Fill Out Your Wyoming Medicaid Edi Application Form
The Wyoming Medicaid EDI Application form serves as a crucial tool for healthcare providers seeking to enroll in electronic data interchange (EDI) with Wyoming Medicaid. Completing this form accurately is essential, as any incomplete sections may delay approval. Providers must fill in their business or provider name and physical address, along with pertinent contact information. Each application also requires a primary phone number, EDI contact details, and a Tax ID. If a provider wishes to access electronic remittance data through the 835 Health Care Claim Payment/Advice, they need to indicate their preference on the form, choosing whether they or a third party will retrieve these files. Critical instructions urge applicants to provide original signatures and complete all fields in ink. Upon submission, applicants will gain access to the Wyoming EqualityCare Secure Web Portal, where they can manage their claims and payments electronically. This process not only streamlines operations for providers but also enhances the accuracy and speed of reimbursements from Wyoming Medicaid.
Wyoming Medicaid Edi Application Example
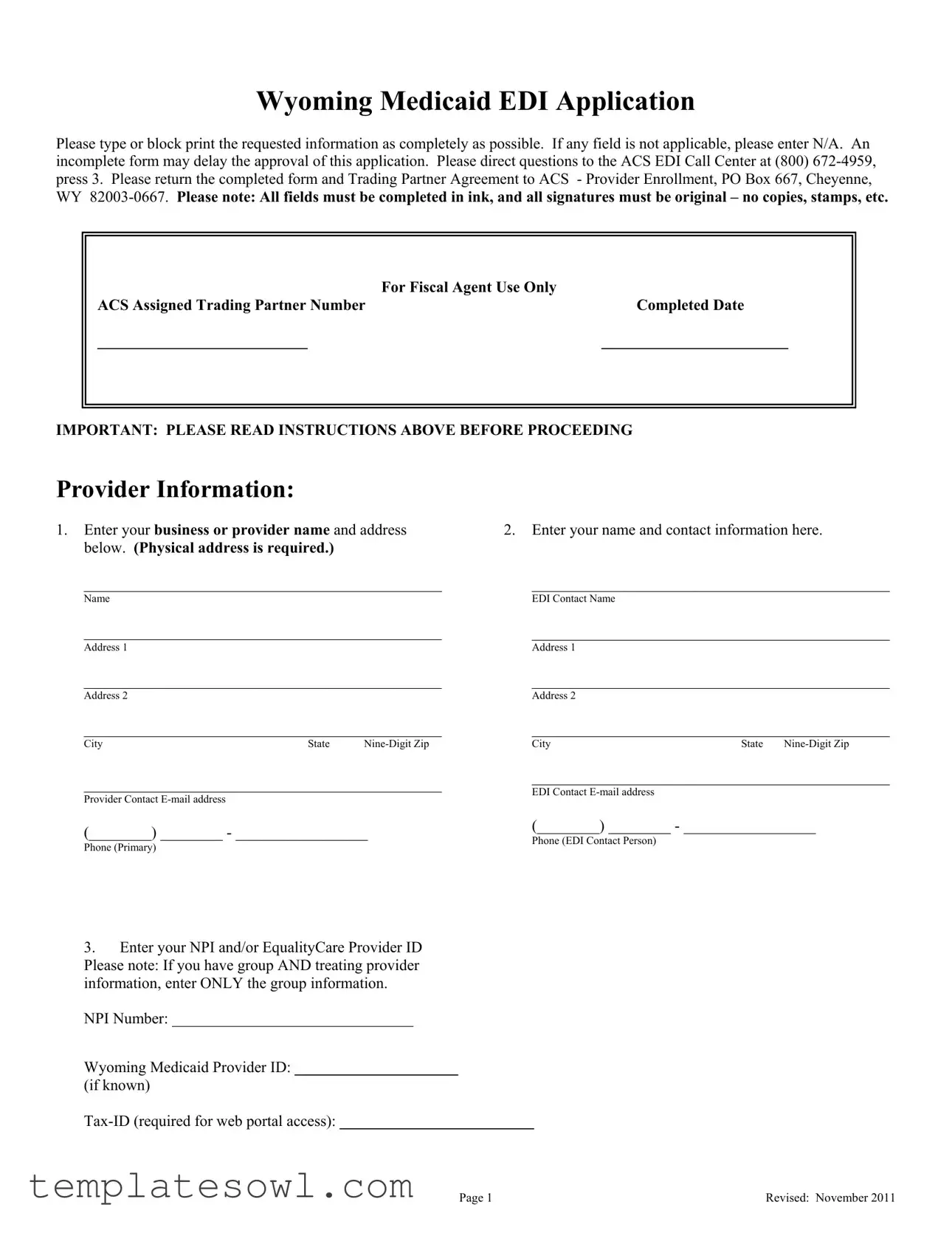
Wyoming Medicaid EDI Application
Please type or block print the requested information as completely as possible. If any field is not applicable, please enter N/A. An incomplete form may delay the approval of this application. Please direct questions to the ACS EDI Call Center at (800)
|
For Fiscal Agent Use Only |
ACS Assigned Trading Partner Number |
Completed Date |
___________________________ |
________________________ |
IMPORTANT: PLEASE READ INSTRUCTIONS ABOVE BEFORE PROCEEDING
Provider Information:
1.Enter your business or provider name and address below. (Physical address is required.)
______________________________________________
Name
______________________________________________
Address 1
______________________________________________
Address 2
______________________________________________
CityState
______________________________________________
Provider Contact
(________) ________ - _________________
Phone (Primary)
3.Enter your NPI and/or EqualityCare Provider ID Please note: If you have group AND treating provider information, enter ONLY the group information.
NPI Number: _______________________________
Wyoming Medicaid Provider ID: _____________________
(if known)
2.Enter your name and contact information here.
______________________________________________
EDI Contact Name
______________________________________________
Address 1
______________________________________________
Address 2
______________________________________________
CityState
______________________________________________
EDI Contact
(________) ________ - _________________
Phone (EDI Contact Person)
Page 1 |
Revised: November 2011 |
Remittance Advices and 835 Health Care Claim Payment files
By signing the provider agreement and returning this application, you will automatically be given access to the Wyoming EqualityCare Secure Web Portal and will be mailed an EDI Welcome Letter containing the necessary user information to register on the secure web portal, which will include access to Wyoming Medicaid’s Proprietary Remittance Advice. If you choose to make use of the 835 Health Care Claim
Payment/Advice, you will no longer receive copies of these Remittance Advices through postal mail, and will be directed to retrieve them through the Secure Web Portal.
1. The 835 Health Care Claim Payment/Advice is the electronic transmission of remittance data from Wyoming Medicaid to a provider (or clearinghouse). This remittance data is often referred to as an EOB (Explanation of Benefits). It is used to reconcile a payment against the claims a provider submitted to Wyoming Medicaid. To use the 835 Health Care Claim Payment/Advice requires special computer software capable of processing it.
Will you or a third party use the 835 Health Care Claim Payment/Advice? Please note – the 835 can only be delivered to a single trading partner number – i.e. either the clearinghouse OR the provider, but not both, can retrieve the 835 file. Regardless of where the 835 file is being delivered, Wyoming Medicaid’s Proprietary Remittance Advice will continue to be available via the Secure Web Portal to the provider.
I will retrieve my 835 (deliver to the Secure Web Portal and stop my mailed paper remittance advices)
A third party (e.g., clearinghouse) will retrieve my 835 (deliver to the
(trading partner of
I do not wish to use the 835 at this time (I wish to continue receiving mailed paper remittance advices. I am aware that in the future there may be a cost associated with this selection).
OR
My 835 files are ALREADY being delivered to trading partner ____________________________ and I wish to stop the delivery
(trading partner name and number)
to this trading partner number and begin the delivery to a new trading partner number ____________________________,
(trading partner name and number)
effective ____________________.
(date change is effective)
Page 2 |
Revised: November 2011 |
Claims and other Transactions
1.If you or your organization is already billing claims electronically to Wyoming Medicaid, enter your
2.If you are not already submitting your claims or other HIPAA 5010 transactions electronically but wish to OR need to update your submission information, indicate how you would like to submit:
Billing Agent
-Billing Agent Trading Partner ID: ____________________
Clearinghouse
-Clearinghouse Trading Partner ID: ___________________
Vendor Supplied Software
-Vendor Software Trading Partner ID: _________________
Secure Web Portal (free
-
WINASAP Billing Software (free
-Download the software from
Agreement
1.Complete the attached Trading Partner Agreement form.
Return By Mail To:
ACS – Provider Enrollment
PO Box 667
Cheyenne, WY
Page 3 |
Revised: November 2011 |
ACS EDI GATEWAY, INC.
TRADING PARTNER AGREEMENT
THIS TRADING PARTNER AGREEMENT (“Agreement”) is by and between SUBMITTER (“Submitter”), and ACS EDI Gateway, Inc. ("Trading Partner”), collectively “the Parties.”
Whereas, Submitter desires to transmit Transactions to Trading Partner for the purpose of submitting data to a Health Plan;
Whereas, Trading Partner desires to receive such Transactions for this purpose recognizing that Trading Partner performs such services on behalf of the Health Plan; and
Whereas, Submitter is subject to the Transaction and Code Set Regulations with respect to the transmission of such Transactions.
Now, therefore, the Parties agree as follows:
1.Definitions
Trading Partner means ACS EDI Gateway, Inc.
Submitter means the party identified as “Submitter” on the signature line of this Agreement who is a Health Care Provider as defined in 45 CFR 164.103.
Standard is defined in 45 CFR 160.103. Transaction is defined in 45 CFR 160.103.
Transactions and Code Set Regulations means those regulations governing the transmission of certain health claims transactions as published by DHHS under HIPAA.
2.Obligations of the Parties Effective Upon Execution of this Agreement by Submitter
A.The Parties agree, in regard to any electronic Transactions between them:
(1)They will exchange data electronically using only those Transaction types as selected by Submitter on the ACS EDI Gateway, Inc. Trading Partner Enrollment Form (TPEF).
(2)They will exchange data electronically using only those formats (versions) as specified on the TPEF.
(3)They will not change any definition, data condition, or use of a data element or segment in a Standard Transaction they exchange electronically.
(4)They will not add any data elements or segments to the Maximum Defined Data Set.
(5)They will not use any code or data elements that are not in or are marked as “Not Used” in a Standard’s implementation specification.
(6)They will not change the meaning or intent of a Standard’s implementation specification.
(7)Trading Partner may reject a Transaction submitted by Submitter if the Transaction is not submitted using the data elements, formats, or Transaction types set forth in the TPEF. Trading Partner may refuse to accept any claims from Submitter if Submitter repeatedly submits Transactions which do not meet the criteria set forth in a TPEF or if Submitter repeatedly submits inaccurate or incomplete Transactions to Trading Partner.
B.Submitter understands that Trading Partner or others may request an exception from the Transaction and Code Set Regulations from DHHS. If an exception is granted, Submitter will participate fully with Trading Partner in the testing, verification, and implementation of a modification to a Transaction affected by the change.
C.Trading Partner understands that DHHS may modify the Transaction and Code Set Regulations. Trading Partner will modify, test, verify, and implement all modifications or changes required by DHHS using a schedule mutually agreed upon by Submitter and Trading Partner.
D.Neither Submitter nor Trading Partner accepts responsibility for technical or operational difficulties that arise out of third party service
November 17, 2011 |
Page 1 |
providers’ business obligations and requirements that undermine Transaction exchange between Submitter and Trading Partner.
E. Submitter and Trading Partner will exercise diligence in protection of the identity, content, and improper access of business documents exchanged between the two parties. Submitter and Trading Partner will make reasonable efforts to protect the safety and security of individually assigned identification numbers that are contained in transmitted business documents and used to authenticate relationships between the parties.
F. Wyoming Medicaid may publish data clarifications (“Medicaid Provider Manuals”) to complement the ASC X12N Standards for Electronic Data Interchange Technical Report Type 3 (TR3). Submitter should use Medicaid Provider Manuals in conjunction with the TR3
documents available at
G. Transactions are considered properly received only after accessibility is established at the designated machine of the receiving party. Once transmissions are properly received, the receiving party will promptly transmit an electronic acknowledgment that conclusively constitutes evidence of properly received transactions. Each party will subject information to a virus check before transmission to the other party.
H. Each party will implement and maintain appropriate policies and procedures and mechanisms to protect the confidentiality and security of PHI transmitted between the parties.
3.Miscellaneous
A.This Agreement is effective on the date last signed below. This Agreement shall continue until such time as either party elects to give written notice of termination to the other party or termination of Transaction services provided by Trading Partner to Submitter, whichever is earlier.
B.This Agreement incorporates, by reference, any written agreements between the parties relating to the subject matter hereof.
C.This Agreement shall be interpreted consistently with all applicable federal and state privacy laws. In the event of a conflict between applicable laws, the more stringent law shall be applied. This Agreement and all disputes arising from or relating in any way to the subject matter of this Agreement shall be governed by and construed in accordance with Florida law, exclusive of conflicts of law principles. THE EXCLUSIVE JURISDICTION FOR ANY LEGAL
PROCEEDING REGARDING THIS AGREEMENT SHALL BE IN THE COURTS OF THE STATE OF FLORIDA AND THE PARTIES HEREBY EXPRESSLY SUBMIT TO SUCH JURISDICTION.
D.Unless otherwise prohibited by statute, the parties agree that this Agreement shall not be affected by any state’s enactment or adoption of the Uniform Computer Information Transaction Act, Electronic Signature or any other similar state or federal law. Each party agrees to comply with all other applicable state and federal laws in carrying out its responsibilities under this Agreement.
E.This Agreement is entered into solely between, and may be enforced only by, Submitter and Trading Partner. This Agreement shall not be deemed to create any rights in third parties or to create any obligations of Submitter or Trading Partner to any third party.
F.NO WARRANTIES, EXPRESS OR IMPLIED, ARE PROVIDED BY TRADING PARTNER UNDER THIS AGREEMENT. TRADING PARTNER’S MAXIMUM AGGREGATE LIABILITY FOR DAMAGES FOR ANY AND ALL CAUSES WHATSOEVER ARISING OUT OF THIS AGREEMENT, REGARDLESS OF THE MANNER IN WHICH CLAIMED OR THE FORM OF ACTION ALLEGED, IS LIMITED TO THE AMOUNT(S) PAID TO TRADING PARTNER BY SUBMITTER UNDER THIS AGREEMENT.
November 17, 2011 |
Page 2 |
G. Trading Partner may provide proprietary software to Submitter to allow Submitter to submit Transactions to Trading Partner. Submitter will protect the software as it protects its own confidential information and will not, directly or indirectly, allow access to or the use of the software or any portion thereof, on any computer, server, or network, by any person, corporation, or business entity other than Submitter. Submitter may permit use of the software by contractors or agents of Submitter provided that any such contractors or agents are not competitors of Trading Partner and further provided that any such persons agree to protect the confidentiality of the software. Submitter and its contractors and agents are not permitted to use the software for any purpose other than submitting Transactions solely to Trading Partner.
H. Agreement contains the entire agreement between the parties and may only be modified by an agreement signed by both parties.
I.Submitter may elect to execute either a hard copy or an electronic copy of this Agreement. Hard Copy Execution: Submitter will sign a hard copy of this Agreement and mail to Trading Partner at the address indicated below. Trading Partner will return a copy of the fully executed Agreement to Submitter. The effective date of the hard copy Agreement is the date on which the Agreement is signed by Trading Partner. Electronic Copy Execution: Submitter should execute this Agreement by clicking on the “I AGREE” button that appears at the bottom of the Agreement. The effective date of the electronic copy agreement is the date Trading Partner receives the electronic transmission of Submitter’s acceptance to the terms of this Agreement.
SUBMITTER:
Provider Number/Trading Partner ID
Signature
Printed Name and Title
Date
Mail Completed Agreement To:
ACS EDI
Attention: EDI Enrollment
PO Box 667
Cheyenne, WY 82003
For ACS EDI Enrollment Use Only:
Signature
Printed Name and Title
Date
November 17, 2011 |
Page 3 |
Form Characteristics
| Fact Name | Description |
|---|---|
| Application Completeness | All fields in the Wyoming Medicaid EDI Application form must be completed in ink. Incomplete applications may delay processing. |
| Submission Address | Completed forms and the Trading Partner Agreement should be sent to ACS - Provider Enrollment, PO Box 667, Cheyenne, WY 82003-0667. |
| Provider Access | By signing the provider agreement, users gain access to the Wyoming EqualityCare Secure Web Portal and receive an EDI Welcome Letter with registration details. |
| Governing Laws | This application complies with HIPAA regulations as well as Wyoming state laws governing Medicaid services. |
Guidelines on Utilizing Wyoming Medicaid Edi Application
Upon completing the Wyoming Medicaid EDI Application form, you will be able to submit it to the appropriate authorities for processing. It is important to ensure that all required fields are filled out accurately and completely to avoid any delays in your application. After submitting the form along with the Trading Partner Agreement, you may expect to receive further instructions on how to access the Wyoming EqualityCare Secure Web Portal.
- Obtain the Form: Start by obtaining the Wyoming Medicaid EDI Application form, ensuring that you have the most recent version.
- Provider Information: In the designated section, enter your business or provider name, physical address, and contact information. Include the city, state, and nine-digit ZIP code.
- Contact Details: Provide the name of your EDI contact person along with their email address and phone number. Be sure to include the complete Tax-ID, as it is necessary for web portal access.
- NPI and EqualityCare Provider ID: If applicable, enter your NPI (National Provider Identifier) and/or the Wyoming Medicaid Provider ID. If you only have group information, only provide that.
- 835 Health Care Claim Payment Files: Respond to whether you or a third party will use the 835 files. Make sure to indicate your choice clearly on the application.
- Claims Submission: If you are already billing claims electronically, provide your current Submitter or Trading Partner ID. If not, select how you wish to submit your claims, indicating the applicable IDs for your chosen method.
- Completing the Agreement: Fill out the attached Trading Partner Agreement form. Ensure that all required signatures are included; original signatures are mandatory.
- Returning the Application: Once completed, mail the form and the Trading Partner Agreement to the address specified: ACS – Provider Enrollment, PO Box 667, Cheyenne, WY 82003-0667.
What You Should Know About This Form
1. What is the purpose of the Wyoming Medicaid EDI Application form?
The Wyoming Medicaid EDI Application form is designed for healthcare providers who wish to electronically submit claims, access payment remittance data, and utilize the Wyoming EqualityCare Secure Web Portal. By completing this application, providers can streamline their billing processes and manage their patient claims more efficiently. This application grants access to necessary resources and ensures that all submissions meet Medicaid’s operational standards.
2. What information is required to complete the application?
To successfully complete the Wyoming Medicaid EDI Application, it is essential to provide detailed information regarding the provider's business or personal identifying details. This includes the provider's name, address, and contact information, as well as the necessary identification numbers such as the NPI number and Wyoming Medicaid Provider ID, if known. Additional contact details for an EDI representative should also be included. Each field in the application must be filled out completely and accurately, as omissions may lead to delays in processing the application.
3. Why is it important to submit the application in ink?
Submitting the Wyoming Medicaid EDI Application in ink ensures that all information provided is legible and permanent. Handwritten submissions are less likely to experience issues with readability compared to typed forms. Moreover, Medicaid mandates that signatures on the application must be original; thus, electronic copies, stamps, or facsimiles are not accepted. Adhering to this requirement helps avoid any potential complications that may arise from incomplete or unclear information.
4. What is the 835 Health Care Claim Payment/Advice, and how does it work?
The 835 Health Care Claim Payment/Advice is an electronic document that details the payment remittance data from Wyoming Medicaid to providers or their designated clearinghouses. This document allows providers to reconcile payments with the claims they have submitted. Providers can opt to retrieve their 835 files through the Secure Web Portal, thus eliminating the need to receive paper remittance advices in the mail. It is important to note that only one trading partner can access the 835 files at a time, which requires choosing between the provider or a third-party clearinghouse.
5. What steps should be taken if a provider wants to make changes to their EDI submissions?
If a provider needs to update their EDI submissions, they must indicate their preferred method of submission on the application form. This may include using a billing agent, a clearinghouse, vendor software, or the free Secure Web Portal. If changes involve halting the delivery of 835 files to one trading partner and redirecting them to another, the provider should carefully fill in the relevant sections to ensure a smooth transition. Following these steps helps maintain accurate and efficient communication with Medicaid.
Common mistakes
Filling out the Wyoming Medicaid EDI Application form can be a straightforward process, but some common mistakes can cause delays or complications. One of the most frequent errors is leaving fields incomplete. Every section must have information filled out. If a question does not apply, using "N/A" is essential. Incomplete forms can significantly slow down the approval process, meaning applicants could face unnecessary waiting times for access to necessary services.
Another mistake occurs when applicants provide incorrect or outdated information. This often happens with contact details such as phone numbers, email addresses, or the business address. It’s vital to double-check that everything entered is accurate and current. Simply missing a digit in a phone number or a misspelled email can prevent communication, leading to delays or the rejection of the application.
Not gathering and submitting required documentation is also a major pitfall. Individuals sometimes forget to include their Trading Partner Agreement or fail to provide their NPI and Tax ID as specified. Missing these documents can halt the processing of the application. Take the time to ensure all necessary paperwork is included before submission.
Finally, neglecting to sign the application in the required manner is a serious oversight. All signatures must be original. Using copies, stamps, or electronic signatures can result in automatic rejection of the form. Ensuring that all required signatures are in ink and authentic will save time and avoid complications during the review of the application.
Documents used along the form
The Wyoming Medicaid EDI Application form is a key document for providers seeking electronic data interchange (EDI) services. Along with this form, several additional documents are typically required or recommended to facilitate the enrollment process and ensure compliance with applicable regulations. Below are other important forms and documents often used in conjunction with the Wyoming Medicaid EDI Application.
- Trading Partner Agreement: This agreement establishes the terms between the submitter (provider) and the trading partner (ACS EDI Gateway, Inc.). It encompasses the exchange of electronic transactions and the responsibilities each party holds in the process.
- NPI (National Provider Identifier): This unique identification number is essential for all healthcare providers. It is used to identify providers in a standardized way and is typically required on billing claims and other healthcare documentation.
- Provider Enrollment Application: This application collects essential information from providers looking to enroll in the Wyoming Medicaid program. It includes details about the provider's business structure and services offered.
- Tax Identification Number (TIN): A TIN or Employer Identification Number (EIN) may be required for tax reporting purposes. This number helps distinguish the entity for taxation and billing activities.
- HIPAA Compliance Documentation: Proof that the provider complies with the Health Insurance Portability and Accountability Act. This may involve detailing policies and procedures to protect patient information and ensure secure electronic transactions.
- Claim Submission Protocols: These documents outline the procedures for submitting claims electronically. They typically include guidelines for formatting and submitting claims to ensure they are processed smoothly.
- Software and Technology Requirements: Documentation specifying the technology needs for electronic submissions, including any software necessary to submit claims and receive payments electronically.
- State-Specific Medicaid Policies: Manuals or resources that provide guidance on the Medicaid program specific to Wyoming. They include regulations, billing procedures, and other essential information for Medicaid providers.
- EDI Enrollment Confirmation: A document confirming the successful enrollment in the EDI system once the Wyoming Medicaid EDI Application and associated forms are processed.
These documents serve to streamline the enrollment process, ensure compliance, and clarify responsibilities among all parties involved. Providers should ensure they complete and submit all necessary documentation to facilitate prompt processing and avoid delays in receiving Medicaid services and payments.
Similar forms
Trading Partner Agreement: Similar to the Wyoming Medicaid EDI Application form, the Trading Partner Agreement outlines the responsibilities and expectations between parties involved in electronic transactions. Both documents are designed to ensure that critical information is exchanged accurately and efficiently while maintaining compliance with regulations.
EDI Enrollment Form: The EDI Enrollment Form serves as a registration document that collects essential details from healthcare providers who wish to participate in electronic data interchange. Much like the Medicaid EDI Application, it requires specific provider information and highlights the importance of accurate data entry to avoid delays in processing.
Authorization Agreement: This document grants permission for the electronic submission of claims and sensitive information. Similar to the Medicaid EDI Application, it ensures that all parties involved understand their roles and the procedures they must follow to protect personal health information and comply with regulations.
Claims Submission Form: The Claims Submission Form allows healthcare providers to submit billing information for services rendered to Medicaid. Just like the Medicaid EDI Application, it emphasizes the necessity of complete and correct data. In both cases, thorough documentation helps streamline the reimbursement process and reduce claims denials.
Dos and Don'ts
When filling out the Wyoming Medicaid EDI Application form, it's important to be both thorough and careful. Here’s a list of things to do and avoid:
- Do type or print your information clearly and completely to avoid delays in processing.
- Do fill in any fields that do not apply to you with "N/A" to indicate they are not applicable.
- Do use blue or black ink for all handwritten entries to ensure legibility.
- Do ensure that all signatures are original; do not use copies or stamps.
- Do send the completed application and Trading Partner Agreement to the correct address: ACS - Provider Enrollment, PO Box 667, Cheyenne, WY 82003-0667.
- Don't leave any fields blank, as an incomplete form will delay the approval process.
- Don't forget to provide a physical address; this is a required field.
- Don't use any third-party applications or services unless you have indicated it on the form.
- Don't assume you can make changes after submission; check everything before sending.
- Don't forget to direct any questions to the ACS EDI Call Center at (800) 672-4959, press 3 for assistance.
Misconceptions
The Wyoming Medicaid EDI Application form comes with a number of misconceptions that can cause confusion among applicants. The following list addresses these common misunderstandings:
- The form can be filled out in pencil or typed: Many people assume they can use any writing method. However, it is essential to complete the form in ink only.
- All fields are optional: Some applicants think that fields not applicable to them can be left blank. In reality, every field must be filled out, and if not applicable, use "N/A."
- Forms can be submitted without original signatures: It's a common error to believe copies or stamped signatures are acceptable. All signatures must be original for the application to be valid.
- The EDI Welcome Letter is sent immediately: Many people expect to receive their EDI Welcome Letter as soon as they submit their application. The letter will be sent after the application is processed.
- Delivery options for the 835 files are flexible: Some applicants think they can receive the 835 files delivered to multiple parties. Deliveries are limited to one trading partner number only.
- The application process is quick and easy: While the form itself may seem straightforward, incomplete submissions can significantly delay the approval process.
- Using the 835 file requires special training: It is a misconception that extensive training or software is always necessary. While certain software is required to process 835 files, assistance is available for those who need it.
- The form is only for new providers: Existing providers might think the EDI Application is irrelevant to them. In fact, this form can also be used for updating existing information, such as contact details or billing setups.
Understanding these misconceptions can help ensure a smoother application process and avoid unnecessary delays. If you have concerns, don't hesitate to reach out to the ACS EDI Call Center for assistance.
Key takeaways
Filling out the Wyoming Medicaid EDI Application form is an important process. Here are key takeaways to consider:
- Complete All Fields: Ensure that every field of the application is filled out completely. Write in ink and make sure all signatures are original.
- Use Accurate Information: Provide precise details for your business or provider name, address, and contact information. An incomplete form can lead to delays in processing.
- Contact Information: Include your EDI contact’s information to facilitate communication. This will help if any issues arise during the approval process.
- Trading Partner Agreement: Complete and send the Trading Partner Agreement along with your application. This is necessary for registration.
- 835 Health Care Claim Payment: If you opt for the 835 electronic remittance, ensure your software can process it. Decide whether you or a third party will retrieve the data.
- Claims Submission: Indicate how you'll submit claims electronically. Options include a billing agent, clearinghouse, or directly through the secure web portal.
- Mailing Instructions: After completion, mail the application and agreement to the specified address in Cheyenne, WY. Following instructions meticulously is crucial.
- Technical Requirements: Understand any technical requirements needed to successfully transmit transactions electronically. Familiarize yourself with the necessary software.
- Record Keeping: Maintain copies of all submitted forms and confirmations. This can be helpful for tracking and future reference.
These takeaways can streamline the application process and ensure a smooth experience with Wyoming Medicaid.
Browse Other Templates
Can You File an Appeal After 30 Days - The defendant or respondent’s name is also required for accuracy.
Minor Employment Authorization,Youth Work Approval Form,Underage Work Certification,Apprentice Employment Application,Student Work Validation,Youth Labor Permit,Part-Time Employment Request,Minor Work Eligibility Application,Junior Worker Permission - The length and type of employment can directly impact the approval of the permit.