|
$_____________________ |
|||||||
a |
New Patient |
92002 |
$_______________ |
|
|
n |
|
|
|||||
|
|
Trifocals |
|
V2300 |
|
$_____________________ |
|||||||
m |
|
92004 |
$_______________ |
|
|
s |
|
|
|||||
|
|
|
|
Lenticular |
V2121 |
|
$_________________ |
||||||
s |
Established Patient |
92012 |
$_______________ |
|
|
e |
|
|
|||||
|
|
|
|
|
|
|
|
||||||
|
92014 |
$_______________ |
|
|
s |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
||||
|
Refraction |
92015 |
$_______________ |
|
|
|
|
|
|
|
|
|
|
|
|
92310 |
$____________ _ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
F |
Date of Purchase: ____________________________________ |
|
C |
Date of Purchase:_________________________________________ |
|||||||||
Standard |
V2020 |
$______________ |
|
PMMA |
V2500 |
|
$_____________________ |
||||||
r- |
|
o |
L |
|
|||||||||
Deluxe |
V2025 |
$______________ |
|
Gas Permeable |
V2510 |
|
|
$_____________________ |
|||||
|
n |
e |
|
|
|||||||||
a |
|
|
|
|
|
Hydrophilic |
V2520 |
|
|
$_____________________ |
|||
|
|
|
|
|
t |
n |
|
|
|||||
m |
|
|
|
|
|
|
|
||||||
|
|
|
|
|
Scleral |
V2530 |
|
$___________________ _ |
|||||
|
|
|
|
|
a |
s |
|
||||||
e |
|
|
|
|
|
|
|||||||
|
|
|
|
|
c |
e |
|
|
|
|
|
|
|
s |
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
t |
s |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Description: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Total Charges |
|
|
$ |
|
|
|
Amount Paid by the Employee |
$ |
|
||||
Name of Provider who Performed the Services: |
|
|
|
|
Phone (Area Code): |
|
|
||||||
Address: |
|
|
|
|
|
|
|
|
|
||||
Provider’s Signature: |
|
|
|
|
|
Tax ID |
|
|
|
Must be Furnished |
|||
|
|
|
|
|
|
|
No.:_____________________________ |
|
|
||||
Date: |
|
Degree/Title: |
|
|
Employee ID No.: _____________________ |
Under Authority of |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Law |
F. ASSIGNMENT OF BENEFITS
Please sign below only if you want UnitedHealthcare to pay benefits directly to the provider of vision service:
Patient Signature: |
Member Signature: |
Date: |
|
|
|
NOTE: Please do not attach any receipts or bills to this form. Make sure form is completely filled out and mail only this form to the above address.
Form Characteristics
| Fact Name | Description |
|---|---|
| Claim Address | The completed Vision Claim Transmittal form should be sent to UnitedHealthcare at PO Box 740800, Atlanta, GA 30374-0800. |
| Employer Information | This form is associated with North Jersey Health Insurance Fund, and it requires the group (policy) number, which is 705996. |
| Patient Information | Include detailed patient information. This includes the patient’s last name, first name, and other identifiers like date of birth and relationship to the member. |
| Accident Section | Providers must check if there's any accident involved, indicating both work and auto accidents. This provides context for the claim. |
| Other Insurance Coverage | If the patient has other insurance, details such as name, date of birth, SSN, and policy number must be provided. |
| Provider Information | Providers must fill out their information, including signatures and tax ID numbers, ensuring all legal bases are covered. |
| Assignment of Benefits | Patients can assign benefits directly to the provider by signing the designated area on the form. |
| Filing Instructions | It's crucial not to attach any receipts or bills, just the completed form. Ensure it is fully filled out before mailing. |
Guidelines on Utilizing Vision Claim Transmittal
Completing the Vision Claim Transmittal form involves providing various personal details and information about the services rendered. This process ensures that all necessary information is conveyed clearly, allowing for efficient processing of the claim.
- Claim Address: Write the address for UnitedHealthcare: PO Box 740800, Atlanta, GA 30374-0800.
- Employer Name: Enter "North Jersey Health Insurance Fund."
- Group (Policy) Number: Fill in "705996."
- Member/Employee Information:
- Member # (SSN): Input the member's Social Security Number.
- Last Name: Provide the last name of the member.
- Home Address: Include the complete home address of the member.
- Patient Information:
- Last Name: Write the patient’s last name.
- First Name: Include the patient’s first name.
- Middle Initial: Add the patient’s middle initial.
- Date of Birth: Provide the patient’s date of birth.
- Sex: Circle M for male or F for female.
- Relationship to Member: State the relationship, such as "spouse" or "child."
- If applicable, indicate if the patient is a full-time student and the school name.
- City, State, and Zip Code: Complete the patient’s location information.
- Accident Information:
- Check "Yes" or "No" for work or auto accident and describe how the accident occurred.
- Include the date the accident occurred.
- Other Insurance:
- Indicate if the patient has another insurance plan by circling "Yes" or "No."
- If yes, complete details: name of person carrying the insurance, date of birth, Social Security number, name of the other insurance carrier, and policy number.
- Also provide employer name.
- Provider Section:
- Fill out applicable diagnosis and procedure codes by checking the appropriate boxes.
- Complete date of purchase and date of exam.
- List all charges for services rendered, including single vision, bifocals, etc.
- Provide the total charges and amount paid by the employee.
- Write the provider's name, phone number, and address. Include the provider’s signature, tax ID number, and date.
- Write the degree/title and employee ID number.
- Assignment of Benefits:
- Patients need to sign if they want UnitedHealthcare to pay the provider directly.
- Include member signature and date.
After completing the form, double-check that all sections are filled out accurately. Do not attach any receipts or bills—simply mail the filled-out form to the address listed at the top. This will ensure that your claim is processed smoothly and efficiently.
What You Should Know About This Form
What is the Vision Claim Transmittal form used for?
The Vision Claim Transmittal form is a document that healthcare providers use to submit claims for vision services rendered to a patient. It ensures that all necessary information about the patient, the services provided, and the related costs are communicated to the insurance provider for payment processing.
Where should I send the completed Vision Claim Transmittal form?
Once you have fully completed the form, it should be mailed to UnitedHealthcare at the following address: PO Box 740800, Atlanta, GA 30374-0800. Ensure that you only send this form without any additional receipts or bills attached, as those documents are not required.
What information is required from the member on the form?
The member needs to provide their member ID, social security number, last name, home address, and other identifying details. It is essential to include this information consistently across all documents submitted to prevent any processing delays.
What details must be provided about the patient?
The form requires information such as the patient’s last name, first name, date of birth, and relationship to the member. For dependents who are full-time students, you should also specify the name of the school they attend.
How should accident information be documented on the form?
If the vision claim is related to an accident, it’s crucial to check the boxes for "Work Accident" or "Auto Accident" as applicable. You must provide a brief description of how the accident occurred and the date on which it happened, if relevant.
What if the patient has other insurance coverage?
If the patient is covered by another insurance plan, this information needs to be filled out in the designated section. You will need to provide details such as the name of the insurance carrier, policy number, and the name and date of birth of the person carrying that insurance coverage.
What specific information should the vision care provider complete?
Providers must indicate the patient's diagnosis, services performed, associated charges, and dates of service in Section E of the form. They should also make sure to check the appropriate boxes for the procedures performed and sign the form as the provider responsible for delivering the services.
Do members need to sign the form?
Yes, the member and the patient (if applicable) must sign the form, especially if the member wants UnitedHealthcare to pay benefits directly to the provider. This signature authorizes the claim to be processed and helps prevent delays in payment.
Why shouldn’t receipts or bills be attached to the form?
Attaching receipts or bills to the Vision Claim Transmittal form can complicate the processing of the claim. The insurance company has a designated procedure for handling these claims, and including unnecessary documents could lead to confusion or processing errors. Stick to submitting just the completed form to ensure smooth handling of the claim.
Common mistakes
When people fill out the Vision Claim Transmittal form, several common mistakes can lead to delays or rejections of claims. The first mistake is an incomplete patient or member information section. Each detail counts, including the member ID, name, address, and date of birth. Omitting any of these elements may cause the claim to lack the necessary identification to be processed properly. Double-checking this section before submission can help ensure all fields are filled in completely and accurately.
Another frequent error involves the diagnosis and procedure codes. In Section E, it's vital for vision care providers to indicate the patient’s diagnosis and the correct procedures performed. If the provider does not circle the appropriate procedure codes, the claim may be misclassified or denied altogether. Properly documenting the relevant procedure codes ensures that the claim aligns with the services rendered.
Additionally, individuals often neglect to address other insurance coverage. If the patient has coverage from another insurer, it must be disclosed in Section D. Not reporting this information can result in missing out on potential benefits. Taking a moment to confirm whether other coverage exists can significantly impact the overall processing of the claim.
Finally, signatures and dates are sometimes overlooked. Section F requires the signatures of both the patient and the member, confirming the assignment of benefits to the provider. Without these signatures, the claim may lack authorization for payment. To avoid complications, one should ensure that all necessary signatures, along with the corresponding dates, are included before mailing the form.
Documents used along the form
The Vision Claim Transmittal form serves as a crucial document in the process of submitting a vision care claim. It outlines essential details related to the patient, the service provider, and the services rendered. Alongside this form, several other documents are typically required to support the claim. Below is a list of these complementary documents, along with concise descriptions of each.
- Claim Verification Form: This form is used to confirm the patient’s eligibility for vision services under their insurance policy. It includes details about the coverage limits and any necessary prerequisites.
- Patient Registration Form: Essential for establishing the patient’s demographic information, this form collects data like addresses, contact details, and insurance information.
- Diagnosis Certification: A document from the healthcare provider that clearly states the diagnosis of the patient. This can be pivotal in justifying the necessity of the claimed services.
- Treatment Plan: This outlines the recommended treatments or services following an examination. It helps prove the medical necessity of the services billed on the transmittal form.
- Explanation of Benefits (EOB): Provided by insurance companies, this summary details what was covered in previous claims. It can be useful for establishing continuity of care or addressing any coordination of benefits.
- Itemized Billing Statement: An organized listing of all charges related to the vision services provided, which helps clarify the costs associated with each specific service rendered.
- Authorization for Release of Information: This form allows the provider to disclose patient information to the insurance company, facilitating the claims process and ensuring compliance with privacy regulations.
- Coordination of Benefits Form: This document is necessary when a patient is covered by multiple insurance plans. It ensures that the insurance companies coordinate their payments efficiently.
- Proof of Payment: In cases of out-of-pocket expenses, a proof of payment document may be required to validate the amounts paid by the patient before claim submission.
Careful attention to these forms and documents can significantly streamline the claim process, ensuring that all necessary information is provided for optimal reimbursement and support of the patient's vision care needs.
Similar forms
The Vision Claim Transmittal form shares similarities with various other documents used in healthcare claims and insurance reimbursement processes. Below is a list detailing these documents and how they relate to the Vision Claim Transmittal form.
- Health Insurance Claim Form (CMS-1500): This form is also used for submitting claims for medical services to insurance companies. It requires patient, provider, and service details, much like the Vision Claim Transmittal form.
- Patient Demographic Form: This document collects essential patient information such as name, address, and insurance details, paralleling Section A of the Vision Claim Transmittal form focused on member and patient information.
- Authorization for Release of Medical Information: Patients often provide this form to authorize providers to share their health information. Similar to the assignment of benefits section in the Vision Claim Transmittal form, it involves patient consent.
- Explanation of Benefits (EOB): Once a claim is processed, this document explains what services were paid, denied, or adjusted. It functions as a follow-up to the claim process, similar to how the Vision Claim Transmittal form initiates it.
- Claim Appeals Letter: When a claim is denied, this document is used to formally request a review. It contains patient and provider details similar to those required in submitting the Vision Claim Transmittal form.
- Coordination of Benefits Form: This is utilized when multiple insurance policies are involved. It shares components with the 'Other Insurance' section in the Vision Claim Transmittal form, focusing on patient coverage.
- Referral Authorization Form: This document is often needed to obtain approval for specialist care. It bears resemblance to the requirement for specific procedure codes in Section E of the Vision Claim Transmittal form.
- Insurance Enrollment Form: This form collects information for enrolling individuals in an insurance plan. It also showcases the member’s details, aligning with the member/employee information section of the Vision Claim Transmittal form.
- Provider Network Directory: This is a guide that lists participating providers covered under a health plan. Its relevance mirrors the provider information request in the Vision Claim Transmittal form.
Dos and Don'ts
When filling out the Vision Claim Transmittal form, certain guidelines can help ensure your submission is processed smoothly. Here are seven important things to do and avoid:
- Do: Include the member ID on all documentation. This is crucial for identification purposes.
- Do: Make certain to fill in all sections completely. Missing information can lead to delays.
- Do: Circle the appropriate procedure codes in Section E. This helps clarify the services rendered.
- Do: Ensure that the patient’s diagnosis and date of service are accurately indicated. This information is essential for processing the claim.
- Do: Confirm the patient's full-time student status if applicable. This might affect eligibility for certain benefits.
- Do: Obtain necessary signatures from both the patient and the member. This authorization is necessary for benefits assignment.
- Do: Mail only the completed form to the specified address. Avoid sending additional receipts or bills as instructed.
- Don't: Leave any section blank. Incomplete forms can result in denial or delay.
- Don't: Fail to provide the date of services or the nature of the diagnosis. Inaccuracies can lead to complications.
- Don't: Forget to provide the name of the insurance carrier if there is other insurance involved. This information must be correctly reported.
- Don't: Use white-out or scribble on the form. Clarity is important; messy paperwork may be rejected.
- Don't: Submit the form without verifying all entries for accuracy. Simple mistakes can create significant delays.
- Don't: Attach any receipts or invoices. Only the completed form should be included.
- Don't: Post the form without proper postage. Ensure it is adequately stamped to prevent returns.
Misconceptions
When it comes to the Vision Claim Transmittal form, several misconceptions might hinder its proper completion. It's crucial to clarify these misunderstandings to ensure a smooth claims process.
- Misconception 1: The form can be submitted with missing information.
- Misconception 2: Patients are not required to provide diagnosis information.
- Misconception 3: Supporting documents should be attached to the form.
- Misconception 4: Only new patients require a detailed form.
- Misconception 5: The provider does not need to sign the form.
- Misconception 6: The form is only necessary for vision services under the member's insurance.
Incomplete forms will typically lead to delays or denials. Each section needs to be filled out thoroughly to facilitate quick processing.
It's essential to include the patient's diagnosis, date of service, and relevant procedure codes. This detail is necessary for proper assessment of the claim.
The guidelines explicitly state that no receipts or bills should accompany the form. Ensure you follow this instruction to avoid issues.
Both new and established patients must provide complete information. This ensures that the claims process is efficient for everyone involved.
A signature from the provider who performed the services is mandatory. This confirmation verifies that the services were indeed rendered as stated.
If the patient has additional insurance, it is vital to indicate this on the form. This transparency allows for potential coordination of benefits.
By addressing these misconceptions, individuals can enhance their understanding of the claims process and contribute to a more efficient system for filing vision care claims.
Key takeaways
The Vision Claim Transmittal form is a vital document for processing vision claims effectively. Below are key takeaways to ensure accurate completion and submission:
- Accurate Information: It is crucial to fill in the member and patient information completely to avoid delays. Ensure the member ID is included in all documentation.
- Provider Section: Vision care providers must indicate the patient’s diagnosis, date of service, and appropriate procedure codes in Section E before submitting the claim.
- Accident Information: If applicable, clearly state whether the vision issue is related to a work or auto accident. This information helps in the claims process.
- Additional Insurance: If the patient has other insurance coverage, this must be disclosed. Complete the relevant sections to ensure that all potential benefits are considered.
- No Attachments: It is important to remember that receipts or bills should not be attached to the form. Send only the completed form to the designated address.
Browse Other Templates
Heroin - Provide the date when the previous marriage ended.
Maritime College Scholarship Application,New York State Cadet Scholarship Form,SUNY Maritime Cadet Program Application,Excellence in Maritime Education Scholarship,Cadet Appointment Program Application,Leadership and Adventure Scholarship Form,SUNY M - The scholarship is open to high school graduates, current students, and those with equivalent education.