Fill Out Your Workers Compensation C 4 Form
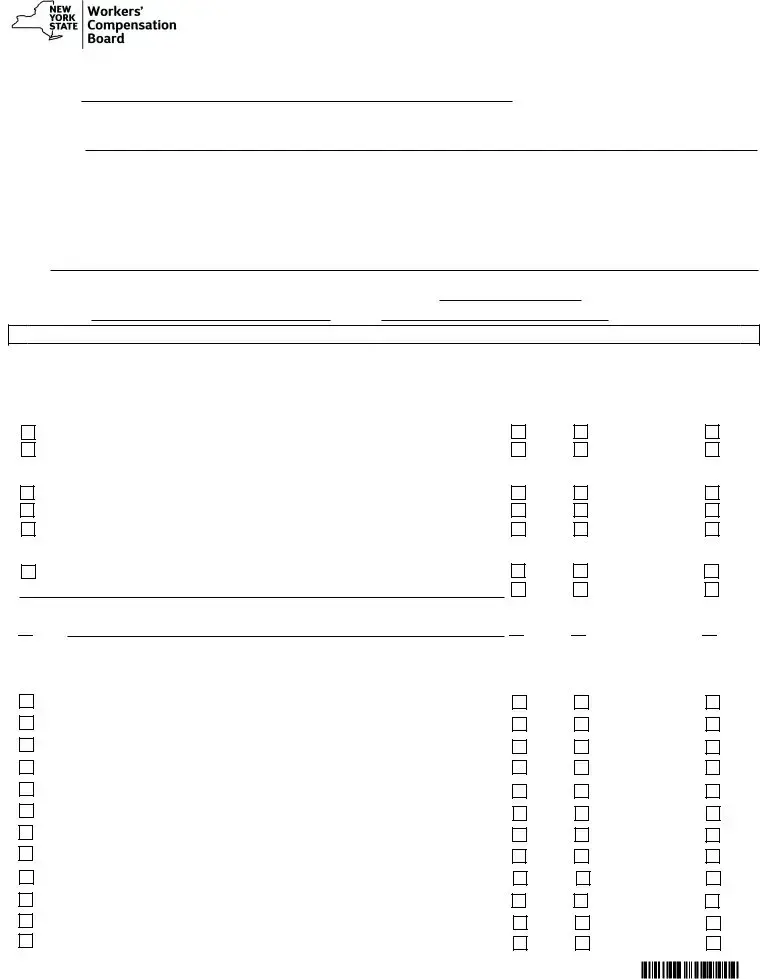
The Workers Compensation C-4 form plays a crucial role in the process of obtaining medical treatment for injured workers. Used primarily to request written authorization for special services that exceed $1,000, it ensures that necessary medical treatments align with established Medical Treatment Guidelines. The form prompts healthcare providers to furnish critical information, including patient details, injury specifics, and the requested services. Authorized signatures from attending doctors confirm the legitimacy of the request. Additionally, the form includes sections for insurers to respond, detailing whether a request is granted, denied, or granted without prejudice. Providers must be precise; any omission can lead to delays or denials of crucial treatments. The form emphasizes a clear communication channel with insurers and outlines response timelines to maintain accountability. Ultimately, navigating this form effectively is vital for accessing timely care for injured workers, balancing both their rights and the insurer's requirements.
Workers Compensation C 4 Example

IMPORTANT:
PLEASE READ CAREFULLY THE FOLLOWING INFORMATION FOR DETERMINING HOW TO FIND
A.
|
|
|
|
ATTENDING DOCTOR'S REQUEST FOR |
|
|||||
|
|
|
|
AUTHORIZATION AND INSURER'S RESPONSE |
|
|||||
|
|
|
|
|
Answer all questions fully on this report |
|
|
|
AUTH |
|
WCB Case #: |
|
Claim Administrator Claim (Carrier Case) #: |
|
Date of Injury/Illness: |
||||||
|
|
|
|
|
|
|
|
|
||
Patient's Name: |
First |
MI |
Last |
Social Security No.: |
||||||
Address: |
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
||
Employer Name: |
Number and Street |
|
City |
State |
Zip Code |
|||||
|
|
|
|
|
|
|
|
|
||
Address:
|
|
|
Number and Street |
City |
State |
Zip Code |
|
|
Insurer Name: |
|
|
|
|
||
|
Address: |
|
|
|
|||
B. |
|
|
Number and Street |
City |
State |
Zip Code |
|
Attending Doctor's Name: |
|
|
|
|
|||
|
Address: |
|
|
|
|||
Number and Street |
City |
||||||||||||||
Individual Provider's WCB Authorization No.: |
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
Telephone No.: |
|
|
|
|
|
|
|
|
|
|
|
Fax No.: |
|||
State |
Zip Code |
NPI No.:
C.
AUTHORIZATION REQUEST
The undersigned requests written authorization for the following special service(s) costing over $1,000 or requiring
Authorization Requested: |
|
|
|
|
|
|
|
|
Insurer Response: if any service |
|
|
||||
Diagnostic Tests: |
|
|
|
|
|
|
|
|
is denied, explain on reverse. |
|
|
||||
|
|
|
|
|
|
|
|
Granted |
Granted w/o Prejudice |
Denied |
|||||
Radiology Services |
|
|
|
||||||||||||
Other |
|
|
|
|
|
|
|
|
|
Granted |
Granted w/o Prejudice |
Denied |
|||
Therapy (including Post Operative): |
|
|
|
|
|
|
|
|
|
|
|
|
|||
Physical Therapy: |
|
|
times per week for |
weeks |
Granted |
Granted w/o Prejudice |
Denied |
||||||||
|
|
|
|
|
|
|
|
Granted |
Granted w/o Prejudice |
Denied |
|||||
Occupational Therapy: |
|
|
times per week for |
weeks |
|||||||||||
Other |
|
|
|
|
|
|
|
|
|
|
Granted |
Granted w/o Prejudice |
Denied |
||
Surgery: |
|
|
|
|
|
|
|
|
|
|
|
|
|||
Type of Surgery (Describe, include use of hardware/surgical implants) |
|
|
|
Granted |
Granted w/o Prejudice |
Denied |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Granted |
Granted w/o Prejudice |
Denied |
|
Treatment:

 Other
Other  Granted
Granted 
 Granted w/o Prejudice
Granted w/o Prejudice  Denied
Denied
Medical Treatment Guidelines Procedures Requiring
1. |
Lumbar Fusions |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1. |
|||
|
B |
|
- |
|
E |
|
4 |
|
a |
|
|
|
|
|
|
|
............................................................................. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
2. Artificial Disk Replacement |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
|||||||||||
|
|
|
|
|
|
- |
|
|
|
|
E |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
........................................................... |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
3. |
Vertebroplasty |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
||
|
|
B |
|
- |
E |
|
7 |
|
|
a |
|
|
|
|
|
i |
|
|
................................................................................ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
4. Kyphoplasty |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4. |
|||||||
B |
|
- |
|
E |
|
7 |
|
a |
|
|
i |
|
|
.................................................................................... |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
5. |
Electrical Bone Growth Stimulators |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5. |
|||||||||||||||||||||
|
|
|
|
|
|
- |
|
|
E |
|
|
|
|
|
a |
|
|
|
|
|
|
............................................... |
|
|
|
|
|
|
|||||||||||||||||||||||||||
6. |
Osteochondral Autograft |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6. |
|||||||||||||
|
K |
- |
|
D |
|
1 |
|
|
|
|
f |
|
|
|
|
|
................................................................ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
7. Autologous Chondrocyte Implantation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
7. |
||||||||||||||||||||||||||||
|
|
|
K |
- |
|
D |
|
1 |
|
f |
|
|
|
|
|
|
|
............................................. |
|
|
|
|
|||||||||||||||||||||||||||||||||
8. Meniscal Allograft Transplantation |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
................................................. |
|
|
|
|
|
|
8. |
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
K |
- |
|
D |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||
9. Knee Arthroplasty (total or partial knee joint replacement) |
|
|
|
|
|
|
|
|
|
|
9. |
||||||||||||||||||||||||||||||||||||||||||||
|
|
|
K |
- |
F |
2 |
|
|
|||||||||||||||||||||||||||||||||||||||||||||||
10. Spinal Cord Stimulators |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10. |
||||||||||
|
P |
|
- |
|
|
G |
|
1 |
|
|
|
|
|
|
|
|
|
|
|
................................................................. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
11. Intrathecal Drug Delivery (pain pumps) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
......................................... |
|
|
|
11. |
|||||||||||||||||||||||||||||
|
|
|
P |
|
|
- |
|
G |
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
12. Second or Subsequent Procedure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
................................................ |
|
|
|
|
|
|
|
12. |
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |
Granted |
Granted w/o Prejudice |
Denied |














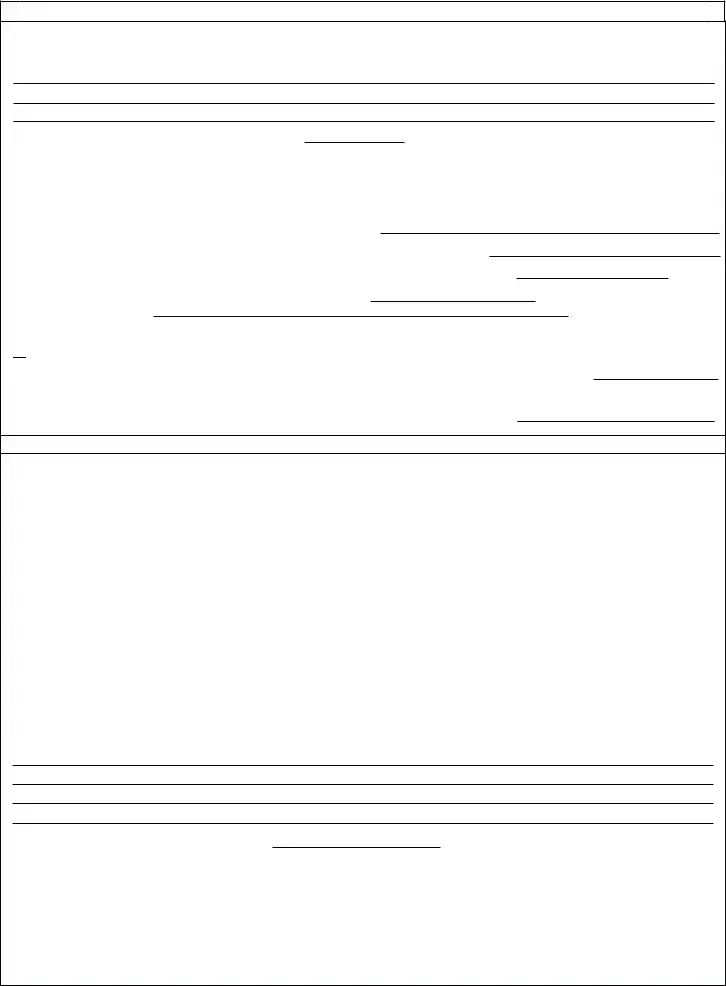
D.
STATEMENT OF MEDICAL NECESSITY
Pursuant to 12 NYCRR
Date of service of supporting medical in WCB Case File:(Attach if not already submitted.)
Pursuant to 12 NYCRR 325.1(a)(3), the treating provider shall submit this form to the Workers' Compensation Board and insurer.
Providers must complete Part A below indicating that the request was sent to the
A.Insurer's designated fax # or email address as provided on the Board's website:
B. If the request was also submitted to another fax # or email address provided by the insurer, provide here:
C.I am not equipped to send or receive forms by fax or email. This form was mailed (return receipt requested) on:
If you called the insurer and spoke with an individual, provide the date of the call: and name of person contacted:

 Designated contact information not available.
Designated contact information not available.
I certify I am making the above request for certification. This request was made to the insurance
Provider's Signature: |
|
Date: |
Response Time and Notification Required:
The
Denial of the Request for Authorization of a Special Service: A denial of authorization of a special service must be based upon and accompanied by a conflicting second opinion rendered by a physician authorized to conduct IMEs, or record review, or qualified medical professional, or a physician authorized to treat workers' compensation claimants. (If authorization is denied in a controverted case, the conflicting second opinion must address medical necessity only.) Failure to file timely the conflicting second opinion will render the denial defective. If denial of an authorization is based upon claimant's failure to attend an IME examination scheduled within the 30 day authorization period, contemporaneous supporting evidence of claimant's failure must be attached.
Failure to Timely Respond to Form
REASON FOR DENIAL(S), IF ANY. (ATTACH OR REFERENCE CONFLICTING SECOND MEDICAL OPINION AS EXPLAINED ABOVE.)
Date of service of supporting medical in WCB case file:
I certify that the
and
I certify that copies of this form were emailed, faxed, or mailed to the treating provider, the claimant (patient), the claimant's legal representative, if any, the Workers' Compensation Board and all parties of interest on the date below:
By: (print name) |
|
Title: |
||||
Signature: |
|
|
|
|
Date: |
|
www.wcb.ny.gov |
REQUEST FOR WRITTEN AUTHORIZATION
IMPORTANT TO ATTENDING DOCTOR
AUTHORIZATION FOR SPECIAL SERVICES IS NOT REQUIRED IN AN EMERGENCY
1.This form is used for a workers' compensation, volunteer firefighters' or volunteer ambulance workers' benefit case to request written authorization for special service(s) costing over $1,000 in a
2.This form must be signed by the attending doctor and must contain her/his authorization number and code letters.
3.Please ask your patient for his/her WCB case # and the claim administrator claim (carrier case) number and show these numbers on this form. In addition, ask your patient if he/she has retained a representative. If represented, ask for the name and address of the representative.
This request must be sent to the Workers' Compensation Board, and the the workers' compensation insurance carrier,
4.The attending doctor must submit this form with the Board and on the same day serve a copy on the
5.If authorization or denial is not forthcoming within 30 calendar days, (or 35 days if
6.SPECIAL SERVICES - Services for which authorization must be requested are as follows:
Physicians - To engage the services of a specialist, consultant, or a surgeon, or to provide for
Podiatrists - In treating the foot, to provide physiotherapeutic procedures,
Occupational/Physical Therapists - In treating a condition as provided in Article 136 or 156 of the Education Law, in the Workers' Compensation Law, and the Rules of the Chair relative to Occupational/Physical Therapy Practice to provide occupational/physical therapy procedures costing more than $1,000.
Psychologists - Prior authorization for procedures enumerated in section
Medical Treatment Guidelines - Lumbar Fusions, Artificial Disk Replacement, Vertebroplasty, Kyphoplasty, Electrical Bone Growth Stimulators, Spinal Cord Stimulators, Osteochondral Autograft, Autologus Chondrocyte Implantation, Meniscal Allograft Transplantation, Knee Arthroplasty (total or partial knee joint replacement), Intrathecal Drug Delivery (pain pumps).
7.If the insurer has checked "GRANTED WITHOUT PREJUDICE" in Section C, the liability for this claim has not yet been determined. This authorization is made pending final determination by the Board. Pursuant to 12 NYCRR §
8.It is the attending doctor's burden to set forth the medical necessity of the special services required. Be sure to provide this information in the Statement of Medical Necessity section of this form.
9.HIPAA NOTICE - In order to adjudicate a workers' compensation claim,
ANY PERSON WHO KNOWINGLY AND WITH INTENT TO DEFRAUD PRESENTS, CAUSES TO BE PRESENTED, OR PREPARES WITH KNOWLEDGE OR BELIEF THAT IT WILL BE PRESENTED TO OR BY AN INSURER, OR
This form must be served on the
www.wcb.ny.gov by fax, email or mailed, return receipt requested. Failure to submit the form to the designated contact identified on the Board's website may result in your request being denied. A copy of the form must also be filed with the Board.
NYS Workers' Compensation Board
PO Box 5205
Binghamton, NY
Email Filing: wcbclaimsfiling@wcb.ny.gov l |
Customer Service: (877) |
THE WORKERS' COMPENSATION BOARD EMPLOYS AND SERVES PEOPLE WITH DISABILITIES WITHOUT DISCRIMINATION |
Form Characteristics
| Fact Name | Description |
|---|---|
| Purpose | The C-4 form is used to request written authorization for special services related to workers' compensation cases. This includes services costing over $1,000 or requiring pre-authorization. |
| Necessary Signatures | This form must be signed by the attending doctor, who must also provide their authorization number and code letters. Out-of-state providers need to include their NPI number. |
| Response Time | Insurers must respond to requests within 30 days. If the C-4 is sent via regular mail, this period extends to 35 days. |
| Legal References | The C-4 form is governed by New York Workers' Compensation Law. Relevant regulations include 12 NYCRR § 325-1.4. |
| Authorization Situations | Authorization is not required in emergencies, according to the guidelines provided in the form. |
| Submission Requirements | All requests must be submitted to the insurer's designated contact, which can be found on the Workers' Compensation Board's website. |
| Denial Criteria | If a request for authorization is denied, the insurer must provide a conflicting second opinion from a qualified medical professional. |
| Consequences of Non-response | If an insurer fails to respond within the stipulated time frame, the requested treatment is automatically granted. |
Guidelines on Utilizing Workers Compensation C 4
Completing the Workers Compensation C-4 form is an important step in the process of requesting authorization for special services related to a worker's compensation claim. Once the form is properly filled out and submitted, it will be reviewed by the relevant parties, and a response will be provided based on the information presented within the form.
- Obtain the Required Information: Gather all necessary details, including the patient's name, date of injury, WCB case number, and claim administrator case number.
- Patient's Personal Information: Fill in the patient's full name and Social Security number. Add their address, including the number, street, city, state, and zip code.
- Employer Information: Input the employer's name and address, ensuring accuracy in the street, city, state, and zip code fields.
- Insurer Information: Provide the name and address of the insurer. Ensure to include the street, city, state, and zip code.
- Attending Doctor's Information: Enter the name, individual provider’s WCB authorization number, telephone number, and fax number of the attending doctor. Also, include their address and NPI number.
- Authorization Request Section: Clearly specify the special service(s) requiring authorization, such as diagnostic tests, therapy, or surgeries.
- Justification for Services: Provide a thorough explanation for the medical necessity of the requested services, which supports why the treatment is appropriate for the patient.
- Submission Details: Indicate how the form was sent (fax, email, or mail) and provide the designated fax number or email address of the insurer.
- Signature: Ensure the doctor signs and dates the form, confirming the submission and request for authorization.
- Send the Form: Submit the completed form to the appropriate parties, including the insurer and the Workers' Compensation Board.
What You Should Know About This Form
What is the purpose of the Workers Compensation C-4 form?
The Workers Compensation C-4 form is designed to request written authorization for specific medical services costing over $1,000 in non-emergency situations. This request must be made when specialized medical services are required, as outlined in the Medical Treatment Guidelines. The form should be completed by the attending physician and submitted to the insurer or self-insured employer to facilitate the approval process for necessary medical treatment.
Who needs to fill out the C-4 form?
The C-4 form must be filled out by the attending physician responsible for the patient's care. It requires the doctor's details, such as their name, contact information, and practicing credentials, in order to process the authorization request. If the patient is hospitalized, a licensed attending physician can sign the form in the place of the primary attending doctor.
How do I submit the C-4 form?
The form can be submitted by either fax, email, or regular mail, depending on the capabilities of the sending provider. It's important to identify and use the insurer's designated contact information found on the Workers' Compensation Board's website. If the designated contact is not available, that must be indicated on the form to avoid a denial based on submission errors.
What happens if the insurer does not respond to the C-4 form within 30 days?
If the insurer fails to respond within 30 calendar days (or 35 days if sent via mail with return receipt requested), the requested medical services will be deemed authorized. This means the attending physician may proceed with the treatment, without needing further approval from the insurer. It’s crucial for patients and providers to keep track of submission dates to ensure compliance with these timelines.
What should I do if the authorization request is denied?
If the authorization request for the services is denied, the denial must be accompanied by a conflicting medical opinion provided by an authorized physician. This second opinion should specifically address the medical necessity of the proposed services. If the request is denied based on the claimant's non-compliance—such as not attending a scheduled Independent Medical Examination (IME)—that evidence must be attached to the denial to clarify the rationale behind the insurer's decision.
Common mistakes
When filling out the Workers' Compensation C-4 form, one common mistake is failing to check the insurer's designated contact information. It is crucial to provide the correct name and fax number or email address listed on the Workers' Compensation Board's website. Omitting this information can lead to delays or denial of the request. Providers must ensure that they have the most current contact details before submitting the form.
Another frequent error is incomplete information in the authorization request section. This part of the form requires a clear explanation of the medical services being requested. Providers often neglect to detail every service or test, which can lead to confusion and potentially result in a denial. Ensuring that all services are specified can help streamline the authorization process.
Furthermore, some attendees overlook the need to establish medical necessity clearly. The Statement of Medical Necessity is a critical component that must provide adequate justification for the requested services. If this section is vague or lacks sufficient detail, it might delay the authorization process or prompt a request for additional information.
Additionally, failing to submit the form through the appropriate channels is a common mistake. The C-4 form must be sent to the insurer's designated contact via fax, email, or regular mail. If the request goes to the wrong contact, it could lead to unnecessary delays or a complete denial of authorization.
Lastly, neglecting to keep records of the submission can pose a challenge. It's important to document the date of submission and the method used to send the form. This information can be vital in follow-ups. If there is a need to prove that the request was made in a timely manner, having a record will save effort and confusion. Proper documentation supports the claim and helps ensure a smooth authorization process.
Documents used along the form
The Workers Compensation C-4 form is crucial for requesting authorization for special medical services. However, several other documents often accompany this form during the authorization process. Here are four essential documents used in conjunction with the C-4 form.
- WCB Form C-3: This is the Employee Claim Form. It details the employee's injury, including how it happened and when. It serves as the initial claim and helps the insurer understand the context of the injury.
- WCB Form C-2: The Employer's Report of Work-Related Injury. This form is completed by the employer to provide their perspective on the injury. It includes information about the employee's job duties and the circumstances surrounding the incident.
- WCB Form C-8: This is the Notice of Compensation Payable. It is issued by the insurer to inform the employee about the approval of their claim and the compensation awarded. The form helps clarify the benefits the injured party can expect.
- WCB Form M-1: The Medical Treatment Guidelines. This document outlines the standards for medical treatments approved for workers' compensation cases. It aids healthcare providers in understanding what services require pre-authorization.
Understanding these accompanying forms can facilitate a smoother workers' compensation process. Each plays a pivotal role in ensuring that injured workers receive the necessary support and that all parties have accurate information.
Similar forms
- Form C-3: This form is a claim for workers' compensation benefits. Like the C-4 form, it collects detailed information about the employee’s injury and medical treatment history, serving as a critical part of the claims process.
- Form C-5: The C-5 requests for medical treatment authorization. Similar to the C-4, it seeks approval for medical services, ensuring that necessary treatments receive timely funding.
- Form C-7: This form appeals a denial for benefits or medical services. Much like the C-4, it demands thorough documentation of support for the request, showcasing the need for transparency in the claims process.
- Form C-8: It requests a change in medical provider. Similar to the C-4, it requires justification for the request, ensuring that the insurer verifies the new provider's qualifications and appropriateness.
- Form C-11: This form serves as a notice of change in a claimant's condition. It's akin to the C-4 in that it communicates essential updates to the insurer regarding the medical situation of the claimant.
- Form C-28: This is used to report a change in a claimant's employment status. Similar to the C-4, it informs the insurer of significant developments that impact the ongoing claim.
- Form C-257: It requests reimbursement for medical expenses. Comparable to the C-4, this form emphasizes the need for proper documentation and clear lines of communication between the claimant and the insurer.
Dos and Don'ts
When filling out the Workers Compensation C-4 form, there are several important guidelines to follow. Below is a list of ten dos and don’ts to ensure the process runs smoothly.
- Do provide the full name and contact information for the insurer's designated contact.
- Don’t leave any questions unanswered on the form. Filling out all sections thoroughly is crucial.
- Do ensure that the form is signed by the attending doctor, including any required authorization numbers.
- Don’t use this form for specific injuries that require different documentation, such as those involving the back or neck.
- Do request written authorization for services costing over $1,000 in a timely manner.
- Don’t send the form to the wrong contact. Always verify the insurer’s designated contact information.
- Do attach supporting medical documents to the form if needed, especially for the statement of medical necessity.
- Don’t forget to keep copies of the submitted form for your records.
- Do submit the form via the recommended method: fax, email, or certified mail.
- Don’t ignore the deadlines for responses; timely follow-ups can prevent delays in authorization.
Misconceptions
Understanding the Workers Compensation C 4 form is crucial, yet many misconceptions often lead to confusion. Here’s a comprehensive list of common misunderstandings regarding this important document:
- Misconception 1: The C 4 form is only for serious injuries.
- Misconception 2: All medical requests must be made using this form.
- Misconception 3: Submitting the form guarantees approval for requested services.
- Misconception 4: Authorization without prejudice means the insurer accepts the claim.
- Misconception 5: A verbal agreement with the insurer is sufficient authorization.
- Misconception 6: Only the attending doctor can submit the C 4 form.
- Misconception 7: Waiting for a response is necessary before treatment can begin.
- Misconception 8: The form can be sent to any fax or email address.
- Misconception 9: A signature from the treating physician is unnecessary.
- Misconception 10: All medical procedures require prior authorization.
This form is not limited to severe injuries. It applies to any injuries or illnesses requiring treatment over $1,000 or pre-authorization, regardless of severity.
Not every medical request requires the C 4 form. It is specifically for "special services" that exceed $1,000 or necessitate prior approval according to Medical Treatment Guidelines.
Submitting the C 4 form does not assure authorization. Approval is contingent upon the insurer’s review and determination of medical necessity.
Authorization "without prejudice" indicates that the case's liability is not yet confirmed. It does not imply the insurer accepts responsibility for payment.
A verbal agreement does not fulfill the requirements. The written authorization must be formalized through the completion and submission of the C 4 form.
While it's typically the attending doctor’s responsibility, other authorized healthcare providers may also submit it, provided they meet specific identification requirements.
If no response occurs within 30 days (or 35 days if mailed), the treatment is deemed authorized, and the doctor can proceed.
The C 4 form must be sent to the insurer or self-insurer's designated contact listed on the Workers' Compensation Board's website to avoid denial of the request.
The form must be signed by the attending doctor and include their authorization number. This signature validates the request.
Emergency procedures do not require prior authorization using the C 4 form. The form is specifically designed for non-emergency situations involving significant costs.
Clarifying these misconceptions can help streamline the process for both providers and patients, ensuring that necessary treatments proceed without unnecessary delays.
Key takeaways
Filling out the Workers Compensation C-4 form can be a straightforward process, but there are several important points to keep in mind. Here are some key takeaways to help you navigate this essential documentation.
- Use Accurate Contact Information: Ensure you have the proper email address or fax number for the insurer's designated contact. This information can be found on the Workers’ Compensation Board’s website.
- Complete All Sections: Fill out every section of the form completely and accurately. Missing information can lead to delays or denials.
- Authorization for Special Services: This form is specifically for requesting authorization for special services that cost over $1,000 or require pre-authorization as defined by the Medical Treatment Guidelines.
- Emergency Situations: Remember, authorization isn't needed in an emergency. You can treat the patient without waiting for the go-ahead.
- Medical Necessity: Clearly explain the medical necessity for the requested services. This is crucial to avoid delays in the approval process.
- Timely Submission: Submit the completed form on the same day it’s filled out. Send it to both the Workers’ Compensation Board and the insurer or self-insured employer.
- Response Timeframe: Insurers have 30 days to respond to your request. If they fail to do so, you are authorized to proceed with the treatment.
- Denial Procedures: Should the insurer deny your request, they must provide conflicting medical evidence. Ensure you attach any necessary documentation for a solid appeal.
- Importance of Retaining Copies: Keep copies of the submitted form for your records. This is important in case you need to reference it later.
By following these guidelines, you'll be better prepared to navigate the workers' compensation claims process. Good luck!
Browse Other Templates
Affidavit Template California - Potential personal liability for debts is noted in the affidavit instructions.
8190 Nalc - Keeping records of all communications is advisable for both the employee and the management.
Wildlife Removal Hammond La - Permitted NWCOs may need to utilize different techniques depending on the species encountered.