Fill Out Your Wellcare Prior Authorization Form
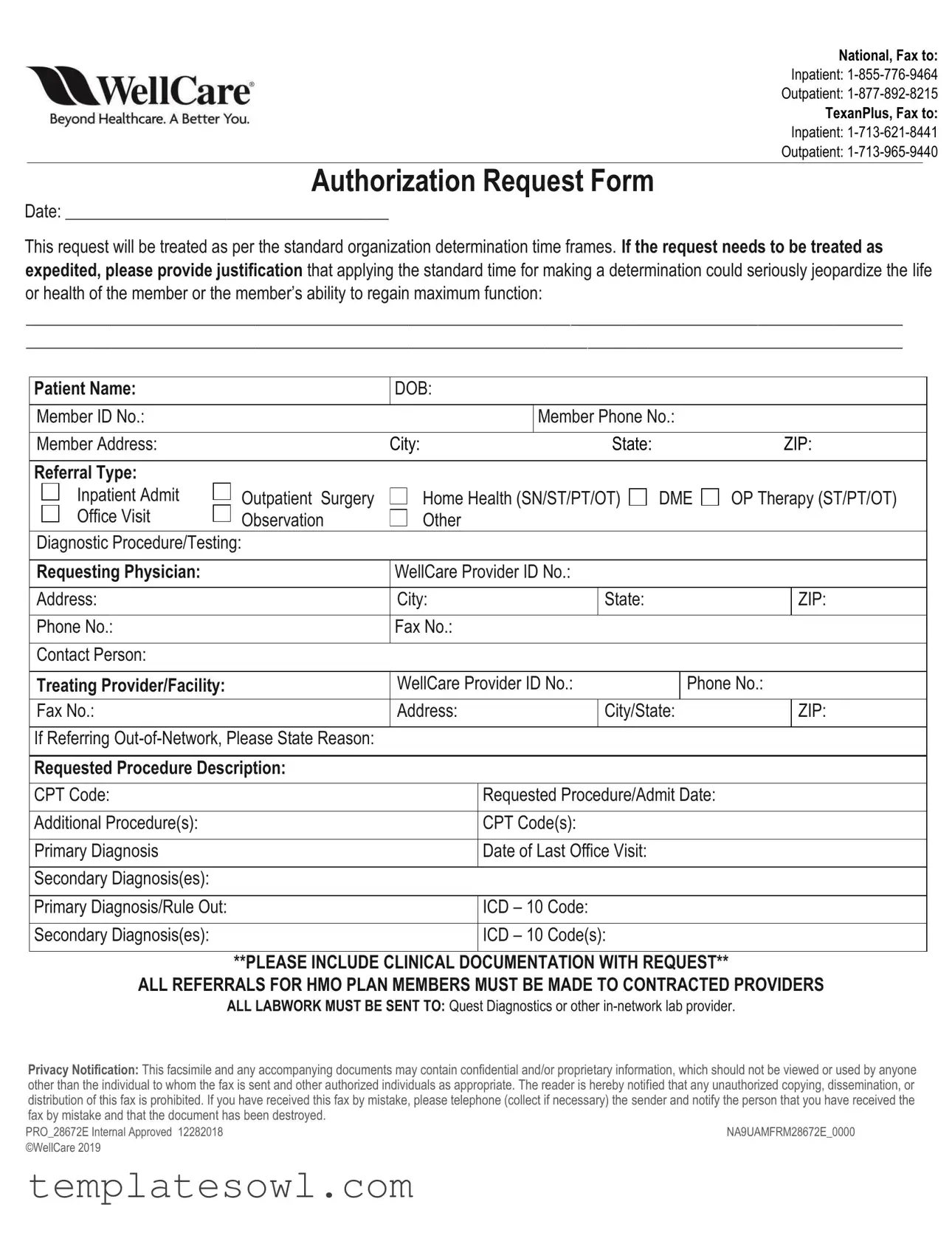
The Wellcare Prior Authorization form is vital for healthcare providers seeking approval for specific medical services and procedures for their patients. This form ensures that requests for inpatient and outpatient services, such as surgeries, home health care, and diagnostic testing, meet Wellcare's criteria for authorization. Key components of the form include the patient’s personal information, including their name, date of birth, and member ID, as well as details regarding the requested procedure and relevant diagnosis codes. The requesting physician's credentials and contact information also play a significant role in the process. To expedite approval, it is crucial to provide justification if the standard authorization timeframe is not applicable due to urgent health concerns. The form also emphasizes the requirement of including clinical documentation to support the request. Additionally, healthcare providers must ensure that referrals are made to contracted providers within the HMO plan and that all necessary lab work is directed to in-network options. Lastly, the form incorporates a confidentiality notice, highlighting the importance of protecting sensitive patient information during the submission process.
Wellcare Prior Authorization Example

National, Fax to:
Inpatient:
Outpatient:
TexanPlus, Fax to:
Inpatient:
Outpatient:
Authorization Request Form
Date: ______________________________________
This request will be treated as per the standard organization determination time frames. If the request needs to be treated as expedited, please provide justification that applying the standard time for making a determination could seriously jeopardize the life or health of the member or the member’s ability to regain maximum function:
_______________________________________________________________________________________________________
_______________________________________________________________________________________________________
Patient Name: |
DOB: |
|
|
|
|
|
|
Member ID No.: |
|
Member Phone No.: |
|
|
|
|
|
Member Address: |
City: |
State: |
ZIP: |
|
|
|
|
Referral Type: |
|
|
|
Inpatient Admit Office Visit
Outpatient Surgery Observation
Home Health (SN/ST/PT/OT) Other
DME
OP Therapy (ST/PT/OT)
Diagnostic Procedure/Testing:
Requesting Physician: |
WellCare Provider ID No.: |
|
|
||
|
|
|
|
|
|
Address: |
City: |
|
State: |
|
ZIP: |
|
|
|
|
|
|
Phone No.: |
Fax No.: |
|
|
|
|
|
|
|
|
|
|
Contact Person: |
|
|
|
|
|
|
|
|
|
||
Treating Provider/Facility: |
WellCare Provider ID No.: |
Phone No.: |
|||
|
|
|
|
|
|
Fax No.: |
Address: |
|
City/State: |
|
ZIP: |
|
|
|
|
|
|
If Referring |
|
|
|
|
|
|
|
|
|
|
|
Requested Procedure Description: |
|
|
|
|
|
|
|
|
|||
CPT Code: |
|
Requested Procedure/Admit Date: |
|||
|
|
|
|
|
|
Additional Procedure(s): |
|
CPT Code(s): |
|
|
|
|
|
|
|
|
|
Primary Diagnosis |
|
Date of Last Office Visit: |
|
|
|
|
|
|
|
|
|
Secondary Diagnosis(es): |
|
|
|
|
|
|
|
|
|
|
|
Primary Diagnosis/Rule Out: |
|
ICD – 10 Code: |
|
|
|
|
|
|
|
|
|
Secondary Diagnosis(es): |
|
ICD – 10 Code(s): |
|
|
|
**PLEASE INCLUDE CLINICAL DOCUMENTATION WITH REQUEST**
ALL REFERRALS FOR HMO PLAN MEMBERS MUST BE MADE TO CONTRACTED PROVIDERS
ALL LABWORK MUST BE SENT TO: Quest Diagnostics or other
Privacy Notification: This facsimile and any accompanying documents may contain confidential and/or proprietary information, which should not be viewed or used by anyone other than the individual to whom the fax is sent and other authorized individuals as appropriate. The reader is hereby notified that any unauthorized copying, dissemination, or distribution of this fax is prohibited. If you have received this fax by mistake, please telephone (collect if necessary) the sender and notify the person that you have received the fax by mistake and that the document has been destroyed.
PRO_28672E Internal Approved 12282018 |
NA9UAMFRM28672E_0000 |
©WellCare 2019 |
|
Form Characteristics
| Fact Name | Details |
|---|---|
| Authorization Request Submission | The Wellcare Prior Authorization form must be completed and submitted to the appropriate fax number based on the referral type. |
| Fax Numbers | For national submissions, use 1-855-776-9464 for inpatient and 1-877-892-8215 for outpatient requests. |
| TexanPlus Submission | For TexanPlus, fax inpatient requests to 1-713-621-8441 and outpatient requests to 1-713-965-9440. |
| Expedited Requests | Requests may be treated as expedited if justification shows that standard time frames could jeopardize the member’s health. |
| Clinical Documentation Requirement | It is essential to include clinical documentation with each prior authorization request. |
| Confidentiality Notification | The form contains confidentiality notices indicating that unauthorized use or distribution is prohibited. |
Guidelines on Utilizing Wellcare Prior Authorization
Filling out the Wellcare Prior Authorization form requires careful attention to detail. This form is crucial for ensuring that necessary medical procedures receive timely approval. Following these steps will help streamline the process and ensure that all required information is included.
- Begin by noting the date at the top of the form.
- Identify the patient’s information by entering the patient's name, date of birth, member ID number, phone number, and address, including city, state, and ZIP code.
- Specify the referral type by selecting from the options provided, such as inpatient admission, office visit, outpatient surgery, and others as applicable.
- Provide details about the requesting physician, including their WellCare Provider ID number, address, city, state, ZIP code, phone number, and fax number.
- If applicable, fill out the information for the treating provider or facility, including their WellCare Provider ID number, phone number, fax number, and address.
- For any out-of-network referrals, include a reason for the referral.
- Describe the requested procedure and note the corresponding CPT code.
- Indicate the requested procedure or admission date along with any additional procedures and their CPT codes.
- Complete the diagnosis section by providing the primary diagnosis, the date of the last office visit, any secondary diagnoses, and the relevant ICD-10 codes.
- Attach clinical documentation to this request to support the prior authorization.
- Remember that for HMO plan members, referrals must be directed to contracted providers.
- Ensure that all lab work is sent to Quest Diagnostics or another in-network lab provider.
- Once completed, fax the form to the appropriate number based on the patient's plan type.
Once the form is submitted, it will be reviewed as per the organization’s standard time frames. If expedited processing is necessary, include a justification within the submission. Always keep copies for your records.
What You Should Know About This Form
What is the Wellcare Prior Authorization form used for?
The Wellcare Prior Authorization form is a request used by healthcare providers to obtain approval before certain medical services or procedures are provided to patients. This form helps ensure that the treatments or services are covered by the patient's health plan. It is essential for both inpatient and outpatient procedures, including surgeries, therapies, and diagnostic tests.
How should I submit the Wellcare Prior Authorization form?
You can submit the Wellcare Prior Authorization form via fax. The fax number depends on the type of authorization needed. For inpatient requests, send the form to 1-855-776-9464 for National members, or 1-713-621-8441 for TexanPlus members. For outpatient requests, the fax number is 1-877-892-8215 for National members, and 1-713-965-9440 for TexanPlus members.
What information is required on the form?
Several important details must be included on the Wellcare Prior Authorization form. You need to provide the patient's name, date of birth, member ID number, and contact information. Additionally, you’ll need to specify the type of referral, describe the requested procedure, include relevant diagnosis codes, and provide information about the requesting physician as well as the treating provider or facility. Clinical documentation should also accompany the request.
What happens if the request is expedited?
If the authorization request is urgent and must be expedited, it is necessary to provide justification in the appropriate section of the form. This justification should explain how following the standard timeframe could seriously affect the member's health or ability to recover. The organization will review the request under expedited guidelines if the justification meets their criteria.
What are the privacy considerations when faxing the form?
This form and any attached documents may contain confidential information. It is important that only the intended recipient views or uses this information. If the fax is received by someone who is not the intended recipient, they are advised to notify the sender immediately and destroy the document. Unauthorized copying and distribution are prohibited.
What if I need to use out-of-network providers?
If you are referring a patient to an out-of-network provider, you must state the reason on the form. This helps Wellcare understand the necessity of using a provider outside their network and allows for appropriate consideration of your request. Remember that all referrals for HMO plan members must go to contracted providers, unless justified otherwise.
Common mistakes
Filling out the Wellcare Prior Authorization form requires careful attention to detail. One common mistake is failing to complete the patient information section thoroughly. Missing information such as the patient’s name, date of birth, or member ID can lead to delays in processing the request. Ensure that all applicable fields are filled out completely.
Another error occurs when individuals do not provide a justification for expedited requests. If a request is urgent, it is essential to explain in writing how waiting for the standard determination period may negatively affect the patient’s health. Without this justification, the request may not be prioritized as needed.
Incorrectly identifying the referral type can complicate the authorization process. It is crucial to select the appropriate type of referral, such as inpatient admission or outpatient surgery. Misclassification can result in the request being sent to the wrong department, causing significant delays.
Omitting clinical documentation is another significant mistake. The form explicitly states the necessity of including clinical information to support the request. Failing to do so can lead to an outright denial of the authorization. Always ensure that all relevant documentation accompanies the request.
Many make the mistake of not providing the correct CPT and ICD-10 codes. These codes are essential for indicating the requested procedure and diagnoses clearly. Ensuring these codes are accurate and up-to-date will help prevent complications during the review process.
Another frequent error is not mentioning the treating provider or facility's information. This section requires complete details, including name, address, and contact numbers. Missing or incorrect information here can lead to unnecessary follow-ups and delays.
Submitting the form without confirming that the requesting physician is in-network can also add complications. For HMO plans, referrals must be made to contracted providers. Failure to verify network status can result in denials and further confusion.
Some individuals neglect to thoroughly review any additional notes or instructions provided on the form. This can include policies regarding lab work or specific documentation requirements. Ignoring these instructions may lead to misunderstandings and increased processing time.
Lastly, forgetting to sign or date the authorization request is a common yet critical oversight. A missing signature invalidates the entire submission. Always ensure that the form is signed and dated before sending it to the appropriate fax number.
Documents used along the form
When submitting the Wellcare Prior Authorization form, several additional documents may be required to support the request. Each of these documents plays a critical role in ensuring timely and effective approvals for patient care. Below is a list of commonly used forms alongside the Prior Authorization request.
- Clinical Documentation: This includes medical records, progress notes, and any relevant test results that help substantiate the necessity of the requested service or procedure.
- Referral Form: Often required when referring a patient to a specialist. It outlines the reason for the referral and any preliminary evaluations performed.
- Patient Consent Form: This document confirms that the patient understands and agrees to the proposed treatment or procedure, ensuring informed consent.
- Insurance Verification Form: This verifies the patient's insurance coverage and benefits to ensure that the requested services are authorized under their plan.
- Prescriptions: Copies of any relevant prescriptions may be needed to provide context for the request, especially for medications related to the procedure.
- Diagnostic Test Results: This includes results from labs or imaging studies that support the medical necessity of the requested service.
- History and Physical (H&P) Report: An H&P report outlines the patient’s medical history and examination findings, providing a comprehensive overview of their health status.
- Letter of Medical Necessity: A letter from the physician detailing why the requested service or procedure is critical to the patient's health and treatment plan.
- Benefit Interpretation Letter: This document helps clarify coverage issues, highlighting any special considerations or exceptions that may apply to the patient’s insurance policy.
- Additional Authorization Forms: Depending on the service type, other specific authorization documents may be needed for procedures like imaging studies or surgical interventions.
Collecting and submitting the right documents can significantly impact the process of securing authorization. Staying organized and thorough will help facilitate a smoother approval process for necessary medical services.
Similar forms
- Medicare Prior Authorization Request Form: This document is utilized by Medicare providers to request authorization for specific services. It follows similar guidelines and requires details about the patient, procedure, diagnosis, and supporting clinical documentation.
- Medicaid Authorization Request Form: Providers use this form when seeking approval for services covered by Medicaid. Like the Wellcare form, it requests identifying information, procedure details, and justification for medical necessity.
- Commercial Insurance Authorization Form: This document serves to obtain pre-approval from private insurance companies. It includes data about the patient, treatment plan, and rationale for the requested service, mirroring the structure of the Wellcare form.
- Inpatient Admission Authorization Form: Frequently used for hospital admissions, this form requires patient and admission details, similar to the Wellcare Prior Authorization form. It emphasizes urgency and necessity for inpatient care.
- Outpatient Service Authorization Form: This form is specific to outpatient procedures and services. It requests patient information, procedure description, and clinical justification, aligning closely with the information required on the Wellcare form.
- Durable Medical Equipment (DME) Authorization Form: Providers submit this form to obtain authorization for medical equipment. It shares commonalities with the Wellcare form, focusing on patient identity, equipment requested, and medical necessity documentation.
Dos and Don'ts
When filling out the Wellcare Prior Authorization form, attention to detail is crucial. Here are nine key points to consider:
- Do ensure that all required fields are completed accurately, including patient information and requested procedures.
- Do provide clinical documentation to support the authorization request, as specified in the form.
- Do verify that you are using the appropriate fax number for inpatient or outpatient requests based on your needs.
- Do include the correct CPT and ICD-10 codes; this helps to avoid delays in processing.
- Do keep a copy of the completed form and any accompanying documents for your records.
- Don't submit the request without justification if you mark it as expedited.
- Don't forget to check that all provider information is current and complete, including phone and fax numbers.
- Don't assume that sending the form without additional documentation will guarantee approval.
- Don't send lab work to an out-of-network provider, as all lab work must go to Quest Diagnostics or another in-network lab.
Following these guidelines can significantly streamline the authorization process and enhance the chances of a favorable outcome.
Misconceptions
Misconceptions about the Wellcare Prior Authorization form can lead to confusion and complications in the healthcare process. Here are nine common misunderstandings, along with clarifications for each.
- Prior Authorization Is Always Required for All Services: Many people believe that prior authorization is necessary for every medical service. In reality, it often applies only to specific procedures or services, depending on the insurance plan.
- The Process Is Instant: Some assume that submitting a prior authorization form automatically results in immediate approval. The determination can take time and is subject to standard processing periods unless marked urgent.
- Any Doctor Can Submit the Request: Some patients think any doctor can file the prior authorization. However, generally, it must be submitted by a provider in-network with Wellcare or specifically designated contacts.
- Clinical Documentation Isn’t Necessary: There is a common belief that additional documents are optional. In fact, submitting clinical documentation with the request is essential to support the need for the service.
- Faxing the Form Guarantees It Will Be Received: Many believe that faxing the authorization form ensures receipt. However, transmission can fail, so it’s wise to confirm with the Wellcare contact person.
- All Referrals Go Through Wellcare: People often think all referral requests are handled by Wellcare. Referrals must go to contracted providers and may not always involve Wellcare directly.
- The Same Form Is Used for Inpatient and Outpatient Services: Some assume one form suffices for all services. Each type of service—whether inpatient, outpatient, or others—may require different forms or additional information.
- All Lab Work Can Be Sent Anywhere: There’s a misconception that lab work can be submitted to any lab. However, lab tests must be sent to specific in-network providers like Quest Diagnostics.
- Expedited Requests Are Handled Quickly: While expedited requests are meant for urgent situations, not all are approved quickly. Justification must be compelling, and the approval process can still take time.
Understanding these points can help streamline the submission and approval process for prior authorizations. Being informed reduces delays and ensures better patient care.
Key takeaways
Understanding the Wellcare Prior Authorization form is essential for streamlined healthcare processes. Here are some key takeaways to consider:
- Be Thorough: Complete every section of the form accurately. Missing or incorrect information can delay the approval process.
- Choose the Right Fax Number: Ensure you are faxing to the correct number based on whether the request is inpatient or outpatient. Different fax numbers are provided for TexanPlus and National members.
- Expedited Requests: If a request is urgent, provide a justification. Clearly explain how the delay could impact the patient’s health.
- Include Clinical Documentation: Always attach relevant clinical documents. These help support the medical necessity of the requested services.
- Utilize the Correct Provider ID: Make sure to insert the WellCare Provider ID number for both the requesting and treating providers.
- Lab Work Protocols: Remember that all lab work must go to in-network providers, such as Quest Diagnostics.
- Member Information: Double-check the patient’s details, including name, DOB, and member ID number. Any inaccuracies might result in processing delays.
- Confidentiality Matters: Handle the fax with care. The information contained is confidential and should only be viewed by authorized individuals.
Taking these steps can enhance the likelihood of timely approvals and ensure that patients receive the care they need promptly. By being proactive and careful with the form, you contribute to a smoother healthcare experience.
Browse Other Templates
Tc-810 - Owners must navigate local health department regulations as outlined in the guidance associated with the TC-810.
How to Fight a Ticket in Michigan - Your cooperation helps maintain an efficient appeal process for all parties involved.