Fill Out Your Vyvanse Coupon Form
The Vyvanse Coupon form is an essential tool for patients seeking to manage their medication costs effectively. Designed for use with three different plans—Patient Choice, Therapy First, and Therapy First Plus—it provides detailed instructions on how to file insurance claims related to Vyvanse prescriptions. This form captures all the necessary billing information, from patient identification to claim specifics, ensuring a smooth transaction process. Each plan has unique identifiers, such as BIN and PCN numbers, which are crucial for proper processing. Furthermore, the form indicates mandatory and optional fields to guide users on which information is necessary for successful claim submissions. Beyond billing, it also addresses various rejected claims and essential follow-up actions. Whether you're a pharmacy professional managing claims or a patient aiming to utilize your benefits, understanding and completing the Vyvanse Coupon form accurately can significantly impact your healthcare experience.
Vyvanse Coupon Example
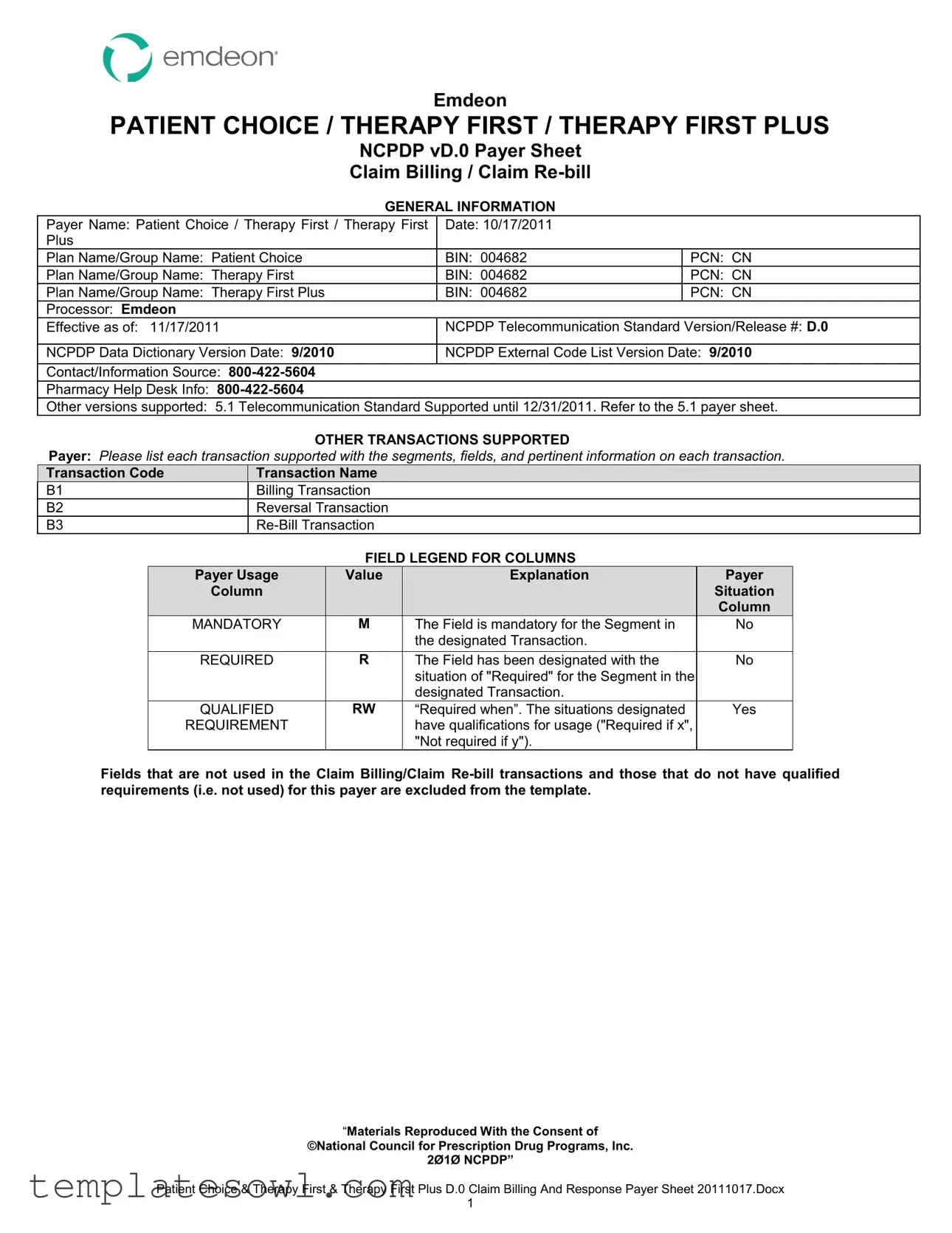
Emdeon
PATIENT CHOICE / THERAPY FIRST / THERAPY FIRST PLUS
NCPDP vD.0 Payer Sheet
Claim Billing / Claim
GENERAL INFORMATION
Payer Name: Patient Choice / Therapy First / Therapy First |
Date: 10/17/2011 |
|
Plus |
|
|
Plan Name/Group Name: Patient Choice |
BIN: 004682 |
PCN: CN |
Plan Name/Group Name: Therapy First |
BIN: 004682 |
PCN: CN |
Plan Name/Group Name: Therapy First Plus |
BIN: 004682 |
PCN: CN |
Processor: Emdeon |
|
|
Effective as of: 11/17/2011 |
NCPDP Telecommunication Standard Version/Release #: D.0 |
|
|
|
|
NCPDP Data Dictionary Version Date: 9/2010 |
NCPDP External Code List Version Date: 9/2010 |
|
|
|
|
Contact/Information Source:
Pharmacy Help Desk Info:
Other versions supported: 5.1 Telecommunication Standard Supported until 12/31/2011. Refer to the 5.1 payer sheet.
OTHER TRANSACTIONS SUPPORTED
Payer: Please list each transaction supported with the segments, fields, and pertinent information on each transaction.
Transaction Code |
Transaction Name |
B1 |
Billing Transaction |
B2 |
Reversal Transaction |
B3 |
FIELD LEGEND FOR COLUMNS
Payer Usage |
Value |
Explanation |
Payer |
Column |
|
|
Situation |
|
|
|
Column |
MANDATORY |
M |
The Field is mandatory for the Segment in |
No |
|
|
the designated Transaction. |
|
|
|
|
|
REQUIRED |
R |
The Field has been designated with the |
No |
|
|
situation of "Required" for the Segment in the |
|
|
|
designated Transaction. |
|
QUALIFIED |
RW |
“Required when”. The situations designated |
Yes |
REQUIREMENT |
|
have qualifications for usage ("Required if x", |
|
|
|
"Not required if y"). |
|
Fields that are not used in the Claim Billing/Claim
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
1

CLAIM BILLING/CLAIM
The following lists the segments and fields in a Claim Billing or Claim
Transaction Header Segment Questions |
|
Check |
Claim Billing/Claim |
|
|
|||
|
|
|
|
|
If Situational, Payer Situation |
|||
This Segment is always sent |
|
X |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Transaction Header Segment |
|
|
|
|
Claim Billing/Claim |
|
Field # |
NCPDP Field Name |
|
Value |
|
Payer |
Payer Situation |
||
|
|
|
|
|
|
Usage |
|
|
|
BIN NUMBER |
|
004682 |
|
M |
|
|
|
|
VERSION/RELEASE NUMBER |
|
DØ |
|
M |
|
|
|
|
TRANSACTION CODE |
|
B1 OR B3 |
|
M |
|
|
|
|
PROCESSOR CONTROL NUMBER |
|
CN |
|
M |
|
|
|
|
TRANSACTION COUNT |
|
1 |
|
M |
|
|
|
|
SERVICE PROVIDER ID QUALIFIER |
|
01 – NPI |
|
M |
|
|
|
|
SERVICE PROVIDER ID |
|
NPI |
|
M |
|
|
|
|
DATE OF SERVICE |
|
|
|
M |
|
|
|
|
SOFTWARE |
|
ALL SPACES |
M |
|
|
||
|
|
VENDOR/CERTIFICATION ID |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Insurance Segment Questions |
|
Check |
Claim Billing/Claim |
|
|
|||
|
|
|
|
|
If Situational, Payer Situation |
|||
This Segment is always sent |
|
X |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Insurance Segment |
|
|
|
|
|
Claim Billing/Claim |
|
|
Segment Identification |
|
|
|
|
|
|
|
|
“Ø4” |
|
|
|
|
|
|
Field # |
NCPDP Field Name |
|
Value |
|
Payer |
|
Payer Situation |
|
|
|
|
|
|
|
Usage |
|
|
|
CARDHOLDER ID |
|
|
|
M |
|
|
|
|
GROUP ID |
|
|
|
R |
Imp Guide: Required if necessary for |
||
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
|
|
|
|
|
|
|
Required if needed for pharmacy claim |
|
|
|
|
|
|
|
|
processing and payment. |
|
|
|
|
|
|
|
|||
Patient Segment Questions |
|
Check |
Claim Billing/Claim |
|
|
|||
|
|
|
|
|
If Situational, Payer Situation |
|||
This Segment is always sent |
|
X |
|
|
|
|
||
This Segment is situational |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Patient Segment |
|
|
|
|
|
Claim Billing/Claim |
|
|
Segment Identification |
|
|
|
|
|
|
|
|
“Ø1” |
|
|
|
|
|
|
Field |
NCPDP Field Name |
|
Value |
|
Payer |
|
Payer Situation |
|
|
|
|
|
|
|
Usage |
|
|
|
DATE OF BIRTH |
|
|
|
R |
|
|
|
|
PATIENT GENDER CODE |
|
|
|
R |
|
|
|
|
PATIENT FIRST NAME |
|
|
|
R |
Imp Guide: Required when the patient has |
||
|
|
|
|
|
|
|
a first name. |
|
|
PATIENT LAST NAME |
|
|
|
R |
|
|
|
|
PATIENT STREET ADDRESS |
|
|
|
RW |
Imp Guide: Optional. |
||
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
available. |
|
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
2

|
|
|
Patient Segment |
|
|
|
|
Claim Billing/Claim |
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“Ø1” |
|
|
|
|
|
Field |
NCPDP Field Name |
|
Value |
Payer |
|
Payer Situation |
||
|
|
|
|
|
|
Usage |
|
|
|
|
PATIENT CITY ADDRESS |
|
|
RW |
Imp Guide: Optional. |
||
|
|
|
|
|
|
|
Payer Requirement : Required when |
|
|
|
|
|
|
|
|
available. |
|
|
|
PATIENT STATE / |
|
|
RW |
Imp Guide: Optional. |
||
|
|
|
PROVINCE ADDRESS |
|
|
|
|
|
|
|
|
|
|
|
|
Payer Requirement : Required when |
|
|
|
|
|
|
|
|
available. |
|
|
|
PATIENT ZIP / POSTAL ZONE |
|
|
RW |
Imp Guide: Optional. |
||
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
available. |
|
|
|
PATIENT PHONE NUMBER |
|
|
RW |
Imp Guide: Optional. |
||
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
available. |
|
|
|
PATIENT |
|
|
RW |
Imp Guide: May be submitted for the |
||
|
|
|
|
|
|
|
receiver to relay patient health care |
|
|
|
|
|
|
|
|
communications via the Internet when |
|
|
|
|
|
|
|
|
provided by the patient. |
|
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
available. |
|
Claim Segment Questions |
|
Check |
Claim Billing/Claim |
|
|
|||
|
|
|
|
|
If Situational, Payer Situation |
|||
This Segment is always sent |
|
X |
|
|
|
|
||
This payer supports partial fills |
|
|
|
|
|
|
||
This payer does not support partial fills |
|
X |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Claim Segment |
|
|
|
|
|
Claim Billing/Claim |
|
|
Segment Identification |
|
|
|
|
|
|
|
|
“Ø7” |
|
|
|
|
|
|
Field # |
NCPDP Field Name |
|
Value |
|
Payer |
|
Payer Situation |
|
|
|
|
|
|
|
Usage |
|
|
|
PRESCRIPTION/SERVICE |
|
1 = Rx Billing |
M |
|
Imp Guide: For Transaction Code of |
||
|
|
REFERENCE NUMBER QUALIFIER |
|
|
|
|
|
“B1”, in the Claim Segment, the |
|
|
|
|
|
|
|
|
Prescription/Service Reference Number |
|
|
|
|
|
|
|
|
Qualifier |
|
PRESCRIPTION/SERVICE |
|
up to 12 positions |
M |
|
|
||
|
|
REFERENCE NUMBER |
|
|
|
|
|
|
|
PRODUCT/SERVICE ID QUALIFIER |
|
03 - NDC |
|
M |
|
00 if Compound Code |
|
|
PRODUCT/SERVICE ID |
|
11 digit NDC |
M |
|
0 if Compound Code |
||
|
QUANTITY DISPENSED |
|
Format 9(7)V999 |
R |
|
|
||
|
|
|
|
|
|
|
|
|
|
FILL NUMBER |
|
New = 00 (zeros must be |
R |
|
|
||
|
|
|
|
sent) |
|
|
|
|
|
DAYS SUPPLY |
|
|
|
R |
|
|
|
|
COMPOUND CODE |
|
1 = Not a Compound |
R |
Refer to Compound Segment when |
|||
|
|
|
|
2 = Compound |
|
Compound Code |
||
|
DISPENSE AS WRITTEN |
|
|
|
R |
|
|
|
|
|
(DAW)/PRODUCT SELECTION CODE |
|
|
|
|
|
|
|
DATE PRESCRIPTION WRITTEN |
|
|
|
R |
|
|
|
|
NUMBER OF REFILLS AUTHORIZED |
|
|
|
R |
Imp Guide: Required if necessary for plan |
||
|
|
|
|
|
|
|
benefit administration. |
|
|
|
“Materials Reproduced With the Consent of |
|
|
||||
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
3

|
|
|
Claim Segment |
|
|
|
|
Claim Billing/Claim |
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“Ø7” |
|
|
|
|
|
Field # |
|
NCPDP Field Name |
Value |
Payer |
|
Payer Situation |
||
|
|
|
|
|
|
Usage |
|
|
|
PRESCRIPTION ORIGIN CODE |
|
R |
Imp Guide: Required if necessary for plan |
||||
|
|
|
|
|
|
|
benefit administration. |
|
|
SUBMISSION CLARIFICATION CODE |
Maximum count of 3. |
RW |
Imp Guide: Required if Submission |
||||
|
|
COUNT |
|
|
Clarification Code |
|||
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
SUBMISSION CLARIFICATION CODE |
|
RW |
Imp Guide: Required if clarification is |
||||
|
|
|
|
|
|
|
needed and value submitted is greater |
|
|
|
|
|
|
|
|
than zero (Ø). |
|
|
|
|
|
|
|
|
If the Date of Service |
|
|
|
|
|
|
|
|
the subsequent payer coverage date, the |
|
|
|
|
|
|
|
|
Submission Clarification Code |
|
|
|
|
|
|
|
|
is required with value of “19” (Split Billing |
|
|
|
|
|
|
|
|
– indicates the quantity dispensed is the |
|
|
|
|
|
|
|
|
remainder billed to a subsequent payer |
|
|
|
|
|
|
|
|
when Medicare Part A expires. Used only |
|
|
|
|
|
|
|
|
in |
|
|
|
|
|
|
|
|
unit of use medications. |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
OTHER COVERAGE CODE |
0 = Not specified by patient |
RW |
Imp Guide: Required if needed by |
||||
|
|
|
|
|
1 = No other coverage |
|
receiver, to communicate a summation of |
|
|
|
|
|
|
3 = Other coverage exist – |
|
other coverage information that has been |
|
|
|
|
|
|
claim not covered* |
|
collected from other payers. |
|
|
|
|
|
|
8 = Claim is billing for patient |
|
|
|
|
|
|
|
|
financial responsibility |
|
Required for Coordination of Benefits. |
|
|
|
|
|
|
only* |
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide. |
|
|
|
|
|
|
|
|
*requires COB segment to be sent. |
|
|
PRIOR AUTHORIZATION TYPE CODE |
1 = Prior Authorization, if |
RW |
Imp Guide: Required if this field could |
||||
|
|
|
|
|
applicable |
|
result in different coverage, pricing, or |
|
|
|
|
|
|
|
|
patient financial responsibility. |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
PRIOR AUTHORIZATION NUMBER |
If applicable to Rx |
RW |
Imp Guide: Required if this field could |
||||
|
|
SUBMITTED |
|
|
result in different coverage, pricing, or |
|||
|
|
|
|
|
|
|
patient financial responsibility. |
|
|
|
|
|
|
|
|
Payer Requirement: Same As Imp Guide |
|
|
ROUTE OF ADMINISTRATION |
|
RW |
Imp Guide: Required if specified in trading |
||||
|
|
|
|
|
|
|
partner agreement. |
|
|
|
|
|
|
|
|
Payer Requirement: When compound |
|
|
|
|
|
|
|
|
code |
|
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
4

Pricing Segment Questions |
|
Check |
Claim Billing/Claim |
|
||||
|
|
|
|
|
If Situational, Payer Situation |
|
||
This Segment is always sent |
|
X |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Pricing Segment |
|
|
|
|
|
Claim Billing/Claim |
|
|
|
|
|
|
|
|
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
“11” |
|
|
|
|
|
|
Field # |
NCPDP Field Name |
|
Value |
|
Payer |
|
Payer Situation |
|
|
|
|
|
|
|
Usage |
|
|
|
INGREDIENT COST SUBMITTED |
|
|
|
R |
|
|
|
|
DISPENSING FEE SUBMITTED |
|
|
|
R |
|
Imp Guide: Required if its value has an |
|
|
|
|
|
|
|
|
|
effect on the Gross Amount Due (43Ø- |
|
|
|
|
|
|
|
|
DU) calculation. |
|
PATIENT PAID AMOUNT SUBMITTED |
|
|
|
R |
|
Imp Guide: Required if this field could |
|
|
|
|
|
|
|
|
|
result in different coverage, pricing, or |
|
|
|
|
|
|
|
|
patient financial responsibility. |
|
INCENTIVE AMOUNT SUBMITTED |
|
|
|
RW |
|
Imp Guide: Required if its value has an |
|
|
|
|
|
|
|
|
|
effect on the Gross Amount Due (43Ø- |
|
|
|
|
|
|
|
|
DU) calculation. |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
OTHER AMOUNT CLAIMED |
|
Maximum count of 3. |
RW |
|
Imp Guide: Required if Other Amount |
||
|
|
SUBMITTED COUNT |
|
|
|
|
|
Claimed Submitted Qualifier |
|
|
|
|
|
|
|
|
used. |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
OTHER AMOUNT CLAIMED |
|
|
|
RW |
|
Imp Guide: Required if Other Amount |
|
|
|
SUBMITTED QUALIFIER |
|
|
|
|
|
Claimed Submitted |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
OTHER AMOUNT CLAIMED |
|
|
|
RW |
|
Imp Guide: Required if its value has an |
|
|
|
SUBMITTED |
|
|
|
|
|
effect on the Gross Amount Due (43Ø- |
|
|
|
|
|
|
|
|
DU) calculation. |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
FLAT SALES TAX AMOUNT |
|
|
|
RW |
|
Imp Guide: Required if its value has an |
|
|
|
SUBMITTED |
|
|
|
|
|
effect on the Gross Amount Due (43Ø- |
|
|
|
|
|
|
|
|
DU) calculation. |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide. |
|
|
|
|
|
|
|
|
If Sales Tax applies to State. |
|
PERCENTAGE SALES TAX AMOUNT |
|
|
|
RW |
|
Imp Guide: Required if its value has an |
|
|
|
SUBMITTED |
|
|
|
|
|
effect on the Gross Amount Due (43Ø- |
|
|
|
|
|
|
|
|
DU) calculation. |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide. |
|
|
|
|
|
|
|
|
If Sales Tax applies to State. |
|
PERCENTAGE SALES TAX RATE |
|
|
|
RW |
|
Imp Guide: Required if Percentage Sales |
|
|
|
SUBMITTED |
|
|
|
|
|
Tax Amount Submitted |
|
|
|
|
|
|
|
|
Percentage Sales Tax Basis Submitted |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Required if this field could result in |
|
|
|
|
|
|
|
|
different pricing. |
|
|
|
|
|
|
|
|
Required if needed to calculate |
|
|
|
|
|
|
|
|
Percentage Sales Tax Amount Paid (559- |
|
|
|
|
|
|
|
|
AX). |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide. |
|
|
|
|
|
|
|
|
If Sales Tax applies to State. |
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
5

|
|
|
Pricing Segment |
|
|
|
|
Claim Billing/Claim |
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“11” |
|
|
|
|
|
Field # |
NCPDP Field Name |
|
Value |
Payer |
|
Payer Situation |
||
|
|
|
|
|
|
Usage |
|
|
|
PERCENTAGE SALES TAX BASIS |
|
|
RW |
Imp Guide: Required if Percentage Sales |
|||
|
|
SUBMITTED |
|
|
|
Tax Amount Submitted |
||
|
|
|
|
|
|
|
Percentage Sales Tax Rate Submitted |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Required if this field could result in |
|
|
|
|
|
|
|
|
different pricing. |
|
|
|
|
|
|
|
|
Required if needed to calculate |
|
|
|
|
|
|
|
|
Percentage Sales Tax Amount Paid (559- |
|
|
|
|
|
|
|
|
AX). |
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide. |
|
|
|
|
|
|
|
|
If Sales Tax applies to State. |
|
|
USUAL AND CUSTOMARY CHARGE |
|
|
R |
Imp Guide: Required if needed per trading |
|||
|
|
|
|
|
|
|
partner agreement. |
|
|
GROSS AMOUNT DUE |
|
|
R |
|
|
||
|
BASIS OF COST DETERMINATION |
|
|
R |
Imp Guide: Required if needed for |
|||
|
|
|
|
|
|
|
receiver claim/encounter adjudication. |
|
Prescriber Segment Questions |
|
Check |
|
Claim Billing/Claim |
|
|||||
|
|
|
|
|
|
|
If Situational, Payer Situation |
|
||
|
|
|
|
|
|
|
|
|||
This Segment is always sent |
|
X |
|
|
|
|
|
|||
This Segment is situational |
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Prescriber Segment |
|
|
|
|
|
|
Claim Billing/Claim |
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“Ø3” |
|
|
|
|
|
|
|
Field # |
NCPDP Field Name |
|
Value |
|
Payer |
|
Payer Situation |
|||
|
|
|
|
|
|
|
|
Usage |
|
|
|
PRESCRIBER ID QUALIFIER |
|
01 – NPI |
|
R |
|
Imp Guide: Required if Prescriber ID (411- |
|||
|
|
|
|
|
12 - DEA |
|
|
|
DB) is used. |
|
|
PRESCRIBER ID |
|
NPI or DEA |
|
R |
|
Imp Guide: Required if this field could |
|||
|
|
|
|
|
|
|
|
|
|
result in different coverage or patient |
|
|
|
|
|
|
|
|
|
|
financial responsibility. |
|
|
|
|
|
|
|
|
|
|
Required if necessary for |
|
|
|
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
PRESCRIBER LAST NAME |
|
|
|
|
RW |
|
Imp Guide: Required when the Prescriber |
||
|
|
|
|
|
|
|
|
|
|
ID |
|
|
|
|
|
|
|
|
|
|
Required if needed for Prescriber ID (411- |
|
|
|
|
|
|
|
|
|
|
DB) validation/clarification. |
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
|
|
submitting DEA |
|
PRESCRIBER FIRST NAME |
|
|
|
|
RW |
|
Imp Guide: Required if needed to assist in |
||
|
|
|
|
|
|
|
|
|
|
identifying the prescriber. |
|
|
|
|
|
|
|
|
|
|
Required if necessary for |
|
|
|
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
|
|
submitting DEA |
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
6

|
|
|
Prescriber Segment |
|
|
|
|
Claim Billing/Claim |
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“Ø3” |
|
|
|
|
|
Field # |
NCPDP Field Name |
|
Value |
Payer |
|
Payer Situation |
||
|
|
|
|
|
|
Usage |
|
|
|
PRESCRIBER STREET ADDRESS |
|
|
RW |
Imp Guide: Required if needed to assist in |
|||
|
|
|
|
|
|
|
identifying the prescriber. |
|
|
|
|
|
|
|
|
Required if necessary for |
|
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
submitting DEA |
|
|
PRESCRIBER CITY ADDRESS |
|
|
RW |
Imp Guide: Required if needed to assist in |
|||
|
|
|
|
|
|
|
identifying the prescriber. |
|
|
|
|
|
|
|
|
Required if necessary for |
|
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
submitting DEA |
|
|
PRESCRIBER STATE/PROVINCE |
|
|
RW |
Imp Guide: Required if needed to assist in |
|||
|
|
ADDRESS |
|
|
|
identifying the prescriber. |
||
|
|
|
|
|
|
|
Required if necessary for |
|
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
submitting DEA |
|
|
PRESCRIBER ZIP/POSTAL ZONE |
|
|
RW |
Imp Guide: Required if needed to assist in |
|||
|
|
|
|
|
|
|
identifying the prescriber. |
|
|
|
|
|
|
|
|
Required if necessary for |
|
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
|
|
|
|
|
|
|
Payer Requirement: Required when |
|
|
|
|
|
|
|
|
submitting DEA |
|
Coordination of Benefits/Other Payments |
|
Check |
Claim Billing/Claim |
|
|
|
|||||
Segment Questions |
|
|
If Situational, Payer Situation |
|
|
|
|||||
This Segment is always sent |
|
|
|
|
|
|
|
|
|
||
This Segment is situational |
|
X |
Required |
only for secondary, tertiary, etc claims. |
Other |
Coverage |
|||||
|
|
|
|
|
Code |
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
Scenario 2 - Other |
|
X |
Required |
only for secondary, tertiary, etc claims. |
Other |
Coverage |
|||||
Amount Repetitions and Benefit Stage Repetitions |
|
|
Code |
|
|
|
|||||
Only |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Coordination of Benefits/Other |
|
|
|
|
|
|
Claim Billing/Claim |
|
|
|
|
Payments Segment |
|
|
|
|
|
|
|
|
|
|
|
Segment Identification |
|
|
|
|
|
|
Scenario 2- Other |
||
|
|
“Ø5” |
|
|
|
|
|
|
Responsibility Amount Repetitions and |
||
|
|
|
|
|
|
|
|
|
Benefit Stage Repetitions Only |
|
|
Field # |
NCPDP Field Name |
|
Value |
|
|
Payer |
|
Payer Situation |
|
|
|
|
|
|
|
|
|
|
Usage |
|
|
|
|
|
COORDINATION OF |
|
Maximum count of 9. |
|
M |
|
|
|
|
||
|
|
BENEFITS/OTHER PAYMENTS |
|
|
|
|
|
|
|
|
|
|
|
COUNT |
|
|
|
|
|
|
|
|
|
|
OTHER PAYER COVERAGE TYPE |
|
|
|
|
M |
|
|
|
|
|
|
OTHER PAYER ID QUALIFIER |
|
03 - BIN |
|
|
R |
|
Imp Guide: Required if Other Payer ID |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“Materials Reproduced With the Consent of |
|
|
|
||||||
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
7

|
|
|
Coordination of Benefits/Other |
|
|
|
|
|
|
|
|
Claim Billing/Claim |
|
|
|
|
Payments Segment |
|
|
|
|
|
|
|
|
|
|
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
Scenario 2- Other |
|
|
|
|
“Ø5” |
|
|
|
|
|
|
|
|
Responsibility Amount Repetitions and |
|
|
|
|
|
|
|
|
|
|
|
|
|
Benefit Stage Repetitions Only |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Field # |
|
NCPDP Field Name |
|
Value |
|
|
Payer |
|
Payer Situation |
||||
|
|
|
|
|
|
|
|
|
|
Usage |
|
|
|
|
OTHER PAYER ID |
|
BIN |
|
|
R |
|
Imp Guide: Required if identification of the |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
Other Payer is necessary for |
|
|
|
|
|
|
|
|
|
|
|
|
|
claim/encounter adjudication. |
|
|
OTHER PAYER REJECT COUNT |
|
Maximum count of 5. |
RW |
|
Imp Guide: Required if Other Payer Reject |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
Code |
|
|
|
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
OTHER PAYER REJECT CODE |
|
|
|
|
|
RW |
|
Imp Guide: Required when the other |
||||
|
|
|
|
|
|
|
|
|
|
|
|
payer has denied the payment for the |
|
|
|
|
|
|
|
|
|
|
|
|
|
billing, designated with Other Coverage |
|
|
|
|
|
|
|
|
|
|
|
|
|
Code |
|
|
|
|
|
|
|
|
|
|
|
|
|
Billed – claim not covered). |
|
|
|
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
OTHER |
|
Maximum count of 25. |
RW |
|
Imp Guide: Required if Other Payer- |
|||||||
|
|
RESPONSIBILITY AMOUNT COUNT |
|
|
|
|
|
|
|
Patient Responsibility Amount Qualifier |
|||
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
OTHER |
|
|
|
|
|
RW |
|
Imp Guide: Required if Other Payer- |
||||
|
|
RESPONSIBILITY AMOUNT |
|
|
|
|
|
|
|
Patient Responsibility Amount |
|||
|
|
QUALIFIER |
|
|
|
|
|
|
|
used. |
|||
|
|
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
OTHER |
|
|
|
|
|
RW |
|
Imp Guide: Required if necessary for |
||||
|
|
RESPONSIBILITY AMOUNT |
|
|
|
|
|
|
|
patient financial responsibility only billing. |
|||
|
|
|
|
|
|
|
|
|
|
|
|
Required if necessary for |
|
|
|
|
|
|
|
|
|
|
|
|
|
state/federal/regulatory agency programs. |
|
|
|
|
|
|
|
|
|
|
|
|
|
Not used for |
|
|
|
|
|
|
|
|
|
|
|
|
|
programs if Other Payer Amount Paid |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
Payer Requirement: Same as Imp Guide |
|
|
|
|
|
|
|
|
|
|
|||||
DUR/PPS Segment Questions |
|
Check |
|
Claim Billing/Claim |
|
|
|||||||
|
|
|
|
|
|
|
|
|
If Situational, Payer Situation |
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|||
This Segment is always sent |
|
|
|
|
|
|
|
|
|
|
|||
This Segment is situational |
|
|
|
X |
for use to define professional service or override clinical edits |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
DUR/PPS Segment |
|
|
|
|
|
|
|
Claim Billing/Claim |
|
|
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
“Ø8” |
|
|
|
|
|
|
|
|
|
|
Field # |
NCPDP Field Name |
|
|
Value |
|
|
Payer |
|
Payer Situation |
||||
|
|
|
|
|
|
|
|
|
|
Usage |
|
|
|
|
DUR/PPS CODE COUNTER |
|
Maximum of 9 occurrences. |
R |
|
Imp Guide: Required if DUR/PPS |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
Segment is used. |
|
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
8

|
|
|
DUR/PPS Segment |
|
|
|
|
|
Claim Billing/Claim |
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
“Ø8” |
|
|
|
|
|
|
Field # |
NCPDP Field Name |
|
|
Value |
Payer |
|
Payer Situation |
||
|
|
|
|
|
|
|
Usage |
|
|
|
REASON FOR SERVICE CODE |
|
|
|
R |
Imp Guide: Required if this field could |
|||
|
|
|
|
|
|
|
|
result in different coverage, pricing, |
|
|
|
|
|
|
|
|
|
patient financial responsibility, and/or drug |
|
|
|
|
|
|
|
|
|
utilization review outcome. |
|
|
|
|
|
|
|
|
|
Required if this field affects payment for or |
|
|
|
|
|
|
|
|
|
documentation of professional pharmacy |
|
|
|
|
|
|
|
|
|
service. |
|
|
PROFESSIONAL SERVICE CODE |
|
|
|
R |
Imp Guide: Required if this field could |
|||
|
|
|
|
|
|
|
|
result in different coverage, pricing, |
|
|
|
|
|
|
|
|
|
patient financial responsibility, and/or drug |
|
|
|
|
|
|
|
|
|
utilization review outcome. |
|
|
|
|
|
|
|
|
|
Required if this field affects payment for or |
|
|
|
|
|
|
|
|
|
documentation of professional pharmacy |
|
|
|
|
|
|
|
|
|
service. |
|
|
RESULT OF SERVICE CODE |
|
|
|
R |
Imp Guide: Required if this field could |
|||
|
|
|
|
|
|
|
|
result in different coverage, pricing, |
|
|
|
|
|
|
|
|
|
patient financial responsibility, and/or drug |
|
|
|
|
|
|
|
|
|
utilization review outcome. |
|
|
|
|
|
|
|
|
|
Required if this field affects payment for or |
|
|
|
|
|
|
|
|
|
documentation of professional pharmacy |
|
|
|
|
|
|
|
|
|
service. |
|
|
DUR/PPS LEVEL OF EFFORT |
|
|
|
R |
Imp Guide: Required if this field could |
|||
|
|
|
|
|
|
|
|
result in different coverage, pricing, |
|
|
|
|
|
|
|
|
|
patient financial responsibility, and/or drug |
|
|
|
|
|
|
|
|
|
utilization review outcome. |
|
|
|
|
|
|
|
|
|
Required if this field affects payment for or |
|
|
|
|
|
|
|
|
|
documentation of professional pharmacy |
|
|
|
|
|
|
|
|
|
service. |
|
|
DUR |
|
|
|
R |
Imp Guide: Required if DUR |
|||
|
|
|
|
|
|
|
|
||
|
DUR |
|
|
|
R |
Imp Guide: Required if this field could |
|||
|
|
|
|
|
|
|
|
result in different coverage, pricing, |
|
|
|
|
|
|
|
|
|
patient financial responsibility, and/or drug |
|
|
|
|
|
|
|
|
|
utilization review outcome. |
|
|
|
|
|
|
|
|
|
Required if this field affects payment for or |
|
|
|
|
|
|
|
|
|
documentation of professional pharmacy |
|
|
|
|
|
|
|
|
|
service. |
|
Compound Segment Questions |
|
|
Check |
Claim Billing/Claim |
||||||||||
|
|
|
|
|
|
|
|
|
|
If Situational, Payer Situation |
||||
This Segment is always sent |
|
|
|
|
|
|
|
|
|
|
||||
This Segment is situational |
|
|
|
|
X |
required when Compound Code |
||||||||
|
|
|
|
Compound Segment |
|
|
|
|
|
|
|
|
Claim Billing/Claim |
|
|
|
|
|
Segment Identification |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
“1Ø” |
|
|
|
|
|
|
|
|
|
|
Field # |
|
NCPDP Field Name |
|
|
Value |
|
|
Payer |
Payer Situation |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
Usage |
|
|
|
|
COMPOUND DOSAGE FORM |
|
|
|
|
|
M |
|
|||||
|
|
|
DESCRIPTION CODE |
|
|
|
|
|
|
|
|
|||
|
|
COMPOUND DISPENSING UNIT |
|
|
|
|
|
M |
|
|||||
|
|
|
FORM INDICATOR |
|
|
|
|
|
|
|
|
|||
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
9

|
|
COMPOUND INGREDIENT |
Maximum 25 ingredients |
M |
|
|
|
|
|
|
COMPONENT COUNT |
|
|
|
|
|
|
COMPOUND PRODUCT ID |
03 - NDC |
M |
|
|
|
|
|
|
QUALIFIER |
|
|
|
|
|
|
COMPOUND PRODUCT ID |
11 digit NDC |
M |
|
|
|
|
|
COMPOUND INGREDIENT QUANTITY |
|
M |
|
|
|
|
|
COMPOUND INGREDIENT DRUG |
|
R |
Imp Guide: Required if needed for |
||
|
|
|
COST |
|
|
receiver claim determination when |
|
|
|
|
|
|
|
multiple products are billed. |
|
|
|
COMPOUND INGREDIENT BASIS OF |
|
R |
Imp Guide: Required if needed for |
||
|
|
|
COST DETERMINATION |
|
|
receiver claim determination when |
|
|
|
|
|
|
|
multiple products are billed. |
|
|
|
|
|
|
|||
|
|
|
** End of Request Claim Billing/Claim |
|
|||
“Materials Reproduced With the Consent of
©National Council for Prescription Drug Programs, Inc.
2Ø1Ø NCPDP”
Patient Choice & Therapy First & Therapy First Plus D.0 Claim Billing And Response Payer Sheet 20111017.Docx
10
Form Characteristics
| Fact Name | Description |
|---|---|
| Payer Information | The coupon form is designed for three specific programs: Patient Choice, Therapy First, and Therapy First Plus. Each program shares the same BIN and PCN codes. |
| Contact Information | The form lists a contact number (800-422-5604) for both participant inquiries and pharmacy help desk assistance. |
| Transaction Codes | Supported transactions include billing (B1), reversals (B2), and re-bills (B3). Each transaction has specific segment and field requirements. |
| Form Versions | The form uses the NCPDP Telecommunication Standard Version D.0, effective from November 17, 2011, and is supported until December 31, 2011. |
Guidelines on Utilizing Vyvanse Coupon
Completing the Vyvanse Coupon form involves several straightforward steps that ensure accurate information is provided. By following the instructions carefully, you can efficiently fill out the necessary sections of the form to process your claim. Here’s what to do:
- Gather Necessary Information: Collect all required personal information, including your insurance details and identification numbers.
- Fill in General Information: Enter the payer name, which could be "Patient Choice," "Therapy First," or "Therapy First Plus." Also, include the date, BIN number (004682), and processor control number (CN).
- Complete the Patient Segment: Include the patient's name (first and last), date of birth, gender, and address. Ensure you have the patient’s email and phone number handy, as these may be required.
- Input Claim Details: In this section, provide the transaction code (B1 or B3), prescription reference number, etc. Make sure to include any associated costs accurately in the pricing segment.
- Review Each Section: Go through the entire form to confirm that all information is complete and correct. Missing or incorrect data can delay processing.
- Submit the Form: Once you're confident everything is accurate, submit the form as instructed, whether via online portal or mailing it directly to the processing entity.
What You Should Know About This Form
What is a Vyvanse coupon form?
A Vyvanse coupon form is a document that allows patients to receive discounts or savings on their prescription for Vyvanse. These coupons are typically provided by the manufacturer or pharmacy benefits programs and can help lower out-of-pocket costs, making the medication more affordable for users.
How does one obtain a Vyvanse coupon?
Vyvanse coupons can be obtained online from the manufacturer's website or participating pharmacies. Patients can also ask their healthcare providers if they have access to any current offers. Many health insurance plans may have specific requirements or limitations regarding coupon use. Therefore, it is wise to check these details before proceeding with redemption.
Can uninsured patients use a Vyvanse coupon?
Yes, uninsured patients can often use a Vyvanse coupon to receive discounts. These coupons are designed to provide financial relief regardless of insurance status. However, patients should always confirm with the pharmacy that they will accept the coupon before making a purchase.
Do Vyvanse coupons expire?
Most Vyvanse coupons have an expiration date clearly printed on them. Patients should pay attention to this date to ensure that they use the coupon before it becomes invalid. If the expiration date has passed, it is recommended to look for any new coupons or promotional offers that may be available.
Is there any limit to how many times a coupon can be used?
Often, the use of a Vyvanse coupon is limited to one per transaction or per prescription. Some coupons may only be used a certain number of times during a given year. The specific terms and conditions will be outlined on the coupon, so careful review is essential to avoid any misconceptions.
Can I use a Vyvanse coupon with my insurance?
In many cases, patients may be able to use a Vyvanse coupon alongside their insurance. However, certain insurance plans may have policies that limit this option. It is advisable to consult with both the pharmacy and the insurance provider to confirm whether combining a coupon with your insurance is feasible.
What information is required to use the Vyvanse coupon?
Using a Vyvanse coupon typically requires basic patient information, including the patient's name, prescription details, and possibly the cardholder ID associated with insurance plans when applicable. Each pharmacy may have slightly different requirements, so it’s wise to be prepared with all necessary information at the time of redemption.
What if my pharmacy does not accept the Vyvanse coupon?
If a pharmacy refuses to accept a Vyvanse coupon, patients should first inquire about the reason for the refusal. It might be due to specific pharmacy policies or insurance restrictions. If the problem persists, contacting the coupon’s provider or the manufacturer for assistance may be an advantageous step.
Are there any alternative savings options available for Vyvanse?
Yes, besides coupons, patients can explore patient assistance programs offered by the manufacturer, which may provide further discounts or access to free medication for those in financial need. Additionally, discussing alternative therapies or generic medications with a healthcare provider might also lead to substantial savings.
Common mistakes
Completing the Vyvanse coupon form can be a straightforward task, but small errors can lead to significant delays in processing or even rejection of claims. One of the most common mistakes is leaving out mandatory fields. Each section of the form has specific fields that must be filled out, such as the BIN number and the transaction code. Omitting these required fields results in processing issues, potentially leaving the patient without their medication.
Another frequent error is providing incorrect information in the patient section. It's vital to ensure that the patient’s full name, date of birth, and gender are filled out accurately. Inaccuracies can arise from simple typos or incorrect entries, leading to mismatches in the patient’s file. Such discrepancies may lead pharmacies to deny claims or require additional documentation, leading to delays.
Additionally, individuals often overlook the necessity of the patient's insurance details. Entering the correct group ID and cardholder ID is essential. Forgetting these can create confusion for pharmacies when verifying eligibility for discounts or benefits. In some cases, pharmacies may refuse to process the coupon due to missing insurance information.
Many people also fail to double-check the medication details outlined in the claim segment. Ensuring the correct prescription reference number and the proper National Drug Code (NDC) for Vyvanse is crucial. Entering an incorrect digit or an outdated code can lead to denied claims, significantly complicating the process for everyone involved.
Another overlooked aspect is the submission of supporting documents. If the form requests documentation like prior authorization, failing to include it can lead to rejection. Always review the requirements and submit any necessary paperwork alongside the form to ensure timely processing.
Picking the right transaction code is also a common stumbling block. Users may either mistakenly select the wrong code or misunderstand the codes’ meanings. Understanding whether to use B1 (billing) or B3 (re-bill) is essential for the proper processing of the claim. Selecting the incorrect code can trigger additional processing times as the pharmacy sorts through the error.
Furthermore, individuals often misinterpret the situational fields and neglect to provide relevant information. Certain fields may be marked as optional, yet they can be critical depending on the specific situation. If the payer requires a field that was marked as optional when additional coverage exists, it could lead to payment delays.
Reviewing the total amounts submitted is crucial. Mistakes in reporting the ingredient cost, dispensing fee, or patient-paid amount can lead to confusion and incorrect billing. Ensuring that all figures are accurate not only eases processing but assists in avoiding potential disputes with insurance providers.
Lastly, a common yet easily avoidable error is failing to sign or date the form where indicated. A missing signature may seem trivial, yet it can halt the processing entirely. Always complete the form thoroughly, paying attention to every detail, including signatures.
By avoiding these common mistakes, individuals can streamline the process of using Vyvanse coupons and access their medications more swiftly. A careful review of the completed form may make all the difference in ensuring a smooth transaction.
Documents used along the form
The Vyvanse Coupon form is often used in conjunction with other essential documents to ensure smooth processing of prescription claims. These forms help clarify billing procedures, patient information, and eligibility, among other critical aspects. Understanding these documents can enhance your experience when dealing with insurance matters related to Vyvanse.
- Prescription Form: This document is filled out by the prescribing physician. It contains essential details such as the patient's name, medication dosage, frequency, and duration of treatment. A valid prescription is necessary for pharmacies to dispense Vyvanse.
- Patient Insurance Card: The insurance card provides proof of coverage and helps the pharmacy verify the patient's insurance details. It typically displays the patient's ID number, group number, and other relevant information needed for billing and reimbursement.
- Prior Authorization Request: This form may be required by the insurance company before the medication is covered. It documents the medical necessity of Vyvanse for treating the patient's condition and must be submitted by the prescribing physician or pharmacy.
- Medication History Form: This document collects information about the patient's previous prescriptions and treatments. It aids healthcare providers and pharmacists in understanding the patient's medical history, ensuring safe and effective medication management.
Each of these documents plays a crucial role in ensuring a seamless process from prescription to coverage approval. Be sure to have them ready for quick reference when dealing with your Vyvanse prescription.
Similar forms
-
Health Insurance Claim Form (CMS-1500): Like the Vyvanse Coupon form, the CMS-1500 is used to submit claims for reimbursement of medical services. Both forms require detailed information about the patient, including identifiers such as names, addresses, and insurance details. Each must be filled out accurately to ensure proper processing and payment for medical treatments.
-
Prescription Drug Claim Form: This document serves a similar purpose to the Vyvanse Coupon form in that it allows patients to submit claims for prescription medications. Users must include the medication name, the prescribing physician's information, and patient insurance details, reflecting the same need for specificity as in the Vyvanse form.
-
Prior Authorization Request Form: Both this form and the Vyvanse Coupon form may require detailed patient information to obtain required approvals from insurance before medication can be dispensed. Accurate data must be shared, and both documents aim to facilitate important communication between healthcare providers and payers.
-
Pharmacy Benefit Manager (PBM) Claim Form: Much like the Vyvanse Coupon form, PBM claim forms are used when processing prescription drug claims through insurance. Each form requires similar information about the patient, the drug prescribed, and the provider, highlighting the necessity for precise record-keeping in medication management.
Dos and Don'ts
When filling out the Vyvanse Coupon form, it is crucial to ensure accuracy and completeness. Here are seven key actions to keep in mind:
- Do double-check all information before submitting the form.
- Don't leave any mandatory fields blank; ensure each required section is filled out completely.
- Do include the correct BIN and PCN numbers as indicated on the payer sheet.
- Don't use outdated versions of the form; always use the most recent version provided.
- Do verify patient information, such as date of birth and contact details, to avoid processing delays.
- Don't overlook optional fields that may require additional documentation; provide what can enhance the claim.
- Do contact the pharmacy help desk if you have questions about how to complete any section.
Following these guidelines can improve the likelihood of a smooth and efficient processing of your Vyvanse Coupon form.
Misconceptions
Misconceptions about the Vyvanse coupon form can lead to confusion and misinterpretation. Here are some common misconceptions clarified:
- The Vyvanse coupon form is only for those with insurance. This is incorrect. The coupon can also benefit individuals without insurance by providing discounts on their prescriptions.
- Coupons provide unlimited use. This is a misconception. Coupons typically have limits on usage, often specified on the form itself.
- You can use the coupon for any prescription medication. This is false. The coupon specifically applies to Vyvanse and is not valid for other medications.
- All pharmacies accept the Vyvanse coupon. Not every pharmacy will accept the coupon. It is essential to verify with the pharmacy first.
- Using a coupon means you have to forgo insurance benefits. This is misleading. In some cases, the coupon can be used alongside insurance to reduce out-of-pocket costs, but this varies by plan.
- The coupon will always result in the lowest price. This is not necessarily true. Sometimes, insurance co-pays can be lower than the coupon price, so it’s wise to compare.
- Applying for the coupon is too complicated. Some believe this, but in reality, the application process is often straightforward and user-friendly.
- The coupon is only valid for a limited time after issuance. While coupons have expiration dates, many are renewed periodically, so it’s worth checking if a new one is available.
Key takeaways
When utilizing the Vyvanse Coupon form, it is essential to keep certain points in mind to ensure successful processing. Below are key takeaways to consider:
- Payer Information: Familiarize yourself with the payer details listed on the coupon, including the payer name and Group Name.
- Bin and PCN Numbers: Provide the appropriate BIN (004682) and PCN (CN) as required for verification.
- Transaction Codes: Understand that the coupon supports multiple transaction codes, specifically B1 (Billing) and B3 (Re-bill).
- Mandatory Fields: Ensure all mandatory fields indicated by "M" are filled out accurately. This includes the BIN number, version/release number, transaction code, and processor control number.
- Service Provider Information: Enter the NPI (National Provider Identifier) of the service provider to facilitate the claim submission.
- Patient Details: Include the patient's first name, last name, date of birth, and contact information, as these are necessary for processing.
- Date of Service: Provide the date when the services were rendered. This is a mandatory requirement.
- Quantity Dispensed: Accurately report the quantity dispensed in the appropriate field, as this can affect the claim's outcome.
- Prior Authorization: If applicable, include a prior authorization number; this can determine how the claim is handled.
- Other Coverage Information: Disclose any other insurance coverage that might apply, as this could influence how the claim is processed.
Reviewing these takeaways can aid in the proper completion and use of the Vyvanse Coupon form, ensuring that all necessary information is provided for claim processing.
Browse Other Templates
California Corporation - The restated articles replace the original articles in their entirety.
Home Health Forms - Applicants must be aware that not all historical data may be available in their records.